Request Demo
What are miHAs inhibitors and how do they work?
25 June 2024
Minor Histocompatibility Antigens (miHAs) are small peptides derived from polymorphic proteins that can provoke immune responses in genetically divergent individuals. These antigens play a critical role in transplant immunology, specifically in bone marrow and stem cell transplantation. MiHAs inhibitors have emerged as a significant focus of research due to their potential to mediate graft-versus-host disease (GVHD) and improve transplantation outcomes. This blog post delves into what miHAs inhibitors are, how they function, and their current and potential applications.
Minor Histocompatibility Antigens (miHAs) are peptide fragments presented on the cell surface by major histocompatibility complex (MHC) molecules. Unlike major histocompatibility antigens, which are highly polymorphic and well-characterized, miHAs are less diverse but can still trigger substantial immune responses. When donor and recipient tissues in a transplant differ in their miHAs, the recipient's immune system can recognize these peptides as foreign. This recognition can lead to either beneficial graft-versus-tumor (GVT) effects or detrimental graft-versus-host disease (GVHD). The dual nature of miHAs makes them a focal point for strategies aimed at mitigating transplant-related complications while preserving anti-tumor activity.
MiHAs inhibitors work by targeting and neutralizing the specific miHAs responsible for adverse immune reactions. These inhibitors can take various forms, including small molecules, peptides, or monoclonal antibodies. The primary goal is to block the presentation or recognition of miHAs by the immune system. One strategy involves using small molecules that interfere with the processing and presentation of miHAs on MHC molecules. By preventing miHAs from being displayed on the cell surface, these inhibitors can reduce the likelihood of immune recognition and subsequent GVHD.
Another approach involves using monoclonal antibodies that specifically bind to miHAs. These antibodies can mask miHAs, rendering them invisible to T cells and preventing immune activation. Additionally, some inhibitors work by modulating the immune response itself, either by dampening the activity of T cells that recognize miHAs or by promoting regulatory T cells that can suppress adverse immune reactions.
The use of miHAs inhibitors has several potential applications, primarily in the field of transplantation. In bone marrow and stem cell transplants, one of the most significant complications is GVHD, where the donor's immune cells attack the recipient's tissues. By targeting the miHAs responsible for initiating this attack, miHAs inhibitors can significantly reduce the incidence and severity of GVHD. This would not only improve patient outcomes but also expand the pool of potential donors, as current matching criteria could be relaxed.
Another promising application is in enhancing graft-versus-tumor (GVT) effects without inducing GVHD. In many hematologic malignancies, the transplanted donor cells can attack residual cancer cells, leading to better long-term outcomes. However, this beneficial effect is often accompanied by the risk of GVHD. MiHAs inhibitors could potentially allow for selective suppression of GVHD while preserving or even enhancing GVT activity, offering a more targeted and effective post-transplant treatment strategy.
Furthermore, miHAs inhibitors hold promise beyond transplantation. They could be used in autoimmune diseases where the immune system erroneously targets the body's own tissues. By identifying and inhibiting specific miHAs involved in these autoimmune processes, it may be possible to develop new therapeutic strategies for conditions such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes.
In conclusion, miHAs inhibitors represent a burgeoning area of research with significant potential to transform the landscape of transplantation medicine and beyond. By selectively targeting the miHAs responsible for adverse immune reactions, these inhibitors offer the promise of reducing GVHD, enhancing GVT effects, and potentially treating autoimmune diseases. As our understanding of miHAs and their role in immune responses continues to deepen, the development of miHAs inhibitors could herald a new era of targeted, effective, and safer immunotherapies.
Minor Histocompatibility Antigens (miHAs) are peptide fragments presented on the cell surface by major histocompatibility complex (MHC) molecules. Unlike major histocompatibility antigens, which are highly polymorphic and well-characterized, miHAs are less diverse but can still trigger substantial immune responses. When donor and recipient tissues in a transplant differ in their miHAs, the recipient's immune system can recognize these peptides as foreign. This recognition can lead to either beneficial graft-versus-tumor (GVT) effects or detrimental graft-versus-host disease (GVHD). The dual nature of miHAs makes them a focal point for strategies aimed at mitigating transplant-related complications while preserving anti-tumor activity.
MiHAs inhibitors work by targeting and neutralizing the specific miHAs responsible for adverse immune reactions. These inhibitors can take various forms, including small molecules, peptides, or monoclonal antibodies. The primary goal is to block the presentation or recognition of miHAs by the immune system. One strategy involves using small molecules that interfere with the processing and presentation of miHAs on MHC molecules. By preventing miHAs from being displayed on the cell surface, these inhibitors can reduce the likelihood of immune recognition and subsequent GVHD.
Another approach involves using monoclonal antibodies that specifically bind to miHAs. These antibodies can mask miHAs, rendering them invisible to T cells and preventing immune activation. Additionally, some inhibitors work by modulating the immune response itself, either by dampening the activity of T cells that recognize miHAs or by promoting regulatory T cells that can suppress adverse immune reactions.
The use of miHAs inhibitors has several potential applications, primarily in the field of transplantation. In bone marrow and stem cell transplants, one of the most significant complications is GVHD, where the donor's immune cells attack the recipient's tissues. By targeting the miHAs responsible for initiating this attack, miHAs inhibitors can significantly reduce the incidence and severity of GVHD. This would not only improve patient outcomes but also expand the pool of potential donors, as current matching criteria could be relaxed.
Another promising application is in enhancing graft-versus-tumor (GVT) effects without inducing GVHD. In many hematologic malignancies, the transplanted donor cells can attack residual cancer cells, leading to better long-term outcomes. However, this beneficial effect is often accompanied by the risk of GVHD. MiHAs inhibitors could potentially allow for selective suppression of GVHD while preserving or even enhancing GVT activity, offering a more targeted and effective post-transplant treatment strategy.
Furthermore, miHAs inhibitors hold promise beyond transplantation. They could be used in autoimmune diseases where the immune system erroneously targets the body's own tissues. By identifying and inhibiting specific miHAs involved in these autoimmune processes, it may be possible to develop new therapeutic strategies for conditions such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes.
In conclusion, miHAs inhibitors represent a burgeoning area of research with significant potential to transform the landscape of transplantation medicine and beyond. By selectively targeting the miHAs responsible for adverse immune reactions, these inhibitors offer the promise of reducing GVHD, enhancing GVT effects, and potentially treating autoimmune diseases. As our understanding of miHAs and their role in immune responses continues to deepen, the development of miHAs inhibitors could herald a new era of targeted, effective, and safer immunotherapies.
How to obtain the latest development progress of all targets?
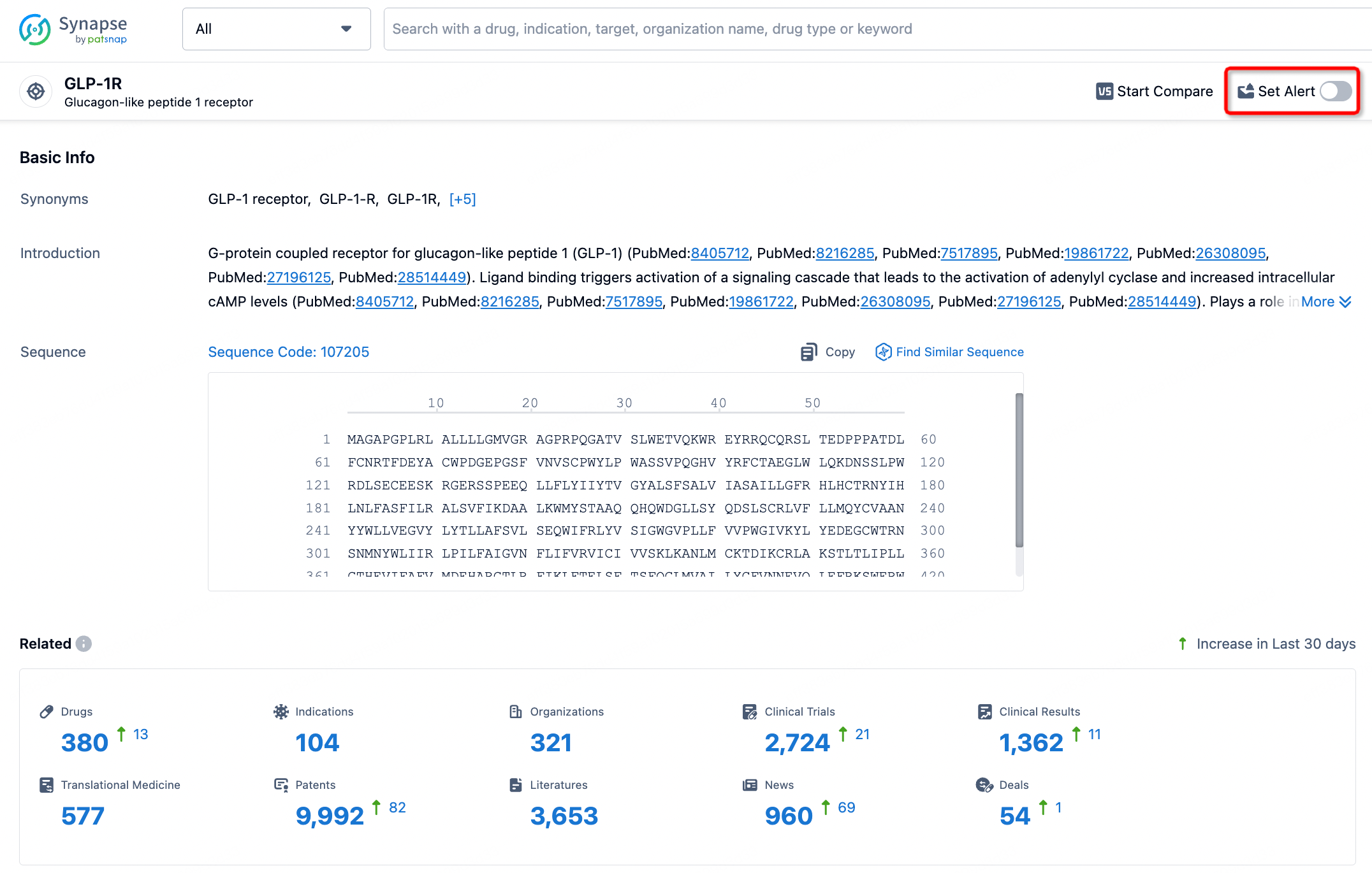
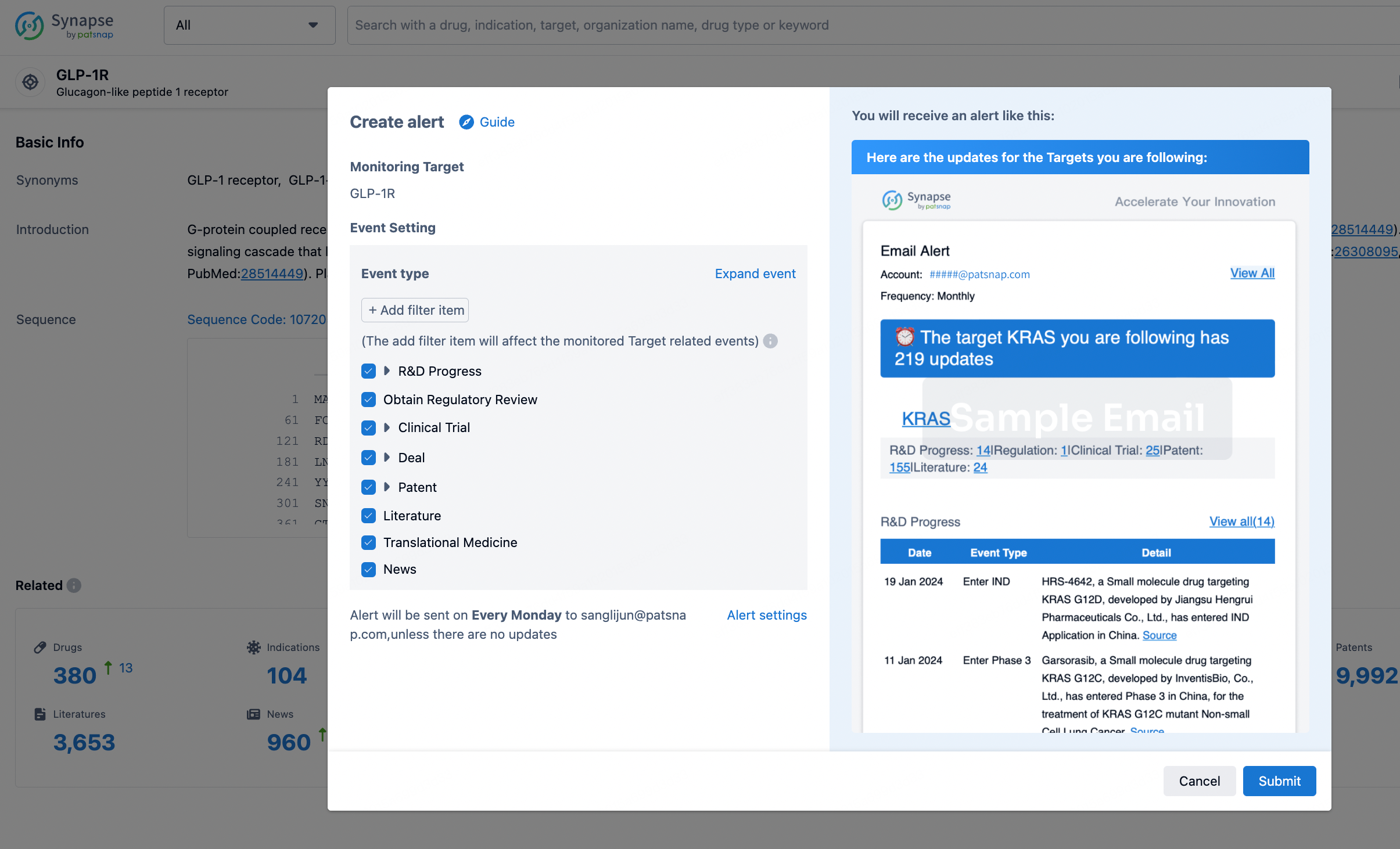
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.