Request Demo
What are GP IIb/IIIa modulators and how do they work?
21 June 2024
In the realm of cardiovascular medicine, GP IIb/IIIa modulators have emerged as critical agents in managing and preventing thrombotic events. These modulators target the GP IIb/IIIa receptor, a crucial component in platelet aggregation, which plays a significant role in clot formation. By understanding the function and application of GP IIb/IIIa modulators, healthcare professionals can better appreciate their importance in treating various cardiovascular conditions.
GP IIb/IIIa modulators work by targeting the glycoprotein IIb/IIIa receptor found on the surface of platelets. This receptor is integral to the platelet aggregation process, which is a key step in the formation of blood clots. Under normal circumstances, when a blood vessel is injured, platelets are activated and aggregate at the site of injury to form a clot, preventing excessive bleeding. The GP IIb/IIIa receptor binds fibrinogen and other adhesive molecules, forming a bridge between platelets and facilitating their clumping together.
GP IIb/IIIa modulators inhibit this receptor, thereby preventing the binding of fibrinogen and other ligands. This inhibition disrupts platelet aggregation, reducing the likelihood of clot formation. These drugs can be particularly effective because they target the final common pathway of platelet aggregation, ensuring a high efficacy in preventing clots. The modulation of GP IIb/IIIa receptors is a finely tuned process that requires precise dosing and administration to achieve the desired therapeutic outcomes without causing excessive bleeding.
GP IIb/IIIa modulators are primarily used in the management of acute coronary syndromes (ACS) and during percutaneous coronary interventions (PCIs). Acute coronary syndromes encompass a range of conditions associated with sudden, reduced blood flow to the heart, including myocardial infarction (heart attack) and unstable angina. In these scenarios, preventing platelet aggregation is crucial to maintaining blood flow and minimizing heart tissue damage.
During PCIs, which are procedures used to open narrowed or blocked coronary arteries, there is a significant risk of thrombus (clot) formation due to the manipulation of the blood vessels. GP IIb/IIIa modulators are often administered to prevent clot formation during and after the procedure, thereby reducing the risk of complications such as myocardial infarction or restenosis (re-narrowing of the artery).
In addition to their use in ACS and PCIs, GP IIb/IIIa modulators may also be used in other clinical settings where there is a high risk of thrombotic events. For example, they may be administered during certain high-risk surgical procedures or in patients with a history of recurrent thrombotic events. The decision to use these modulators depends on a careful assessment of the patient’s risk factors and the potential benefits of therapy.
Despite their efficacy, the use of GP IIb/IIIa modulators is not without risks. One of the primary concerns with these agents is the potential for bleeding complications. Because they inhibit platelet aggregation, there is an increased risk of both minor and major bleeding events. Therefore, their administration must be carefully monitored, and patients receiving these drugs are often subject to regular blood tests and clinical evaluations to ensure safety.
Furthermore, the development of new antiplatelet and anticoagulant drugs has expanded the options available for managing thrombotic conditions. This has led to a more tailored approach in selecting the appropriate therapy for each patient. While GP IIb/IIIa modulators remain a critical tool in certain clinical scenarios, their use must be balanced with considerations of efficacy, safety, and individual patient factors.
In conclusion, GP IIb/IIIa modulators represent a powerful class of drugs in the prevention and management of thrombotic events, particularly in the settings of acute coronary syndromes and percutaneous coronary interventions. By inhibiting the GP IIb/IIIa receptor, these agents effectively reduce platelet aggregation and clot formation. However, their use requires careful monitoring due to the associated risk of bleeding. As the landscape of antithrombotic therapy evolves, the role of GP IIb/IIIa modulators continues to be refined, ensuring their optimal use in clinical practice.
GP IIb/IIIa modulators work by targeting the glycoprotein IIb/IIIa receptor found on the surface of platelets. This receptor is integral to the platelet aggregation process, which is a key step in the formation of blood clots. Under normal circumstances, when a blood vessel is injured, platelets are activated and aggregate at the site of injury to form a clot, preventing excessive bleeding. The GP IIb/IIIa receptor binds fibrinogen and other adhesive molecules, forming a bridge between platelets and facilitating their clumping together.
GP IIb/IIIa modulators inhibit this receptor, thereby preventing the binding of fibrinogen and other ligands. This inhibition disrupts platelet aggregation, reducing the likelihood of clot formation. These drugs can be particularly effective because they target the final common pathway of platelet aggregation, ensuring a high efficacy in preventing clots. The modulation of GP IIb/IIIa receptors is a finely tuned process that requires precise dosing and administration to achieve the desired therapeutic outcomes without causing excessive bleeding.
GP IIb/IIIa modulators are primarily used in the management of acute coronary syndromes (ACS) and during percutaneous coronary interventions (PCIs). Acute coronary syndromes encompass a range of conditions associated with sudden, reduced blood flow to the heart, including myocardial infarction (heart attack) and unstable angina. In these scenarios, preventing platelet aggregation is crucial to maintaining blood flow and minimizing heart tissue damage.
During PCIs, which are procedures used to open narrowed or blocked coronary arteries, there is a significant risk of thrombus (clot) formation due to the manipulation of the blood vessels. GP IIb/IIIa modulators are often administered to prevent clot formation during and after the procedure, thereby reducing the risk of complications such as myocardial infarction or restenosis (re-narrowing of the artery).
In addition to their use in ACS and PCIs, GP IIb/IIIa modulators may also be used in other clinical settings where there is a high risk of thrombotic events. For example, they may be administered during certain high-risk surgical procedures or in patients with a history of recurrent thrombotic events. The decision to use these modulators depends on a careful assessment of the patient’s risk factors and the potential benefits of therapy.
Despite their efficacy, the use of GP IIb/IIIa modulators is not without risks. One of the primary concerns with these agents is the potential for bleeding complications. Because they inhibit platelet aggregation, there is an increased risk of both minor and major bleeding events. Therefore, their administration must be carefully monitored, and patients receiving these drugs are often subject to regular blood tests and clinical evaluations to ensure safety.
Furthermore, the development of new antiplatelet and anticoagulant drugs has expanded the options available for managing thrombotic conditions. This has led to a more tailored approach in selecting the appropriate therapy for each patient. While GP IIb/IIIa modulators remain a critical tool in certain clinical scenarios, their use must be balanced with considerations of efficacy, safety, and individual patient factors.
In conclusion, GP IIb/IIIa modulators represent a powerful class of drugs in the prevention and management of thrombotic events, particularly in the settings of acute coronary syndromes and percutaneous coronary interventions. By inhibiting the GP IIb/IIIa receptor, these agents effectively reduce platelet aggregation and clot formation. However, their use requires careful monitoring due to the associated risk of bleeding. As the landscape of antithrombotic therapy evolves, the role of GP IIb/IIIa modulators continues to be refined, ensuring their optimal use in clinical practice.
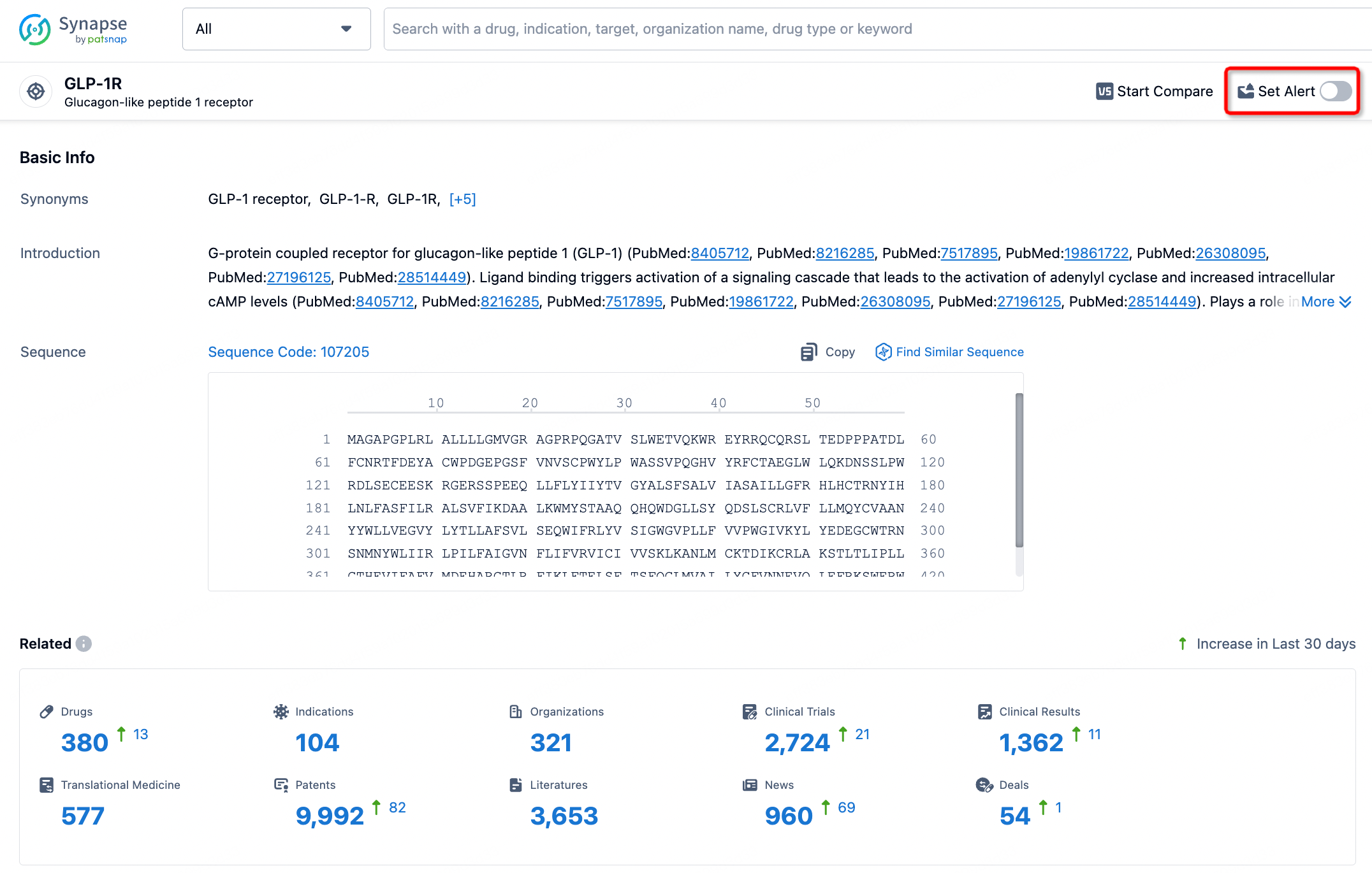
How to obtain the latest development progress of all targets?
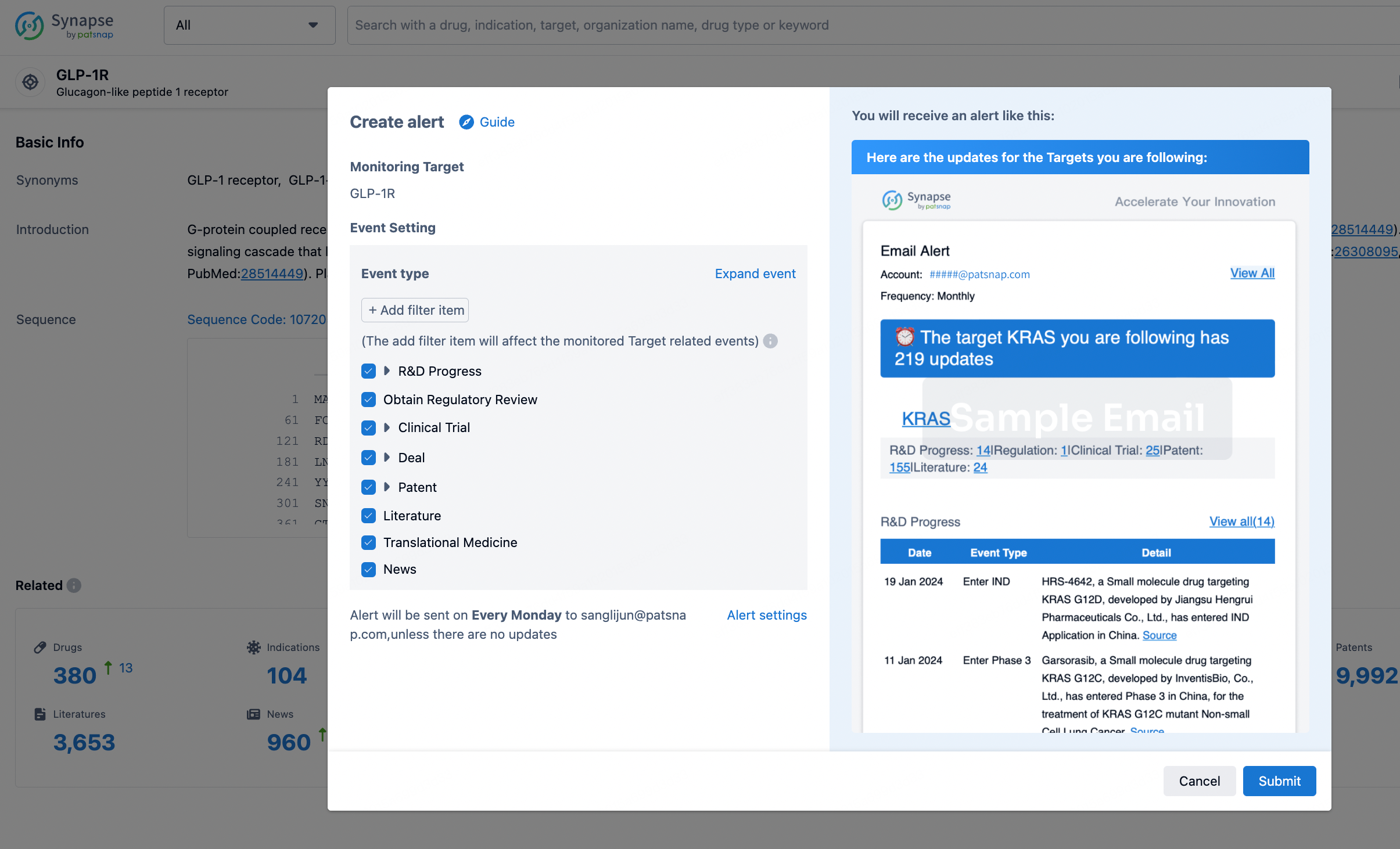
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.