CRISPR/Cas9-Edited Autologous CD34 Cells: Advancing Therapy for β-Thalassemia Major
A novel therapeutic approach involves the use of genetically modified autologous hematopoietic stem cells (HSCs). Research has shown that elevated levels of fetal hemoglobin (HbF) can alleviate clinical symptoms in some β-thalassemia patients. The transcription factor BCL11A is a key repressor of γ-globin expression, which is a crucial component of HbF. A treatment called ET-01 is being developed, which edits autologous CD34+ cells using CRISPR/Cas9 technology to disrupt the BCL11A erythroid enhancer, thereby reactivating γ-globin expression and treating β-thalassemia.
The development of ET-01 has demonstrated high precision and efficiency in editing the BCL11A enhancer, leading to therapeutic levels of HbF. The manufacturing process has been scaled up under current Good Manufacturing Practice (cGMP) standards, and preclinical studies, including Good Laboratory Practice (GLP) studies with clinical-scale ET-01, are underway.
To enhance the BCL11A enhancer, Cas9 mRNA and synthetic sgRNA were introduced into CD34+ HSCs from both healthy and β0/β0 donors via electroporation. The gene editing efficiency was approximately 80% for both donor types. The in vitro erythroid differentiation efficiency was similar between ET-01 and unedited CD34+ HSCs. Both HbF+ cell levels and γ-globin mRNA levels were significantly increased in ET-01 compared to unedited cells. Notably, in ET-01 derived from β0/β0 donor cells, the combined levels of γ-globin and β-globin exceeded a threshold that could have a meaningful clinical impact.
Colony-forming unit assays indicated that the types and numbers of colonies were comparable between ET-01 and unedited CD34+ HSCs, suggesting no significant impact on colony-forming capability. To assess the specificity of the gene-editing method, a panel of 42 sites with the highest off-target editing probabilities was analyzed, showing no significant off-target events, indicating minimal off-target effects.
In vivo engraftment potential was evaluated by transplanting ET-01 and unedited CD34+ HSCs into immunodeficient NPG mice. Both cell types showed rapid and efficient engraftment, with similar multi-lineage reconstitution in various hematopoietic and immune organs. The Indels efficiencies remained similar in NPG mice after 4 months and after a second transplantation, indicating long-term hematopoietic repopulating and differentiation capabilities without tumorigenicity.
The ET-01 manufacturing process has been successfully scaled up, producing a large number of CD34+ HSCs from healthy donor leukopak. High cell viability, purity, and Indels frequencies were maintained throughout the process. Preclinical studies, including GLP studies with clinical-scale ET-01, are in progress.
How to Use Synapse Database to Search and Analyze Translational Medicine Data?
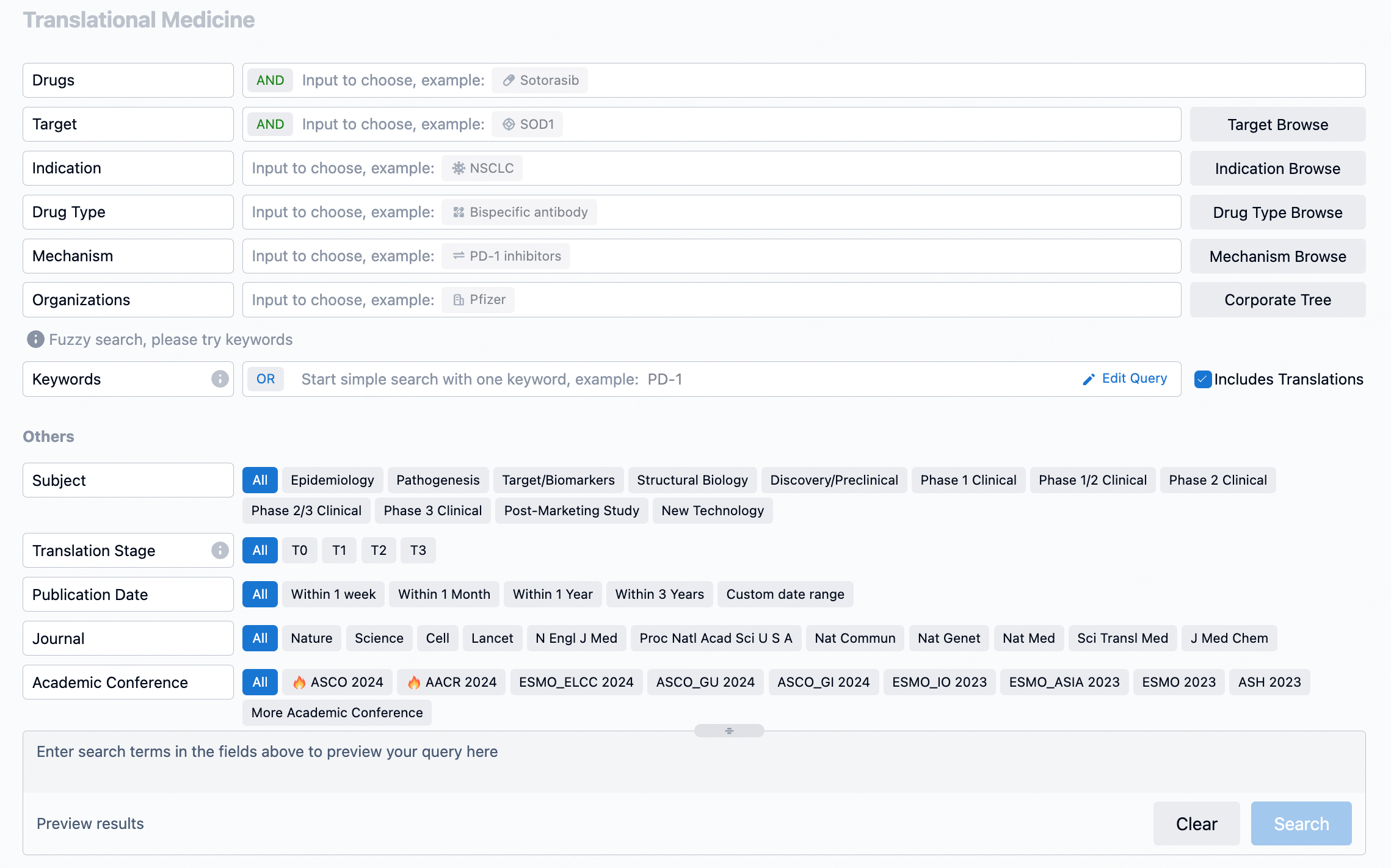
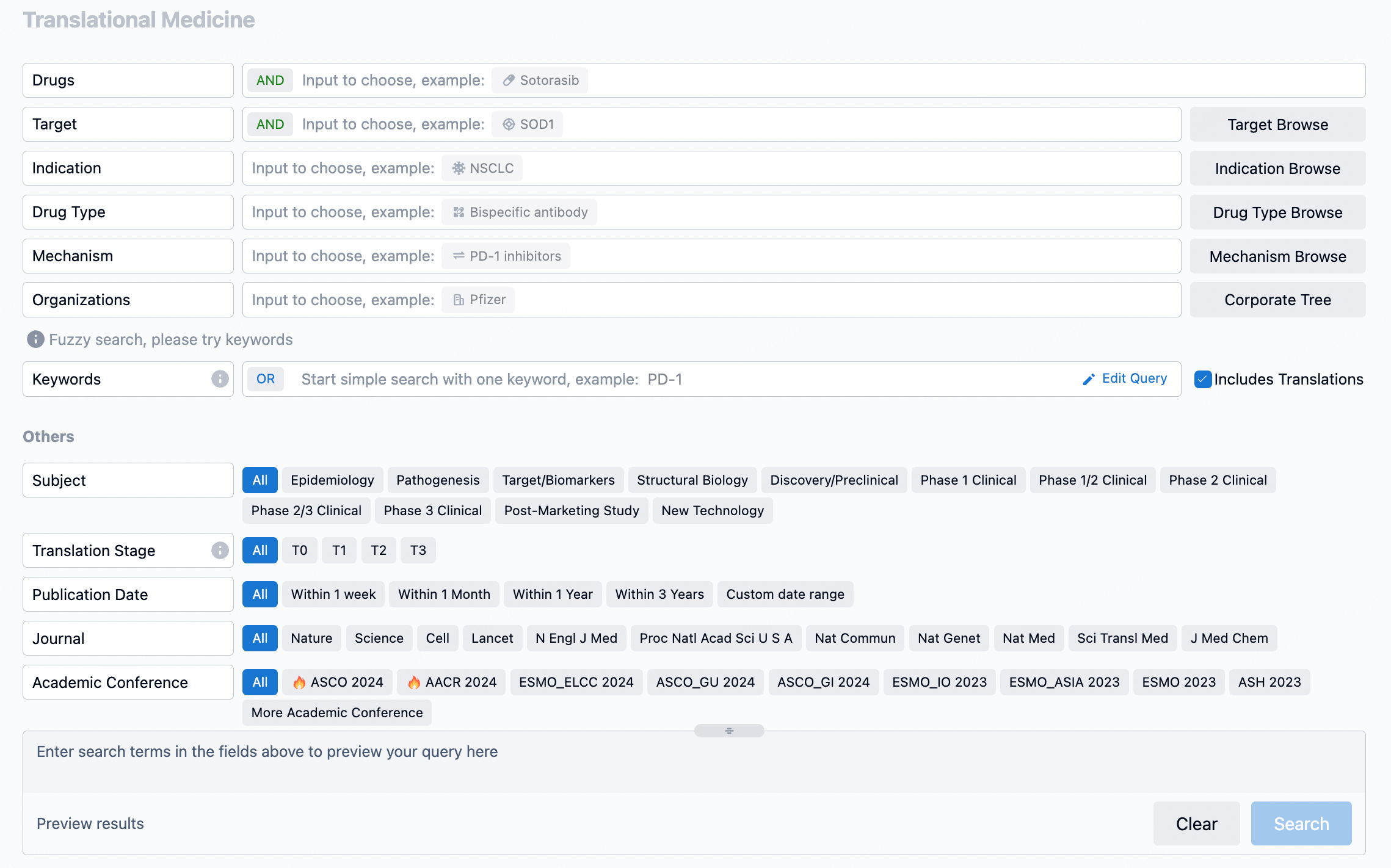
The transational medicine section of the Synapse database supports searches based on fields such as drug, target, and indication, covering the T0-T3 stages of translation. Additionally, it offers a historical conference search function as well as filtering options, view modes, translation services, and highlights summaries, providing you with a unique search experience.
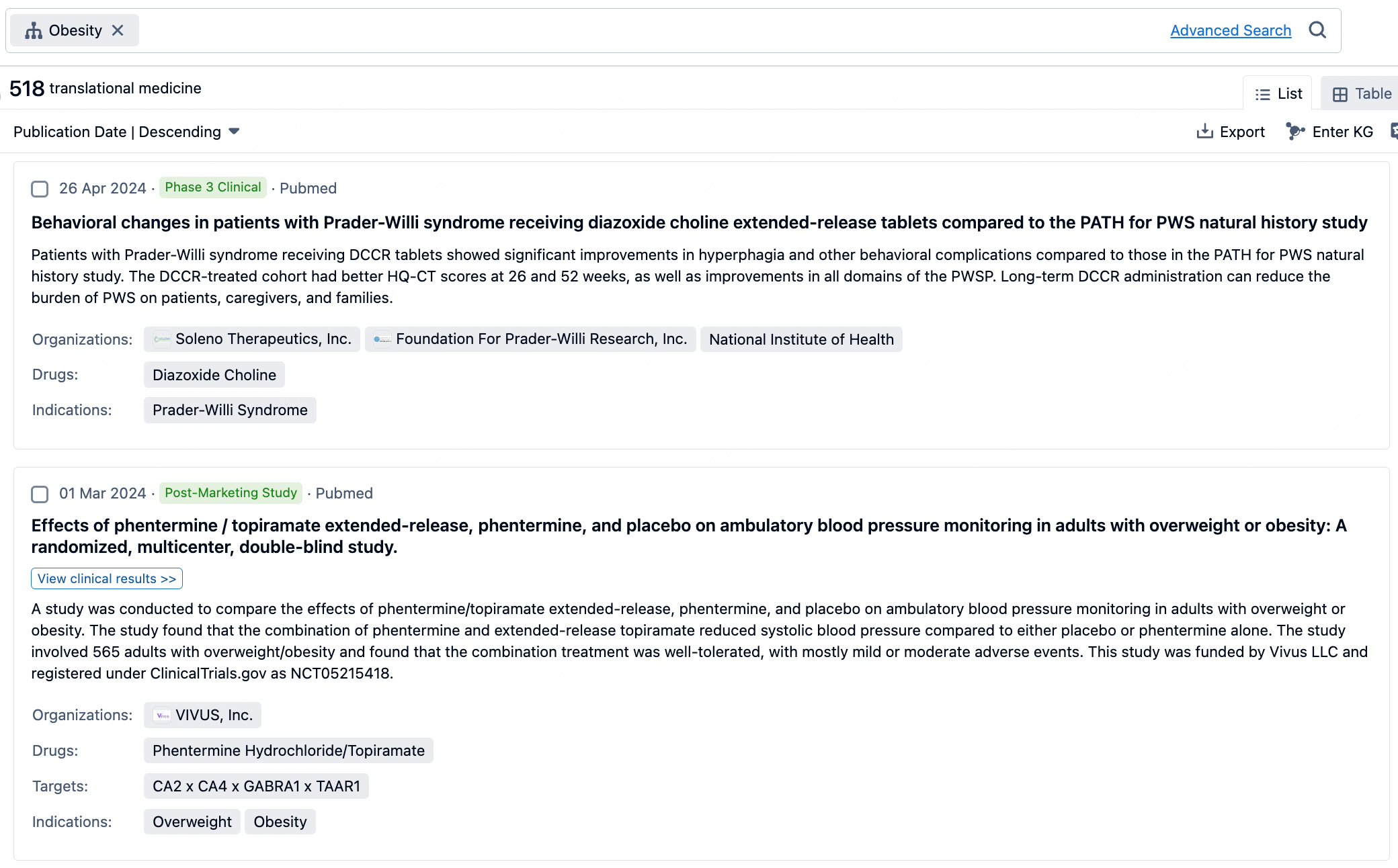
Taking obesity as an example, select "obesity" under the indication category and click search to enter the Translational Medicine results list page. By clicking on the title, you can directly navigate to the original page.
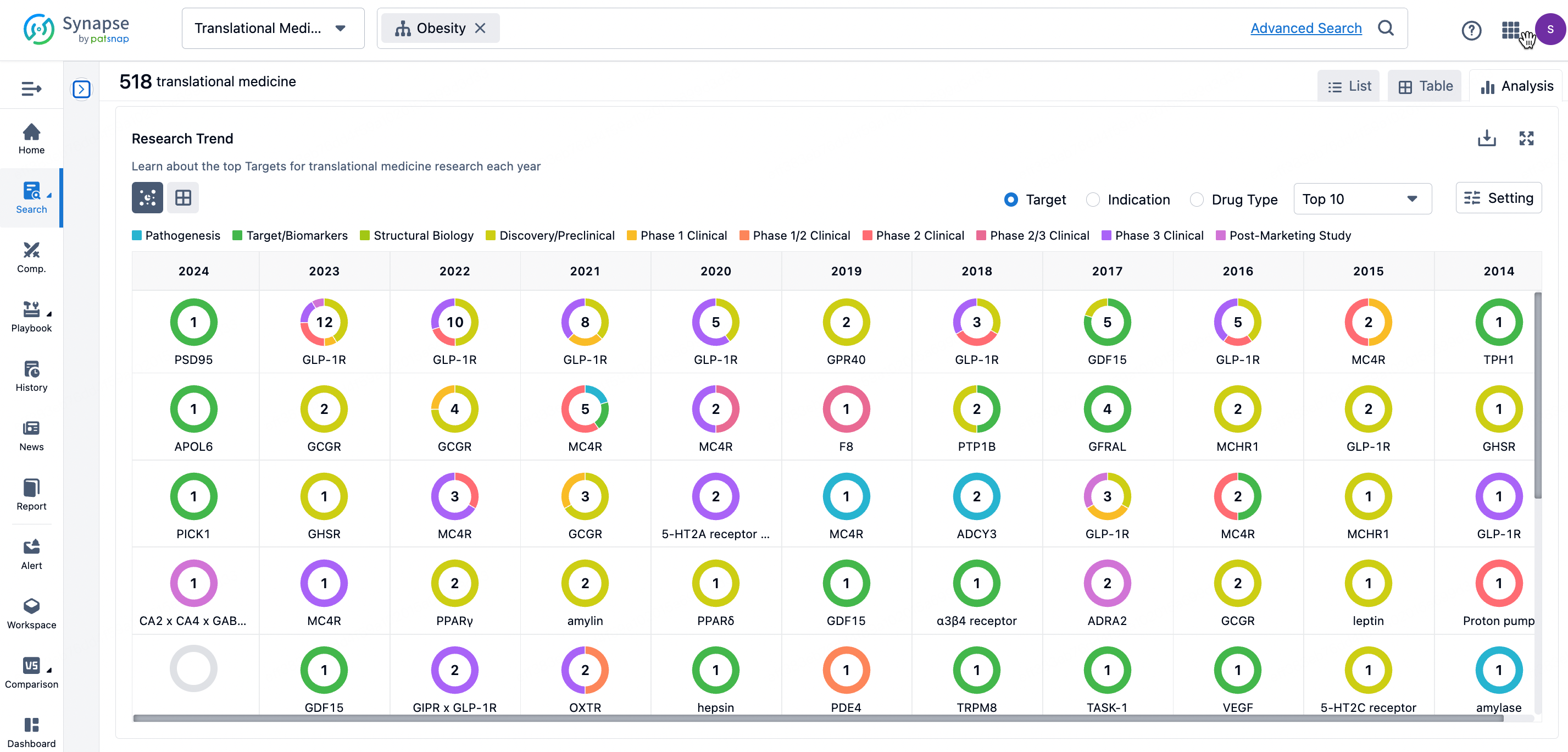
By clicking the analysis button, you can observe that GLP-1R treatment for obesity has gained significant attention over the past three years, with preclinical research still ongoing in 2023. Additionally, there are emerging potential targets, such as GDF15, among others.
Click on the image below to go directly to the Translational Medicine search interface.