Request Demo
For what indications are Shared antigen vaccine being investigated?
17 March 2025
Introduction to Shared Antigen Vaccines
Shared antigen vaccines are a category of therapeutic vaccines designed to target antigens that are commonly expressed among tumors or other disease‐affected tissues across different patients. These vaccines differ from personalized or neoantigen vaccines in that they exploit well‐characterized, “shared” molecular markers, which are expressed on multiple tumor types or in recurrent disease patterns. In essence, they leverage a “one-size-fits-all” antigen approach that can be applied across a broader spectrum of patients, primarily in oncology.
Definition and Basic Concepts
Shared antigen vaccines are formulated using antigens that are not unique to a single tumor but rather are expressed across a range of cancers. These antigens are often proteins or peptides that serve critical functions in tumor cell physiology and are recognized by the immune system. By targeting these targets, the vaccines aim to elicit a robust T-cell and antibody-mediated response against cancer cells. For example, Sipuleucel-T, which is based on a shared antigen strategy, utilizes immunostimulants to target prostate antigens and generate long-lasting immune responses. Similar approaches include vaccines that target HER2, NY-ESO-1, and PAP—each representing a shared antigen among particular groups of tumors. The core concept is to overcome the immunosuppressive tumor microenvironment by recognizing these relatively invariant antigens, which in many cases are essential for tumor survival and therefore less likely to be lost through mutation.
Overview of Vaccine Development
Vaccine development in the context of shared antigens has evolved through several generations. Initially, vaccines were based on whole pathogens or tumor cell lysates, which sometimes resulted in non-specific immune responses. Today, however, advances in recombinant DNA technology and improved antigen characterization have allowed vaccine developers to isolate specific epitopes responsible for immune recognition. Key to this advancement has been the integration of adjuvants and modern delivery platforms. Shared antigen vaccines have been designed using multiple antigen formats such as peptide vaccines, DNA vaccines, and immune cell therapies—all seeking to present the shared antigen effectively to antigen-presenting cells (APCs). The development pathway typically includes preclinical evaluations in animal models, followed by iterative clinical phases to assess safety, immunogenicity, and eventual clinical efficacy. Large-scale clinical trials, especially in oncology, are crucial to validate that these shared antigens can serve as effective targets for immunotherapy.
Investigational Indications for Shared Antigen Vaccines
Shared antigen vaccines are predominantly investigated in the field of oncology due to the need for treatments that address multiple cancer types simultaneously and overcome tumor immune evasion. That said, there are also exploratory studies looking at shared antigen concepts for infectious diseases. Here, we outline the investigational indications for these vaccines from both a general and specific perspective.
Cancer Indications
Cancer remains the primary indication for which shared antigen vaccines have been extensively investigated. The rationale is based on the observation that many malignancies express common tumor-associated antigens (TAAs) that can be exploited as targets for immunotherapy.
1. Prostate Cancer:
Sipuleucel-T, the first FDA-approved therapeutic cancer vaccine, is designed to treat metastatic castration-resistant prostate cancer and relies on the delivery of a shared antigen that stimulates an immune response against prostate tumor cells. Moreover, PAP vaccines, such as the one developed by Madison Vaccines, Inc., target prostatic acid phosphatase (PAP), a widely expressed antigen in prostate cancer. These vaccines work by activating dendritic cells which can then stimulate cytotoxic T lymphocytes to attack cells expressing PAP.
2. HER2-Expressing Cancers:
Several shared antigen vaccines specifically target the HER2 protein—a receptor overexpressed in a variety of cancers including breast, ovarian, and gastric carcinomas. Nelipepimut-S, for instance, is a shared antigen vaccine aimed at eliciting an immune response against HER2-positive tumor cells. Additionally, AE-37/GP-2, produced by Generex Biotechnology Corp., is another vaccine formulation that targets HER2 through shared antigen strategies. These vaccines have been examined in clinical trials to determine whether boosting immune responses against HER2 can reduce tumor burden and delay disease progression.
3. Broad Spectrum Neoplasms and Urogenital Cancers:
EP-2101, an investigational vaccine from IDM Pharma Inc., is currently in Phase 3 and targets a range of neoplasms, including those affecting respiratory, digestive, and urogenital systems. Similarly, OQR-200, developed by OncoQR ML GmbH, is in its preclinical stage and focuses on tumors within the neoplastic and urogenital disease groups. Furthermore, products like Oncoquest-PC, developed by Xeme Biopharma Inc., are intended for neoplasms with urogenital involvement even at an early preclinical phase.
4. Melanoma and Other Solid Tumors:
Although not exclusively reserved for melanoma, some shared antigen vaccines have shown promise in broader applications including skin and musculoskeletal cancers. For example, the vaccine strategies targeting HER2 or other shared antigens might benefit tumors in these sites by inducing targeted immune responses. Such strategies have also been investigated in combination with other immunotherapeutic modalities to enhance overall response rates.
5. Discontinued or Investigational Candidates:
Some shared antigen vaccine candidates, like the NY-ESO-1/LAGE-1 class I/II peptide vaccine developed at Baylor College of Medicine and VEGFR1 peptide vaccines from The University of Tokyo Hospital, although currently discontinued or not progressing in clinical trials, provide insight into the complex challenges associated with targeting shared antigens. Their clinical pathways highlight both the potential and the pitfalls in targeting widely expressed tumor antigens.
Collectively, these cancer indications demonstrate the diversity of tumor types that can potentially benefit from shared antigen vaccines. They are designed to harness the body’s immune system against tumors that share common molecular features, thereby providing a therapeutic option that could potentially be applied to a wide patient population.
Infectious Diseases
While the bulk of the current investigational data on shared antigen vaccines focuses on oncology, the concept is also applicable to infectious diseases. Shared antigen vaccines in infectious disease settings aim to target conserved epitopes across different strains of a pathogen. For example, influenza vaccines and universal coronavirus vaccines often seek to incorporate antigens that are conserved among the highly mutable strains of the viruses. Although the provided references do not include many examples of shared antigen vaccines explicitly developed for infectious diseases (most infectious disease vaccine references pertain to recombinant protein vaccines, viral vector vaccines, or combination vaccines), the principle remains similar.
1. Influenza Vaccines:
Some patents and research studies have described vaccines that incorporate influenza virus antigens harvested through improved purification methods to achieve high-purity virus antigen standards. These methods aim to identify shared viral antigens that remain conserved despite ongoing mutations. In such a scenario, the antigen design mimics the shared antigen strategy used in cancer vaccines but is oriented toward eliciting broad cross-protective immunity against multiple influenza strains.
2. Universal Coronavirus Vaccines:
The idea of developing a universal coronavirus vaccine—one that could provide broad immunity across variants—also leverages the concept of shared or conserved antigen targets. Recent research prioritizes identifying epitopes that are less likely to mutate (such as regions away from the mutable receptor-binding domain), thereby ensuring long-term efficacy. This parallels the strategy used in developing shared antigen vaccines for cancers, where maintaining immunogenicity despite tumor heterogeneity is a challenge.
3. Other Pathogens:
Similar approaches are being explored for other infectious agents such as tuberculosis, dengue, and even certain bacterial infections where antigen conservation across strains might be exploited. However, unlike cancer indications where the focus has been more pronounced, infectious disease applications are still evolving and may require combining adjuvants and more sophisticated delivery systems to overcome the inherent variability of pathogen antigens.
Overall, while the dominant research and clinical trial data on shared antigen vaccines derive from oncology, the underlying immunological concepts indicate that these vaccines have broader applicability, including in the control and prevention of infectious diseases through targeting conserved antigens.
Mechanisms of Action
The success of shared antigen vaccines relies on their ability to stimulate a specific and durable immune response. By presenting conserved antigens to the immune system, these vaccines leverage both the innate and adaptive arms of immunity.
Immune Response Elicitation
Shared antigen vaccines are designed to activate key cellular players that drive anti-tumor or anti-pathogen responses. The primary mechanisms include:
1. Dendritic Cell Activation and Antigen Presentation:
Vaccines such as Sipuleucel-T are engineered to use a patient’s antigen-presenting cells (APCs) to process and present tumor antigens to T cells. This activation bridges the innate and adaptive immune responses, allowing for subsequent activation of cytotoxic T lymphocytes (CTLs) that directly target antigen-expressing cells.
2. CD8+ T-Cell Mediated Cytotoxicity:
The generation of a robust CD8+ T-cell response has been critical in shared antigen vaccine development. By cross-presenting shared tumor-associated antigens, these vaccines stimulate CTLs capable of recognizing and destroying tumor cells, even when the antigens are shared among multiple tumors.
3. Helper T-Cell Involvement:
In addition to cytotoxic T cells, helper T cells (CD4+) are also activated by these vaccines, supporting the maturation and expansion of CTLs and contributing to a more sustained immune response. The interplay between CD4+ and CD8+ T cells is crucial, as shown in several clinical studies evaluating vaccine efficacy.
4. Humoral Response and Antibody Production:
Some shared antigen vaccines additionally aim to induce antibody responses. In the context of HER2-targeted vaccines, for instance, the production of antibodies can serve both to neutralize the antigen and to mediate antibody-dependent cellular cytotoxicity (ADCC), thereby amplifying the anti-tumor effect.
5. Stimulation of Memory Response:
The ultimate goal of these vaccines is not just to induce an immediate response but to generate immunological memory. This capacity enables the vaccinated individual to mount a faster and more potent response upon re-exposure to the antigen, which is especially vital in the context of cancer where relapse is a persistent risk.
Cross-reactivity and Safety
Given that shared antigen vaccines target antigens that are also expressed, albeit at lower levels, in non-tumor tissues, there is an inherent risk of cross-reactivity. However, multiple strategies are employed to both enhance efficacy and mitigate adverse events:
1. Selective Antigen Design:
Vaccine developers meticulously select antigens that are overexpressed in tumor cells compared to normal tissue. This selectivity minimizes off-target effects and limits the potential for autoimmunity.
2. Use of Adjuvants to Modulate Immune Response:
The inclusion of immunostimulatory adjuvants can enhance the specificity of the immune response by promoting the activation of APCs and modulating the cytokine milieu. This ensures that the immune response is directed toward the tumor antigen rather than self-antigens.
3. Monitoring Cross-reactivity:
Preclinical and clinical trials routinely monitor biomarkers of cross-reactivity to detect any potential adverse events resulting from immune attack against normal tissues. Advanced immunological assays help establish the thresholds for safe activation of the immune system while avoiding collateral damage.
4. Enhancing Antigen Presentation:
Techniques that improve antigen processing and presentation help ensure that even low levels of antigen expression in non-target tissues do not inadvertently trigger an immune response against healthy cells—a critical balance for safety.
Clinical Trials and Research
The clinical investigation of shared antigen vaccines has evolved considerably over the past decades, especially in the realm of oncology. Clinical trials have provided insights into the immunogenicity, safety, and efficacy of vaccines targeting shared antigens.
Current Clinical Trials
A number of clinical trials are underway to evaluate the efficacy of shared antigen vaccines in different cancer indications. Key examples include:
1. Sipuleucel-T (Dendreon Corporation):
This vaccine is approved in the United States for metastatic castration-resistant prostate cancer. Its success is driven by the ex vivo stimulation of autologous immune cells with a fusion protein containing a shared antigen, which leads to a robust anti-tumor T cell response. Its clinical success has paved the way for further investigations into shared antigen vaccine approaches across cancer indications.
2. EP-2101 (IDM Pharma, Inc.):
Investigated in Phase 3 trials, EP-2101 targets the p53 antigen, which is widely mutated in numerous cancers. Its development indicates a broader application beyond prostate cancer, extending into respiratory, digestive, endocrine, and urogenital diseases.
3. Nelipepimut-S (The University of Texas MD Anderson Cancer Center):
This experimental vaccine is currently in Phase 3 and targets HER2-expressing tumors, including breast and other cancers. The goal is to induce a strong T-cell response against HER2-positive cells, which are common in several solid tumors.
4. AE-37/GP-2 Vaccine (Generex Biotechnology Corp.):
In Phase 2 trials, this vaccine further underscores the focus on HER2-targeted therapy. The investigational approach is aimed at stimulating both CD4+ and CD8+ T cells in patients with HER2-expressing cancers, particularly those affecting the skin, musculoskeletal, and urogenital systems.
5. PAP Vaccine (Madison Vaccines, Inc.):
This vaccine is in Phase 2 and targets prostatic acid phosphatase, a shared antigen in prostate cancer. Its investigational use extends its potential application to other urogenital diseases, including those associated with the digestive and endocrine systems.
6. Oncoquest-PC and OQR-200:
These are in preclinical to early clinical evaluation stages. Oncoquest-PC is designed as a shared antigen vaccine targeting IL-2R agonism, and OQR-200 focuses on HER2 antagonism. Both represent promising strategies for treating various neoplasms and urogenital cancers, although further data is needed to validate their efficacy.
7. Discontinued Candidates:
Early investigational candidates such as the NY-ESO-1/LAGE-1 peptide vaccine and VEGFR1 peptide vaccines, although currently discontinued, provided valuable insights into the complexity of targeting shared antigens in cancer. Their clinical trial data helped inform subsequent vaccine designs and immunotherapy strategies.
Preliminary Results and Findings
Preliminary clinical findings have been encouraging in several respects, particularly regarding the induction of antigen-specific immune responses:
1. Immunogenicity:
Many of these shared antigen vaccines have been shown to induce the desired T-cell responses. For example, early-phase clinical trials of the PAP vaccine and HER2-targeting vaccines have demonstrated significant increases in antigen-specific cytotoxic T lymphocytes and helper T cells. This immunogenicity is often measured through increases in specific antibody titers or T-cell activation markers post-vaccination.
2. Clinical Efficacy:
The clinical outcomes observed, such as prolonged survival and delayed disease progression in metastatic prostate cancer treated with Sipuleucel-T, have provided proof-of-concept evidence supporting the effectiveness of shared antigen approaches. Similarly, Phase 2 and Phase 3 trials evaluating HER2-based vaccines have underscored the potential to target tumors with reduced expression of the antigen in normal tissues while maximizing immune-mediated tumor destruction.
3. Safety Profile:
Safety data from these trials suggests that, with carefully selected antigens and optimized adjuvant formulations, shared antigen vaccines can achieve an acceptable safety profile. While some adverse events related to injection site reactions and transient systemic symptoms have been observed, they tend to be mild to moderate and manageable. Monitoring for cross-reactivity is an inherent part of these studies, and the results so far have not indicated significant off-target toxicity.
4. Biomarker Identification:
Studies have also focused on identifying biomarkers that predict vaccine efficacy. For instance, some trials have provided insights into correlates of immune protection, enabling subsequent modifications to vaccine design to enhance both the breadth and durability of the immune response. These data are crucial for the design of adaptive clinical trials that can refine dosage regimens and patient selection criteria.
Challenges and Future Directions
While the research into shared antigen vaccines has yielded promising results, several challenges remain that must be addressed to optimize their clinical utility.
Developmental Challenges
1. Tumor Heterogeneity and Immune Evasion:
One of the greatest challenges is the inherent heterogeneity of tumors. Even when a shared antigen is overexpressed in many tumors, variability in antigen presentation and genetic mutations within different tumor clones can limit vaccine efficacy. Moreover, tumor cells can downregulate antigen expression or MHC molecules as an immune evasion strategy, reducing the effectiveness of the vaccine-induced immune response.
2. Optimizing Antigen Selection:
Selecting an antigen that is both immunogenic and selectively overexpressed in tumor tissues without significant cross-reactivity to normal cells is a complex process. As seen with some discontinued candidates (e.g., NY-ESO-1/LAGE-1 and VEGFR1 vaccines), even slight variations in antigen expression can impact both efficacy and safety. Continued refinement in antigen identification using genomics and proteomics is necessary.
3. Combination Strategies:
The evolving landscape of cancer immunotherapy increasingly recognizes that single-agent vaccine therapy may not suffice in the face of complex tumor microenvironments. There is an ongoing challenge to integrate shared antigen vaccines with other modalities such as immune checkpoint inhibitors, adoptive cell therapies, and conventional chemotherapy or radiotherapy. Determining the optimal timing, dosing, and sequence of these combination therapies remains a critical developmental hurdle.
4. Immunogenicity versus Tolerance:
Overcoming the immunological tolerance that the body may have toward self-antigens remains a formidable challenge. As many shared antigens are derived from proteins that are also expressed at low levels in normal tissues, there is a fine line between inducing an effective anti-tumor response and triggering autoimmunity. Innovations in adjuvant design and delivery systems are being employed to tilt the balance toward immunogenicity without compromising safety.
5. Manufacturing and Regulatory Issues:
The complexity of producing autologous cell-based vaccines, as well as the scalability of peptide-based or DNA-based platforms, poses significant manufacturing challenges. Regulatory pathways for novel vaccine designs are still evolving, which can impact the speed at which these therapies reach larger clinical trials and eventually the market. Harmonizing manufacturing processes and regulatory frameworks is essential for broader clinical adoption.
Future Research Directions
Given these challenges, several promising research directions are anticipated to drive the next generation of shared antigen vaccines forward:
1. Advanced Antigen Discovery Platforms:
Utilizing high-throughput sequencing, proteomics, and bioinformatics, future research is likely to focus on identifying more robust shared antigens that show higher immunogenic potential and lower risk of cross-reactivity. Systems biology approaches will facilitate the discovery of novel antigens that are conserved across various tumor types and could serve as universal targets.
2. Improved Delivery Systems and Formulations:
Innovations such as nanoparticle-based delivery systems and novel adjuvant formulations can enhance the uptake and presentation of antigens while ensuring sustained release and optimal immunostimulation. These advances will likely reduce the number of booster injections required and improve patient compliance.
3. Combination Immunotherapy Regimens:
Ongoing and future clinical trials are expected to explore synergistic combinations of shared antigen vaccines with other immunotherapeutic agents. This includes pairing vaccines with immune checkpoint inhibitors, targeted therapies, or even next-generation CAR-T cell therapies tailored for solid tumors. Such combination strategies may overcome intrinsic tumor resistance and improve overall clinical outcomes.
4. Personalized Approaches within a Shared Framework:
Despite the “shared” nature of the antigens used, future vaccine strategies might incorporate personalized modifications based on individual patient tumor profiling. By stratifying patients based on molecular and immunological biomarkers, clinicians can improve the selection of candidates most likely to benefit from the vaccine, thereby enhancing efficacy while minimizing side effects.
5. Real-Time Adaptive Clinical Trials:
The implementation of adaptive trial designs that allow for modifications in dosing and formulation based on interim results could accelerate the clinical development timeline. These trials can incorporate real-time biomarker data to adjust parameters and enhance the precision of the vaccine’s immunological targeting.
6. Addressing Immune Tolerance Mechanisms:
Future studies will also focus on the mechanisms of immune tolerance and strategies to overcome it without inducing autoimmunity. This may include fine-tuning the antigen concentration, adjusting adjuvant selection, or engineering antigens to modify their immunogenic properties. Increased understanding of the T-cell repertoire and antigen presentation dynamics will be key to overcoming this barrier.
Conclusion
Shared antigen vaccines represent a paradigm shift in the field of cancer immunotherapy by targeting antigens that are commonly expressed among diverse tumor types. Their investigational indications are predominantly within oncology, where vaccines such as Sipuleucel-T, PAP vaccine, HER2-targeting vaccines (Nelipepimut-S, AE-37/GP-2), EP-2101, Oncoquest-PC, and OQR-200 are being evaluated in various stages of clinical development. Although the current focus is largely on neoplastic conditions—especially metastatic, urogenital, and HER2-positive cancers—the shared antigen strategy holds promise for broader application, including infectious diseases, where targeting conserved viral epitopes can lead to broad cross-protective immune responses.
The mechanism of action of shared antigen vaccines relies on the robust activation of both innate and adaptive immune responses, particularly through dendritic cell activation, T-cell mediated cytotoxicity, and the generation of immunological memory. At the same time, considerable efforts are expended to address challenges related to cross-reactivity and safety—a critical balance to ensure effective targeting without causing autoimmune damage.
Clinical trials across various phases have demonstrated promising immunogenicity and acceptable safety profiles, although complexities such as tumor heterogeneity, immune evasion, and manufacturing challenges persist. Future research is oriented toward refining antigen selection via advanced omics technologies, improving vaccine formulations through innovative delivery systems, and developing adaptive, combination immunotherapy regimens that integrate shared antigen approaches with other therapeutic modalities.
In summary, shared antigen vaccines are being investigated primarily for their potential to treat a wide range of cancers by leveraging common tumor-associated antigens. Their development is informed by both successes and setbacks in clinical trials, which continue to guide the evolution of vaccine design, immune modulation, and personalized therapeutic strategies. As research progresses, these vaccines may not only offer improved outcomes for patients with currently challenging neoplasms but could also extend their utility to combat emerging infectious diseases through targeting conserved antigenic regions. The pursuit of improved efficacy and safety along with adaptive clinical strategies underscores the dynamic future of shared antigen vaccines in modern immunotherapy.
Shared antigen vaccines are a category of therapeutic vaccines designed to target antigens that are commonly expressed among tumors or other disease‐affected tissues across different patients. These vaccines differ from personalized or neoantigen vaccines in that they exploit well‐characterized, “shared” molecular markers, which are expressed on multiple tumor types or in recurrent disease patterns. In essence, they leverage a “one-size-fits-all” antigen approach that can be applied across a broader spectrum of patients, primarily in oncology.
Definition and Basic Concepts
Shared antigen vaccines are formulated using antigens that are not unique to a single tumor but rather are expressed across a range of cancers. These antigens are often proteins or peptides that serve critical functions in tumor cell physiology and are recognized by the immune system. By targeting these targets, the vaccines aim to elicit a robust T-cell and antibody-mediated response against cancer cells. For example, Sipuleucel-T, which is based on a shared antigen strategy, utilizes immunostimulants to target prostate antigens and generate long-lasting immune responses. Similar approaches include vaccines that target HER2, NY-ESO-1, and PAP—each representing a shared antigen among particular groups of tumors. The core concept is to overcome the immunosuppressive tumor microenvironment by recognizing these relatively invariant antigens, which in many cases are essential for tumor survival and therefore less likely to be lost through mutation.
Overview of Vaccine Development
Vaccine development in the context of shared antigens has evolved through several generations. Initially, vaccines were based on whole pathogens or tumor cell lysates, which sometimes resulted in non-specific immune responses. Today, however, advances in recombinant DNA technology and improved antigen characterization have allowed vaccine developers to isolate specific epitopes responsible for immune recognition. Key to this advancement has been the integration of adjuvants and modern delivery platforms. Shared antigen vaccines have been designed using multiple antigen formats such as peptide vaccines, DNA vaccines, and immune cell therapies—all seeking to present the shared antigen effectively to antigen-presenting cells (APCs). The development pathway typically includes preclinical evaluations in animal models, followed by iterative clinical phases to assess safety, immunogenicity, and eventual clinical efficacy. Large-scale clinical trials, especially in oncology, are crucial to validate that these shared antigens can serve as effective targets for immunotherapy.
Investigational Indications for Shared Antigen Vaccines
Shared antigen vaccines are predominantly investigated in the field of oncology due to the need for treatments that address multiple cancer types simultaneously and overcome tumor immune evasion. That said, there are also exploratory studies looking at shared antigen concepts for infectious diseases. Here, we outline the investigational indications for these vaccines from both a general and specific perspective.
Cancer Indications
Cancer remains the primary indication for which shared antigen vaccines have been extensively investigated. The rationale is based on the observation that many malignancies express common tumor-associated antigens (TAAs) that can be exploited as targets for immunotherapy.
1. Prostate Cancer:
Sipuleucel-T, the first FDA-approved therapeutic cancer vaccine, is designed to treat metastatic castration-resistant prostate cancer and relies on the delivery of a shared antigen that stimulates an immune response against prostate tumor cells. Moreover, PAP vaccines, such as the one developed by Madison Vaccines, Inc., target prostatic acid phosphatase (PAP), a widely expressed antigen in prostate cancer. These vaccines work by activating dendritic cells which can then stimulate cytotoxic T lymphocytes to attack cells expressing PAP.
2. HER2-Expressing Cancers:
Several shared antigen vaccines specifically target the HER2 protein—a receptor overexpressed in a variety of cancers including breast, ovarian, and gastric carcinomas. Nelipepimut-S, for instance, is a shared antigen vaccine aimed at eliciting an immune response against HER2-positive tumor cells. Additionally, AE-37/GP-2, produced by Generex Biotechnology Corp., is another vaccine formulation that targets HER2 through shared antigen strategies. These vaccines have been examined in clinical trials to determine whether boosting immune responses against HER2 can reduce tumor burden and delay disease progression.
3. Broad Spectrum Neoplasms and Urogenital Cancers:
EP-2101, an investigational vaccine from IDM Pharma Inc., is currently in Phase 3 and targets a range of neoplasms, including those affecting respiratory, digestive, and urogenital systems. Similarly, OQR-200, developed by OncoQR ML GmbH, is in its preclinical stage and focuses on tumors within the neoplastic and urogenital disease groups. Furthermore, products like Oncoquest-PC, developed by Xeme Biopharma Inc., are intended for neoplasms with urogenital involvement even at an early preclinical phase.
4. Melanoma and Other Solid Tumors:
Although not exclusively reserved for melanoma, some shared antigen vaccines have shown promise in broader applications including skin and musculoskeletal cancers. For example, the vaccine strategies targeting HER2 or other shared antigens might benefit tumors in these sites by inducing targeted immune responses. Such strategies have also been investigated in combination with other immunotherapeutic modalities to enhance overall response rates.
5. Discontinued or Investigational Candidates:
Some shared antigen vaccine candidates, like the NY-ESO-1/LAGE-1 class I/II peptide vaccine developed at Baylor College of Medicine and VEGFR1 peptide vaccines from The University of Tokyo Hospital, although currently discontinued or not progressing in clinical trials, provide insight into the complex challenges associated with targeting shared antigens. Their clinical pathways highlight both the potential and the pitfalls in targeting widely expressed tumor antigens.
Collectively, these cancer indications demonstrate the diversity of tumor types that can potentially benefit from shared antigen vaccines. They are designed to harness the body’s immune system against tumors that share common molecular features, thereby providing a therapeutic option that could potentially be applied to a wide patient population.
Infectious Diseases
While the bulk of the current investigational data on shared antigen vaccines focuses on oncology, the concept is also applicable to infectious diseases. Shared antigen vaccines in infectious disease settings aim to target conserved epitopes across different strains of a pathogen. For example, influenza vaccines and universal coronavirus vaccines often seek to incorporate antigens that are conserved among the highly mutable strains of the viruses. Although the provided references do not include many examples of shared antigen vaccines explicitly developed for infectious diseases (most infectious disease vaccine references pertain to recombinant protein vaccines, viral vector vaccines, or combination vaccines), the principle remains similar.
1. Influenza Vaccines:
Some patents and research studies have described vaccines that incorporate influenza virus antigens harvested through improved purification methods to achieve high-purity virus antigen standards. These methods aim to identify shared viral antigens that remain conserved despite ongoing mutations. In such a scenario, the antigen design mimics the shared antigen strategy used in cancer vaccines but is oriented toward eliciting broad cross-protective immunity against multiple influenza strains.
2. Universal Coronavirus Vaccines:
The idea of developing a universal coronavirus vaccine—one that could provide broad immunity across variants—also leverages the concept of shared or conserved antigen targets. Recent research prioritizes identifying epitopes that are less likely to mutate (such as regions away from the mutable receptor-binding domain), thereby ensuring long-term efficacy. This parallels the strategy used in developing shared antigen vaccines for cancers, where maintaining immunogenicity despite tumor heterogeneity is a challenge.
3. Other Pathogens:
Similar approaches are being explored for other infectious agents such as tuberculosis, dengue, and even certain bacterial infections where antigen conservation across strains might be exploited. However, unlike cancer indications where the focus has been more pronounced, infectious disease applications are still evolving and may require combining adjuvants and more sophisticated delivery systems to overcome the inherent variability of pathogen antigens.
Overall, while the dominant research and clinical trial data on shared antigen vaccines derive from oncology, the underlying immunological concepts indicate that these vaccines have broader applicability, including in the control and prevention of infectious diseases through targeting conserved antigens.
Mechanisms of Action
The success of shared antigen vaccines relies on their ability to stimulate a specific and durable immune response. By presenting conserved antigens to the immune system, these vaccines leverage both the innate and adaptive arms of immunity.
Immune Response Elicitation
Shared antigen vaccines are designed to activate key cellular players that drive anti-tumor or anti-pathogen responses. The primary mechanisms include:
1. Dendritic Cell Activation and Antigen Presentation:
Vaccines such as Sipuleucel-T are engineered to use a patient’s antigen-presenting cells (APCs) to process and present tumor antigens to T cells. This activation bridges the innate and adaptive immune responses, allowing for subsequent activation of cytotoxic T lymphocytes (CTLs) that directly target antigen-expressing cells.
2. CD8+ T-Cell Mediated Cytotoxicity:
The generation of a robust CD8+ T-cell response has been critical in shared antigen vaccine development. By cross-presenting shared tumor-associated antigens, these vaccines stimulate CTLs capable of recognizing and destroying tumor cells, even when the antigens are shared among multiple tumors.
3. Helper T-Cell Involvement:
In addition to cytotoxic T cells, helper T cells (CD4+) are also activated by these vaccines, supporting the maturation and expansion of CTLs and contributing to a more sustained immune response. The interplay between CD4+ and CD8+ T cells is crucial, as shown in several clinical studies evaluating vaccine efficacy.
4. Humoral Response and Antibody Production:
Some shared antigen vaccines additionally aim to induce antibody responses. In the context of HER2-targeted vaccines, for instance, the production of antibodies can serve both to neutralize the antigen and to mediate antibody-dependent cellular cytotoxicity (ADCC), thereby amplifying the anti-tumor effect.
5. Stimulation of Memory Response:
The ultimate goal of these vaccines is not just to induce an immediate response but to generate immunological memory. This capacity enables the vaccinated individual to mount a faster and more potent response upon re-exposure to the antigen, which is especially vital in the context of cancer where relapse is a persistent risk.
Cross-reactivity and Safety
Given that shared antigen vaccines target antigens that are also expressed, albeit at lower levels, in non-tumor tissues, there is an inherent risk of cross-reactivity. However, multiple strategies are employed to both enhance efficacy and mitigate adverse events:
1. Selective Antigen Design:
Vaccine developers meticulously select antigens that are overexpressed in tumor cells compared to normal tissue. This selectivity minimizes off-target effects and limits the potential for autoimmunity.
2. Use of Adjuvants to Modulate Immune Response:
The inclusion of immunostimulatory adjuvants can enhance the specificity of the immune response by promoting the activation of APCs and modulating the cytokine milieu. This ensures that the immune response is directed toward the tumor antigen rather than self-antigens.
3. Monitoring Cross-reactivity:
Preclinical and clinical trials routinely monitor biomarkers of cross-reactivity to detect any potential adverse events resulting from immune attack against normal tissues. Advanced immunological assays help establish the thresholds for safe activation of the immune system while avoiding collateral damage.
4. Enhancing Antigen Presentation:
Techniques that improve antigen processing and presentation help ensure that even low levels of antigen expression in non-target tissues do not inadvertently trigger an immune response against healthy cells—a critical balance for safety.
Clinical Trials and Research
The clinical investigation of shared antigen vaccines has evolved considerably over the past decades, especially in the realm of oncology. Clinical trials have provided insights into the immunogenicity, safety, and efficacy of vaccines targeting shared antigens.
Current Clinical Trials
A number of clinical trials are underway to evaluate the efficacy of shared antigen vaccines in different cancer indications. Key examples include:
1. Sipuleucel-T (Dendreon Corporation):
This vaccine is approved in the United States for metastatic castration-resistant prostate cancer. Its success is driven by the ex vivo stimulation of autologous immune cells with a fusion protein containing a shared antigen, which leads to a robust anti-tumor T cell response. Its clinical success has paved the way for further investigations into shared antigen vaccine approaches across cancer indications.
2. EP-2101 (IDM Pharma, Inc.):
Investigated in Phase 3 trials, EP-2101 targets the p53 antigen, which is widely mutated in numerous cancers. Its development indicates a broader application beyond prostate cancer, extending into respiratory, digestive, endocrine, and urogenital diseases.
3. Nelipepimut-S (The University of Texas MD Anderson Cancer Center):
This experimental vaccine is currently in Phase 3 and targets HER2-expressing tumors, including breast and other cancers. The goal is to induce a strong T-cell response against HER2-positive cells, which are common in several solid tumors.
4. AE-37/GP-2 Vaccine (Generex Biotechnology Corp.):
In Phase 2 trials, this vaccine further underscores the focus on HER2-targeted therapy. The investigational approach is aimed at stimulating both CD4+ and CD8+ T cells in patients with HER2-expressing cancers, particularly those affecting the skin, musculoskeletal, and urogenital systems.
5. PAP Vaccine (Madison Vaccines, Inc.):
This vaccine is in Phase 2 and targets prostatic acid phosphatase, a shared antigen in prostate cancer. Its investigational use extends its potential application to other urogenital diseases, including those associated with the digestive and endocrine systems.
6. Oncoquest-PC and OQR-200:
These are in preclinical to early clinical evaluation stages. Oncoquest-PC is designed as a shared antigen vaccine targeting IL-2R agonism, and OQR-200 focuses on HER2 antagonism. Both represent promising strategies for treating various neoplasms and urogenital cancers, although further data is needed to validate their efficacy.
7. Discontinued Candidates:
Early investigational candidates such as the NY-ESO-1/LAGE-1 peptide vaccine and VEGFR1 peptide vaccines, although currently discontinued, provided valuable insights into the complexity of targeting shared antigens in cancer. Their clinical trial data helped inform subsequent vaccine designs and immunotherapy strategies.
Preliminary Results and Findings
Preliminary clinical findings have been encouraging in several respects, particularly regarding the induction of antigen-specific immune responses:
1. Immunogenicity:
Many of these shared antigen vaccines have been shown to induce the desired T-cell responses. For example, early-phase clinical trials of the PAP vaccine and HER2-targeting vaccines have demonstrated significant increases in antigen-specific cytotoxic T lymphocytes and helper T cells. This immunogenicity is often measured through increases in specific antibody titers or T-cell activation markers post-vaccination.
2. Clinical Efficacy:
The clinical outcomes observed, such as prolonged survival and delayed disease progression in metastatic prostate cancer treated with Sipuleucel-T, have provided proof-of-concept evidence supporting the effectiveness of shared antigen approaches. Similarly, Phase 2 and Phase 3 trials evaluating HER2-based vaccines have underscored the potential to target tumors with reduced expression of the antigen in normal tissues while maximizing immune-mediated tumor destruction.
3. Safety Profile:
Safety data from these trials suggests that, with carefully selected antigens and optimized adjuvant formulations, shared antigen vaccines can achieve an acceptable safety profile. While some adverse events related to injection site reactions and transient systemic symptoms have been observed, they tend to be mild to moderate and manageable. Monitoring for cross-reactivity is an inherent part of these studies, and the results so far have not indicated significant off-target toxicity.
4. Biomarker Identification:
Studies have also focused on identifying biomarkers that predict vaccine efficacy. For instance, some trials have provided insights into correlates of immune protection, enabling subsequent modifications to vaccine design to enhance both the breadth and durability of the immune response. These data are crucial for the design of adaptive clinical trials that can refine dosage regimens and patient selection criteria.
Challenges and Future Directions
While the research into shared antigen vaccines has yielded promising results, several challenges remain that must be addressed to optimize their clinical utility.
Developmental Challenges
1. Tumor Heterogeneity and Immune Evasion:
One of the greatest challenges is the inherent heterogeneity of tumors. Even when a shared antigen is overexpressed in many tumors, variability in antigen presentation and genetic mutations within different tumor clones can limit vaccine efficacy. Moreover, tumor cells can downregulate antigen expression or MHC molecules as an immune evasion strategy, reducing the effectiveness of the vaccine-induced immune response.
2. Optimizing Antigen Selection:
Selecting an antigen that is both immunogenic and selectively overexpressed in tumor tissues without significant cross-reactivity to normal cells is a complex process. As seen with some discontinued candidates (e.g., NY-ESO-1/LAGE-1 and VEGFR1 vaccines), even slight variations in antigen expression can impact both efficacy and safety. Continued refinement in antigen identification using genomics and proteomics is necessary.
3. Combination Strategies:
The evolving landscape of cancer immunotherapy increasingly recognizes that single-agent vaccine therapy may not suffice in the face of complex tumor microenvironments. There is an ongoing challenge to integrate shared antigen vaccines with other modalities such as immune checkpoint inhibitors, adoptive cell therapies, and conventional chemotherapy or radiotherapy. Determining the optimal timing, dosing, and sequence of these combination therapies remains a critical developmental hurdle.
4. Immunogenicity versus Tolerance:
Overcoming the immunological tolerance that the body may have toward self-antigens remains a formidable challenge. As many shared antigens are derived from proteins that are also expressed at low levels in normal tissues, there is a fine line between inducing an effective anti-tumor response and triggering autoimmunity. Innovations in adjuvant design and delivery systems are being employed to tilt the balance toward immunogenicity without compromising safety.
5. Manufacturing and Regulatory Issues:
The complexity of producing autologous cell-based vaccines, as well as the scalability of peptide-based or DNA-based platforms, poses significant manufacturing challenges. Regulatory pathways for novel vaccine designs are still evolving, which can impact the speed at which these therapies reach larger clinical trials and eventually the market. Harmonizing manufacturing processes and regulatory frameworks is essential for broader clinical adoption.
Future Research Directions
Given these challenges, several promising research directions are anticipated to drive the next generation of shared antigen vaccines forward:
1. Advanced Antigen Discovery Platforms:
Utilizing high-throughput sequencing, proteomics, and bioinformatics, future research is likely to focus on identifying more robust shared antigens that show higher immunogenic potential and lower risk of cross-reactivity. Systems biology approaches will facilitate the discovery of novel antigens that are conserved across various tumor types and could serve as universal targets.
2. Improved Delivery Systems and Formulations:
Innovations such as nanoparticle-based delivery systems and novel adjuvant formulations can enhance the uptake and presentation of antigens while ensuring sustained release and optimal immunostimulation. These advances will likely reduce the number of booster injections required and improve patient compliance.
3. Combination Immunotherapy Regimens:
Ongoing and future clinical trials are expected to explore synergistic combinations of shared antigen vaccines with other immunotherapeutic agents. This includes pairing vaccines with immune checkpoint inhibitors, targeted therapies, or even next-generation CAR-T cell therapies tailored for solid tumors. Such combination strategies may overcome intrinsic tumor resistance and improve overall clinical outcomes.
4. Personalized Approaches within a Shared Framework:
Despite the “shared” nature of the antigens used, future vaccine strategies might incorporate personalized modifications based on individual patient tumor profiling. By stratifying patients based on molecular and immunological biomarkers, clinicians can improve the selection of candidates most likely to benefit from the vaccine, thereby enhancing efficacy while minimizing side effects.
5. Real-Time Adaptive Clinical Trials:
The implementation of adaptive trial designs that allow for modifications in dosing and formulation based on interim results could accelerate the clinical development timeline. These trials can incorporate real-time biomarker data to adjust parameters and enhance the precision of the vaccine’s immunological targeting.
6. Addressing Immune Tolerance Mechanisms:
Future studies will also focus on the mechanisms of immune tolerance and strategies to overcome it without inducing autoimmunity. This may include fine-tuning the antigen concentration, adjusting adjuvant selection, or engineering antigens to modify their immunogenic properties. Increased understanding of the T-cell repertoire and antigen presentation dynamics will be key to overcoming this barrier.
Conclusion
Shared antigen vaccines represent a paradigm shift in the field of cancer immunotherapy by targeting antigens that are commonly expressed among diverse tumor types. Their investigational indications are predominantly within oncology, where vaccines such as Sipuleucel-T, PAP vaccine, HER2-targeting vaccines (Nelipepimut-S, AE-37/GP-2), EP-2101, Oncoquest-PC, and OQR-200 are being evaluated in various stages of clinical development. Although the current focus is largely on neoplastic conditions—especially metastatic, urogenital, and HER2-positive cancers—the shared antigen strategy holds promise for broader application, including infectious diseases, where targeting conserved viral epitopes can lead to broad cross-protective immune responses.
The mechanism of action of shared antigen vaccines relies on the robust activation of both innate and adaptive immune responses, particularly through dendritic cell activation, T-cell mediated cytotoxicity, and the generation of immunological memory. At the same time, considerable efforts are expended to address challenges related to cross-reactivity and safety—a critical balance to ensure effective targeting without causing autoimmune damage.
Clinical trials across various phases have demonstrated promising immunogenicity and acceptable safety profiles, although complexities such as tumor heterogeneity, immune evasion, and manufacturing challenges persist. Future research is oriented toward refining antigen selection via advanced omics technologies, improving vaccine formulations through innovative delivery systems, and developing adaptive, combination immunotherapy regimens that integrate shared antigen approaches with other therapeutic modalities.
In summary, shared antigen vaccines are being investigated primarily for their potential to treat a wide range of cancers by leveraging common tumor-associated antigens. Their development is informed by both successes and setbacks in clinical trials, which continue to guide the evolution of vaccine design, immune modulation, and personalized therapeutic strategies. As research progresses, these vaccines may not only offer improved outcomes for patients with currently challenging neoplasms but could also extend their utility to combat emerging infectious diseases through targeting conserved antigenic regions. The pursuit of improved efficacy and safety along with adaptive clinical strategies underscores the dynamic future of shared antigen vaccines in modern immunotherapy.
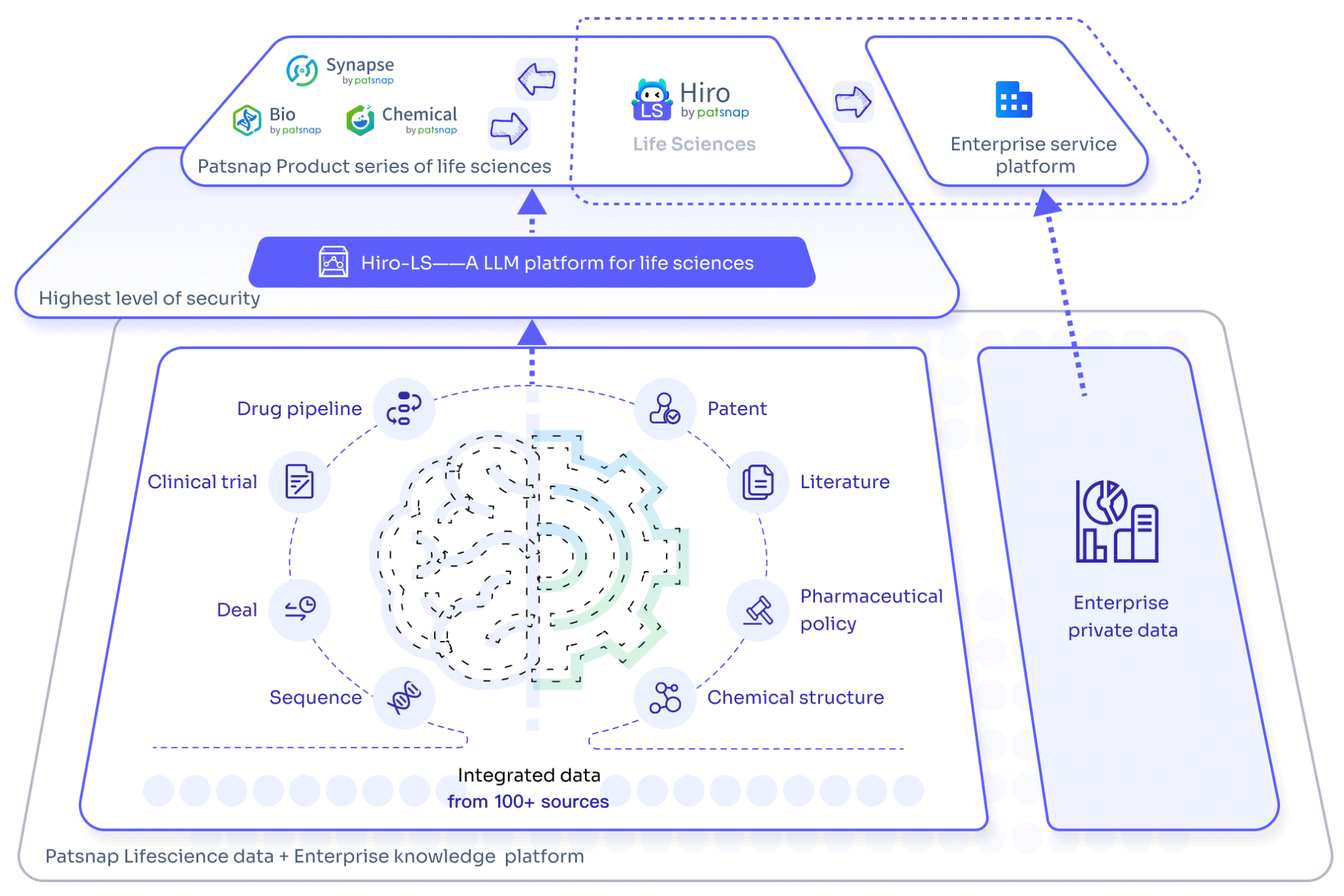
For an experience with the large-scale biopharmaceutical model Hiro-LS, please click here for a quick and free trial of its features!
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.