Request Demo
What are L-HBsAg inhibitors and how do they work?
21 June 2024
Introduction to L-HBsAg inhibitors
L-HBsAg inhibitors are emerging as a promising class of therapeutic agents in the battle against chronic Hepatitis B Virus (HBV) infections. Chronic HBV infection remains a significant global health issue, affecting millions of people worldwide and leading to severe liver diseases, including cirrhosis and hepatocellular carcinoma. Efforts to develop effective treatments have led to the identification of various viral targets, among which the large hepatitis B surface antigen (L-HBsAg) stands out as a critical component. L-HBsAg inhibitors specifically target this viral protein, offering new hope for patients with chronic HBV.
How do L-HBsAg inhibitors work?
To understand how L-HBsAg inhibitors function, it is essential to grasp the role of the large hepatitis B surface antigen in the HBV life cycle. The HBV envelope contains three surface proteins: the small (S-HBsAg), middle (M-HBsAg), and large (L-HBsAg) antigens. L-HBsAg, with its unique preS1 domain, plays a crucial role in the initial attachment and entry of the virus into hepatocytes (liver cells). By binding to the sodium taurocholate co-transporting polypeptide (NTCP) receptor on the hepatocyte surface, L-HBsAg facilitates viral entry and subsequent infection.
L-HBsAg inhibitors work by binding to the L-HBsAg protein, thereby disrupting its interaction with the NTCP receptor. This inhibition prevents the virus from attaching to and entering liver cells, effectively blocking the early stages of the HBV life cycle. The precise mechanisms of inhibition can vary depending on the specific inhibitor, but the overarching goal remains the same: to prevent HBV from establishing infection within the host.
What are L-HBsAg inhibitors used for?
The primary use of L-HBsAg inhibitors lies in the treatment of chronic HBV infection. Traditional antiviral therapies, such as nucleos(t)ide analogues (NAs), focus on targeting the viral polymerase to suppress HBV replication. While these treatments can reduce viral load and slow disease progression, they often fall short of achieving a functional cure, where the virus is completely eradicated from the body. This is partly due to the persistence of covalently closed circular DNA (cccDNA), which acts as a reservoir for HBV replication and can remain unaffected by NAs.
L-HBsAg inhibitors offer an innovative approach by targeting a different stage of the viral life cycle. By preventing the virus from entering hepatocytes, these inhibitors can potentially reduce the establishment and replenishment of the cccDNA reservoir. This complementary mechanism of action holds promise for achieving higher rates of functional cure when used in combination with existing antivirals.
Moreover, L-HBsAg inhibitors may also play a role in addressing drug-resistant HBV strains. Resistance to nucleos(t)ide analogues is a growing concern in the management of chronic HBV, as mutations in the viral polymerase can render these drugs less effective. Since L-HBsAg inhibitors target a different viral protein, they provide an alternative therapeutic option that may retain efficacy against resistant strains, thereby enhancing the overall treatment arsenal.
In addition to their antiviral benefits, L-HBsAg inhibitors may help mitigate the immune-mediated liver damage often seen in chronic HBV infection. The chronic presence of HBV antigens, including L-HBsAg, can trigger an immune response that leads to liver inflammation and fibrosis. By reducing the levels of circulating L-HBsAg, these inhibitors may alleviate immune-mediated liver injury and improve overall liver health.
In conclusion, L-HBsAg inhibitors represent a novel and exciting avenue in the treatment of chronic HBV infection. By targeting the large hepatitis B surface antigen and disrupting viral entry, these inhibitors offer a complementary approach to existing therapies. Their potential to enhance functional cure rates, address drug-resistant strains, and mitigate liver damage makes them a promising addition to the arsenal against HBV. As research and clinical trials continue to advance, L-HBsAg inhibitors hold the potential to transform the landscape of HBV treatment and bring renewed hope to millions of affected individuals worldwide.
L-HBsAg inhibitors are emerging as a promising class of therapeutic agents in the battle against chronic Hepatitis B Virus (HBV) infections. Chronic HBV infection remains a significant global health issue, affecting millions of people worldwide and leading to severe liver diseases, including cirrhosis and hepatocellular carcinoma. Efforts to develop effective treatments have led to the identification of various viral targets, among which the large hepatitis B surface antigen (L-HBsAg) stands out as a critical component. L-HBsAg inhibitors specifically target this viral protein, offering new hope for patients with chronic HBV.
How do L-HBsAg inhibitors work?
To understand how L-HBsAg inhibitors function, it is essential to grasp the role of the large hepatitis B surface antigen in the HBV life cycle. The HBV envelope contains three surface proteins: the small (S-HBsAg), middle (M-HBsAg), and large (L-HBsAg) antigens. L-HBsAg, with its unique preS1 domain, plays a crucial role in the initial attachment and entry of the virus into hepatocytes (liver cells). By binding to the sodium taurocholate co-transporting polypeptide (NTCP) receptor on the hepatocyte surface, L-HBsAg facilitates viral entry and subsequent infection.
L-HBsAg inhibitors work by binding to the L-HBsAg protein, thereby disrupting its interaction with the NTCP receptor. This inhibition prevents the virus from attaching to and entering liver cells, effectively blocking the early stages of the HBV life cycle. The precise mechanisms of inhibition can vary depending on the specific inhibitor, but the overarching goal remains the same: to prevent HBV from establishing infection within the host.
What are L-HBsAg inhibitors used for?
The primary use of L-HBsAg inhibitors lies in the treatment of chronic HBV infection. Traditional antiviral therapies, such as nucleos(t)ide analogues (NAs), focus on targeting the viral polymerase to suppress HBV replication. While these treatments can reduce viral load and slow disease progression, they often fall short of achieving a functional cure, where the virus is completely eradicated from the body. This is partly due to the persistence of covalently closed circular DNA (cccDNA), which acts as a reservoir for HBV replication and can remain unaffected by NAs.
L-HBsAg inhibitors offer an innovative approach by targeting a different stage of the viral life cycle. By preventing the virus from entering hepatocytes, these inhibitors can potentially reduce the establishment and replenishment of the cccDNA reservoir. This complementary mechanism of action holds promise for achieving higher rates of functional cure when used in combination with existing antivirals.
Moreover, L-HBsAg inhibitors may also play a role in addressing drug-resistant HBV strains. Resistance to nucleos(t)ide analogues is a growing concern in the management of chronic HBV, as mutations in the viral polymerase can render these drugs less effective. Since L-HBsAg inhibitors target a different viral protein, they provide an alternative therapeutic option that may retain efficacy against resistant strains, thereby enhancing the overall treatment arsenal.
In addition to their antiviral benefits, L-HBsAg inhibitors may help mitigate the immune-mediated liver damage often seen in chronic HBV infection. The chronic presence of HBV antigens, including L-HBsAg, can trigger an immune response that leads to liver inflammation and fibrosis. By reducing the levels of circulating L-HBsAg, these inhibitors may alleviate immune-mediated liver injury and improve overall liver health.
In conclusion, L-HBsAg inhibitors represent a novel and exciting avenue in the treatment of chronic HBV infection. By targeting the large hepatitis B surface antigen and disrupting viral entry, these inhibitors offer a complementary approach to existing therapies. Their potential to enhance functional cure rates, address drug-resistant strains, and mitigate liver damage makes them a promising addition to the arsenal against HBV. As research and clinical trials continue to advance, L-HBsAg inhibitors hold the potential to transform the landscape of HBV treatment and bring renewed hope to millions of affected individuals worldwide.
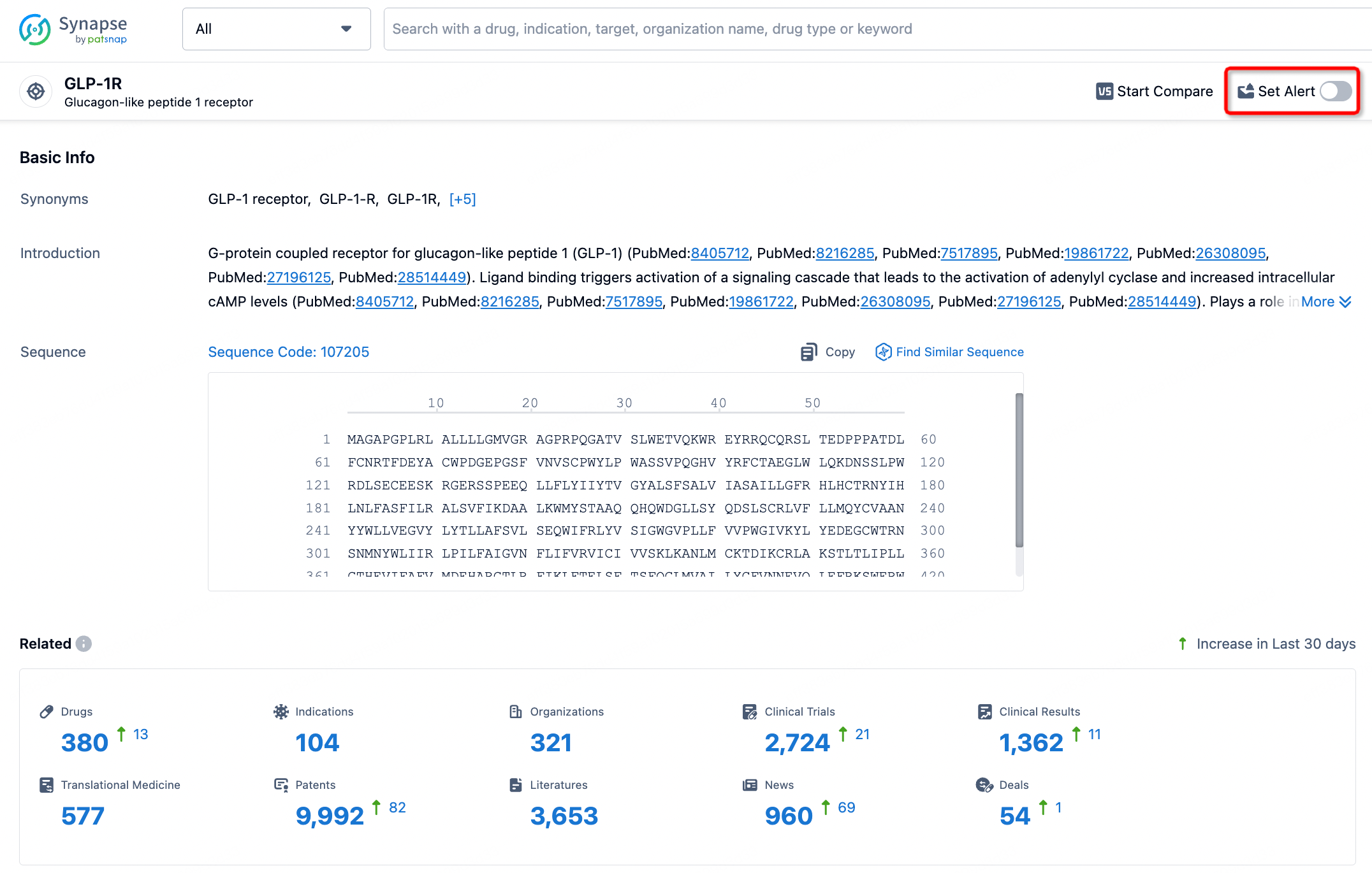
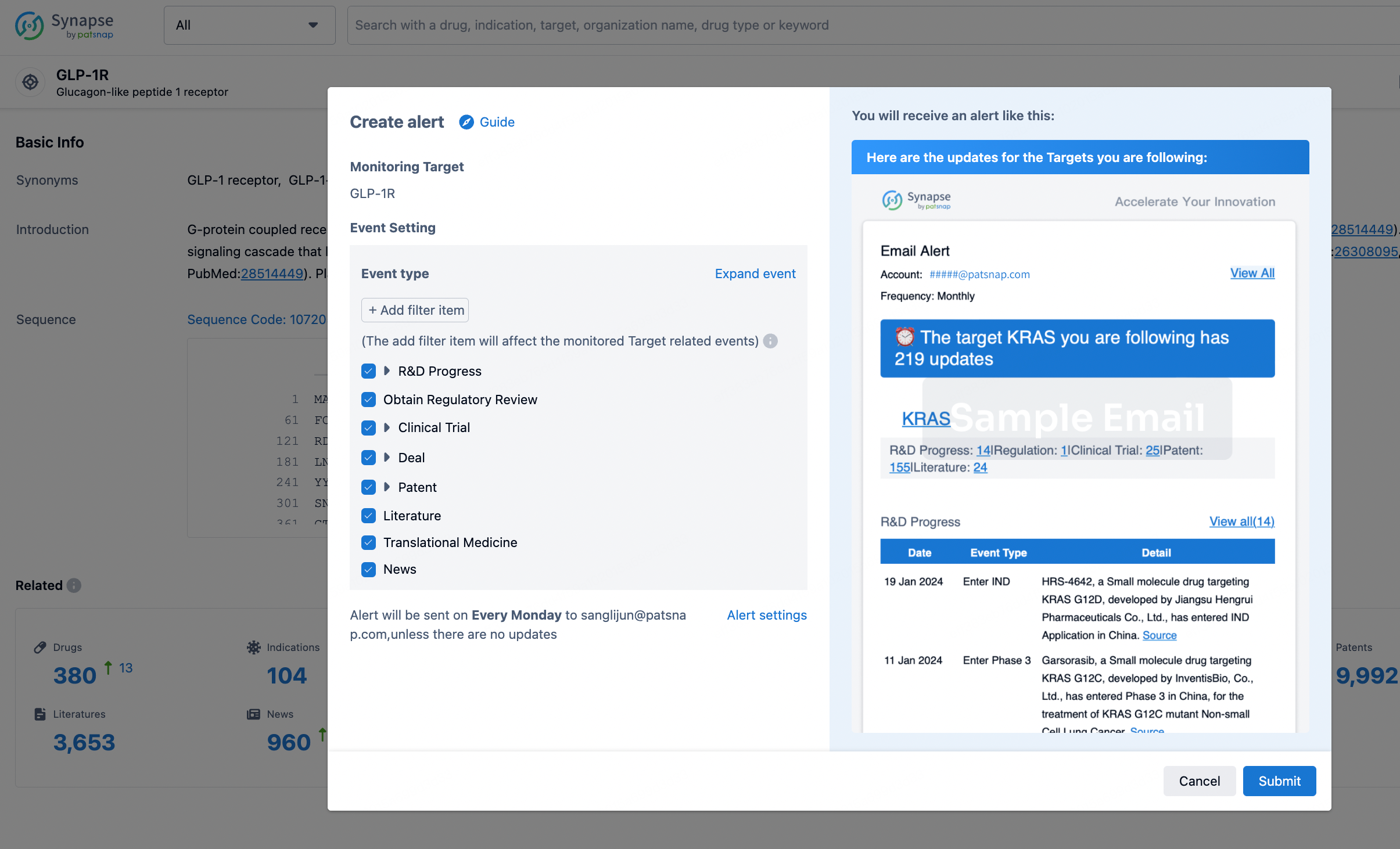
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.