Request Demo
What are Cav1.2 antagonists and how do they work?
21 June 2024
Cav1.2 antagonists are a group of pharmacological agents that play a crucial role in modern medicine, particularly in the management of cardiovascular diseases. Cav1.2 channels are a subtype of L-type calcium channels predominantly found in cardiac and smooth muscle cells, where they facilitate the influx of calcium ions into the cells. This calcium influx is essential for various cellular processes, including muscle contraction and neurotransmission. However, dysregulation of Cav1.2 channels can lead to pathological conditions such as hypertension, arrhythmias, and other cardiovascular disorders. Cav1.2 antagonists, also known as calcium channel blockers, effectively inhibit these channels, thereby offering therapeutic benefits for several medical conditions.
Cav1.2 antagonists work by binding to the voltage-dependent L-type calcium channels on the cell membrane of cardiac and smooth muscle cells. These channels are responsible for the initial influx of calcium ions when the cell membrane depolarizes. The binding of Cav1.2 antagonists prevents the opening of these channels, thereby reducing the influx of calcium ions into the cells. This inhibition decreases intracellular calcium concentrations, which is pivotal for muscle contraction. In cardiac muscles, reduced calcium entry leads to decreased contractility, which lowers the heart's workload and oxygen demand. In smooth muscle cells, such as those lining the blood vessels, reduced calcium entry causes vasodilation, leading to a decrease in blood pressure. This dual action—reducing cardiac workload and inducing vasodilation—makes Cav1.2 antagonists highly effective in treating various cardiovascular conditions.
One of the primary uses of Cav1.2 antagonists is in the management of hypertension. Hypertension, or high blood pressure, is a major risk factor for cardiovascular diseases, including heart attack, stroke, and heart failure. By inhibiting the L-type calcium channels in the smooth muscle cells of blood vessels, Cav1.2 antagonists cause vasodilation, which reduces peripheral resistance and subsequently lowers blood pressure. This makes them an essential component of antihypertensive therapy, often used in conjunction with other medications such as ACE inhibitors or diuretics for comprehensive blood pressure control.
Cav1.2 antagonists are also used in the treatment of angina pectoris, a condition characterized by chest pain due to reduced blood flow to the heart muscle. By decreasing the contractility of the heart and inducing vasodilation, these drugs help to improve oxygen supply to the myocardium while simultaneously reducing its oxygen demand. This dual action alleviates the chest pain associated with angina and improves the overall quality of life for patients suffering from this condition.
Another significant application of Cav1.2 antagonists is in the management of arrhythmias, which are irregular heartbeats that can lead to serious complications if not properly managed. By reducing the influx of calcium ions into cardiac cells, these drugs help stabilize the electrical activity of the heart, thereby preventing abnormal heart rhythms. This is particularly beneficial in conditions such as atrial fibrillation, where rapid and irregular heartbeats can increase the risk of stroke and heart failure.
In addition to their primary cardiovascular applications, Cav1.2 antagonists are also being explored for their potential benefits in other medical conditions. For instance, some studies suggest that these drugs may have neuroprotective effects, making them a potential therapeutic option for neurodegenerative diseases such as Alzheimer's disease. While this area of research is still in its early stages, the broad-ranging effects of Cav1.2 antagonists on calcium signaling pathways make them a promising candidate for various therapeutic applications beyond cardiovascular health.
In summary, Cav1.2 antagonists are a versatile and effective group of medications that have revolutionized the management of several cardiovascular conditions. By inhibiting L-type calcium channels, they reduce intracellular calcium levels, leading to decreased cardiac contractility and vasodilation. This makes them invaluable in the treatment of hypertension, angina pectoris, and arrhythmias. As research continues to uncover new potential applications for these drugs, their role in modern medicine is likely to expand, offering hope for improved therapies for a range of conditions.
Cav1.2 antagonists work by binding to the voltage-dependent L-type calcium channels on the cell membrane of cardiac and smooth muscle cells. These channels are responsible for the initial influx of calcium ions when the cell membrane depolarizes. The binding of Cav1.2 antagonists prevents the opening of these channels, thereby reducing the influx of calcium ions into the cells. This inhibition decreases intracellular calcium concentrations, which is pivotal for muscle contraction. In cardiac muscles, reduced calcium entry leads to decreased contractility, which lowers the heart's workload and oxygen demand. In smooth muscle cells, such as those lining the blood vessels, reduced calcium entry causes vasodilation, leading to a decrease in blood pressure. This dual action—reducing cardiac workload and inducing vasodilation—makes Cav1.2 antagonists highly effective in treating various cardiovascular conditions.
One of the primary uses of Cav1.2 antagonists is in the management of hypertension. Hypertension, or high blood pressure, is a major risk factor for cardiovascular diseases, including heart attack, stroke, and heart failure. By inhibiting the L-type calcium channels in the smooth muscle cells of blood vessels, Cav1.2 antagonists cause vasodilation, which reduces peripheral resistance and subsequently lowers blood pressure. This makes them an essential component of antihypertensive therapy, often used in conjunction with other medications such as ACE inhibitors or diuretics for comprehensive blood pressure control.
Cav1.2 antagonists are also used in the treatment of angina pectoris, a condition characterized by chest pain due to reduced blood flow to the heart muscle. By decreasing the contractility of the heart and inducing vasodilation, these drugs help to improve oxygen supply to the myocardium while simultaneously reducing its oxygen demand. This dual action alleviates the chest pain associated with angina and improves the overall quality of life for patients suffering from this condition.
Another significant application of Cav1.2 antagonists is in the management of arrhythmias, which are irregular heartbeats that can lead to serious complications if not properly managed. By reducing the influx of calcium ions into cardiac cells, these drugs help stabilize the electrical activity of the heart, thereby preventing abnormal heart rhythms. This is particularly beneficial in conditions such as atrial fibrillation, where rapid and irregular heartbeats can increase the risk of stroke and heart failure.
In addition to their primary cardiovascular applications, Cav1.2 antagonists are also being explored for their potential benefits in other medical conditions. For instance, some studies suggest that these drugs may have neuroprotective effects, making them a potential therapeutic option for neurodegenerative diseases such as Alzheimer's disease. While this area of research is still in its early stages, the broad-ranging effects of Cav1.2 antagonists on calcium signaling pathways make them a promising candidate for various therapeutic applications beyond cardiovascular health.
In summary, Cav1.2 antagonists are a versatile and effective group of medications that have revolutionized the management of several cardiovascular conditions. By inhibiting L-type calcium channels, they reduce intracellular calcium levels, leading to decreased cardiac contractility and vasodilation. This makes them invaluable in the treatment of hypertension, angina pectoris, and arrhythmias. As research continues to uncover new potential applications for these drugs, their role in modern medicine is likely to expand, offering hope for improved therapies for a range of conditions.
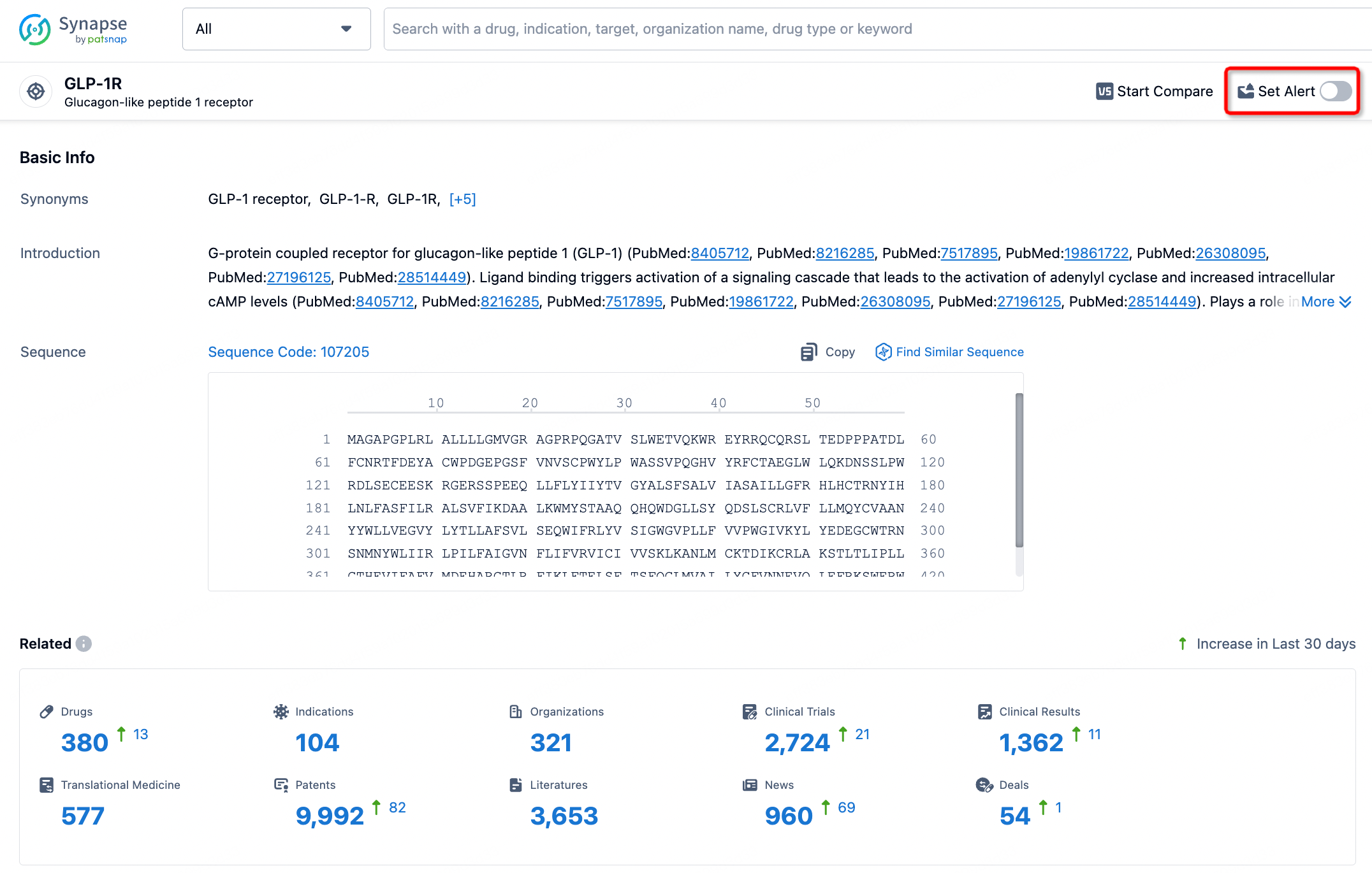
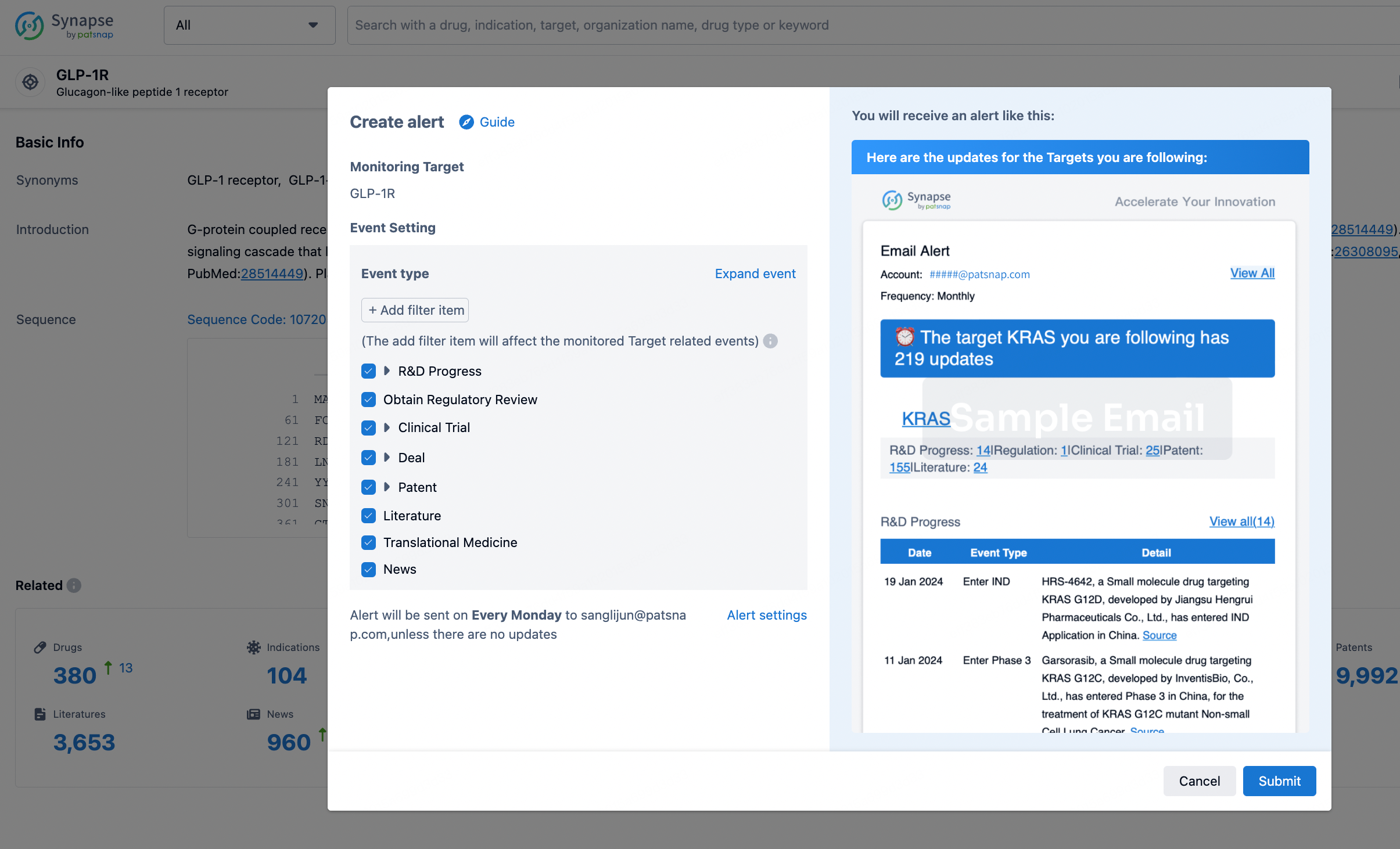
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.