Request Demo
What are Poly-N-acetyl glucosamine inhibitors and how do they work?
26 June 2024
Poly-N-acetyl glucosamine (PNAG) inhibitors represent a promising frontier in medical and pharmaceutical research. PNAG is a polysaccharide molecule found in the biofilm of various pathogenic bacteria. This biofilm plays a crucial role in the bacteria's ability to evade the host's immune system and resist antibiotic treatments. As such, PNAG inhibitors have garnered significant attention for their potential to disrupt bacterial biofilm formation, thereby enhancing the efficacy of existing antibiotics and improving patient outcomes.
Biofilms are complex structures that protect bacteria from environmental stressors, including the host's immune defenses and antimicrobial agents. The ability of biofilms to confer resistance to treatment is a significant challenge in managing bacterial infections, particularly chronic and recurrent infections. By targeting PNAG, researchers aim to dismantle these biofilms and render bacteria more susceptible to eradication by the immune system and antibiotics.
The development of PNAG inhibitors has opened new avenues for combating bacterial infections. These inhibitors are designed to specifically target and degrade PNAG, thereby disrupting the integrity of the biofilm. This disruption can significantly reduce the bacteria's ability to adhere to surfaces, form colonies, and protect themselves from hostile environments. As a result, PNAG inhibitors can enhance the effectiveness of conventional antibiotics and potentially reduce the duration and severity of bacterial infections.
One of the key mechanisms by which PNAG inhibitors work is by preventing the synthesis or promoting the degradation of PNAG. This can be achieved through various means, such as enzymatic degradation or chemical inhibition. Enzymatic degradation involves the use of enzymes that specifically break down PNAG into smaller, non-functional components. Chemical inhibition, on the other hand, involves the use of small molecules that interfere with the biosynthesis of PNAG by inhibiting the enzymes responsible for its production.
By targeting PNAG, these inhibitors can disrupt the formation and maintenance of bacterial biofilms. This can lead to the detachment of bacteria from surfaces, making them more susceptible to antimicrobial agents and the host's immune response. Additionally, the breakdown of biofilms can prevent the recurrence of infections by reducing the reservoir of bacteria that can cause reinfection.
PNAG inhibitors have shown promise in preclinical studies and animal models. For example, studies have demonstrated that PNAG inhibitors can enhance the efficacy of antibiotics against biofilm-associated infections, such as those caused by Staphylococcus aureus and Pseudomonas aeruginosa. These findings suggest that PNAG inhibitors could be used as adjunctive therapies to improve the outcomes of antibiotic treatments.
One of the primary applications of PNAG inhibitors is in the treatment of chronic and recurrent bacterial infections. These infections are often difficult to manage due to the presence of biofilms, which protect the bacteria from antibiotics and the host's immune system. By disrupting the biofilms, PNAG inhibitors can enhance the effectiveness of antibiotics and improve patient outcomes. This is particularly important in the treatment of infections associated with medical devices, such as catheters and prosthetic implants, where biofilms are a common cause of treatment failure.
PNAG inhibitors also have potential applications in the prevention of biofilm formation on medical devices. By coating the surfaces of these devices with PNAG inhibitors, it may be possible to prevent the initial adhesion and colonization of bacteria, thereby reducing the risk of infection. This approach could be particularly beneficial in hospital settings, where the use of medical devices is common and the risk of infection is high.
In addition to their potential in treating and preventing bacterial infections, PNAG inhibitors may also have applications in other areas of medicine. For example, they could be used in the treatment of chronic wounds, where biofilms are a common impediment to healing. By disrupting the biofilms, PNAG inhibitors could promote wound healing and reduce the risk of infection.
In conclusion, PNAG inhibitors represent a promising approach to combating bacterial infections, particularly those involving biofilms. By targeting PNAG, these inhibitors can disrupt the formation and maintenance of biofilms, enhancing the effectiveness of antibiotics and improving patient outcomes. As research in this area continues to advance, PNAG inhibitors could become an important tool in the fight against bacterial infections and the growing problem of antibiotic resistance.
Biofilms are complex structures that protect bacteria from environmental stressors, including the host's immune defenses and antimicrobial agents. The ability of biofilms to confer resistance to treatment is a significant challenge in managing bacterial infections, particularly chronic and recurrent infections. By targeting PNAG, researchers aim to dismantle these biofilms and render bacteria more susceptible to eradication by the immune system and antibiotics.
The development of PNAG inhibitors has opened new avenues for combating bacterial infections. These inhibitors are designed to specifically target and degrade PNAG, thereby disrupting the integrity of the biofilm. This disruption can significantly reduce the bacteria's ability to adhere to surfaces, form colonies, and protect themselves from hostile environments. As a result, PNAG inhibitors can enhance the effectiveness of conventional antibiotics and potentially reduce the duration and severity of bacterial infections.
One of the key mechanisms by which PNAG inhibitors work is by preventing the synthesis or promoting the degradation of PNAG. This can be achieved through various means, such as enzymatic degradation or chemical inhibition. Enzymatic degradation involves the use of enzymes that specifically break down PNAG into smaller, non-functional components. Chemical inhibition, on the other hand, involves the use of small molecules that interfere with the biosynthesis of PNAG by inhibiting the enzymes responsible for its production.
By targeting PNAG, these inhibitors can disrupt the formation and maintenance of bacterial biofilms. This can lead to the detachment of bacteria from surfaces, making them more susceptible to antimicrobial agents and the host's immune response. Additionally, the breakdown of biofilms can prevent the recurrence of infections by reducing the reservoir of bacteria that can cause reinfection.
PNAG inhibitors have shown promise in preclinical studies and animal models. For example, studies have demonstrated that PNAG inhibitors can enhance the efficacy of antibiotics against biofilm-associated infections, such as those caused by Staphylococcus aureus and Pseudomonas aeruginosa. These findings suggest that PNAG inhibitors could be used as adjunctive therapies to improve the outcomes of antibiotic treatments.
One of the primary applications of PNAG inhibitors is in the treatment of chronic and recurrent bacterial infections. These infections are often difficult to manage due to the presence of biofilms, which protect the bacteria from antibiotics and the host's immune system. By disrupting the biofilms, PNAG inhibitors can enhance the effectiveness of antibiotics and improve patient outcomes. This is particularly important in the treatment of infections associated with medical devices, such as catheters and prosthetic implants, where biofilms are a common cause of treatment failure.
PNAG inhibitors also have potential applications in the prevention of biofilm formation on medical devices. By coating the surfaces of these devices with PNAG inhibitors, it may be possible to prevent the initial adhesion and colonization of bacteria, thereby reducing the risk of infection. This approach could be particularly beneficial in hospital settings, where the use of medical devices is common and the risk of infection is high.
In addition to their potential in treating and preventing bacterial infections, PNAG inhibitors may also have applications in other areas of medicine. For example, they could be used in the treatment of chronic wounds, where biofilms are a common impediment to healing. By disrupting the biofilms, PNAG inhibitors could promote wound healing and reduce the risk of infection.
In conclusion, PNAG inhibitors represent a promising approach to combating bacterial infections, particularly those involving biofilms. By targeting PNAG, these inhibitors can disrupt the formation and maintenance of biofilms, enhancing the effectiveness of antibiotics and improving patient outcomes. As research in this area continues to advance, PNAG inhibitors could become an important tool in the fight against bacterial infections and the growing problem of antibiotic resistance.
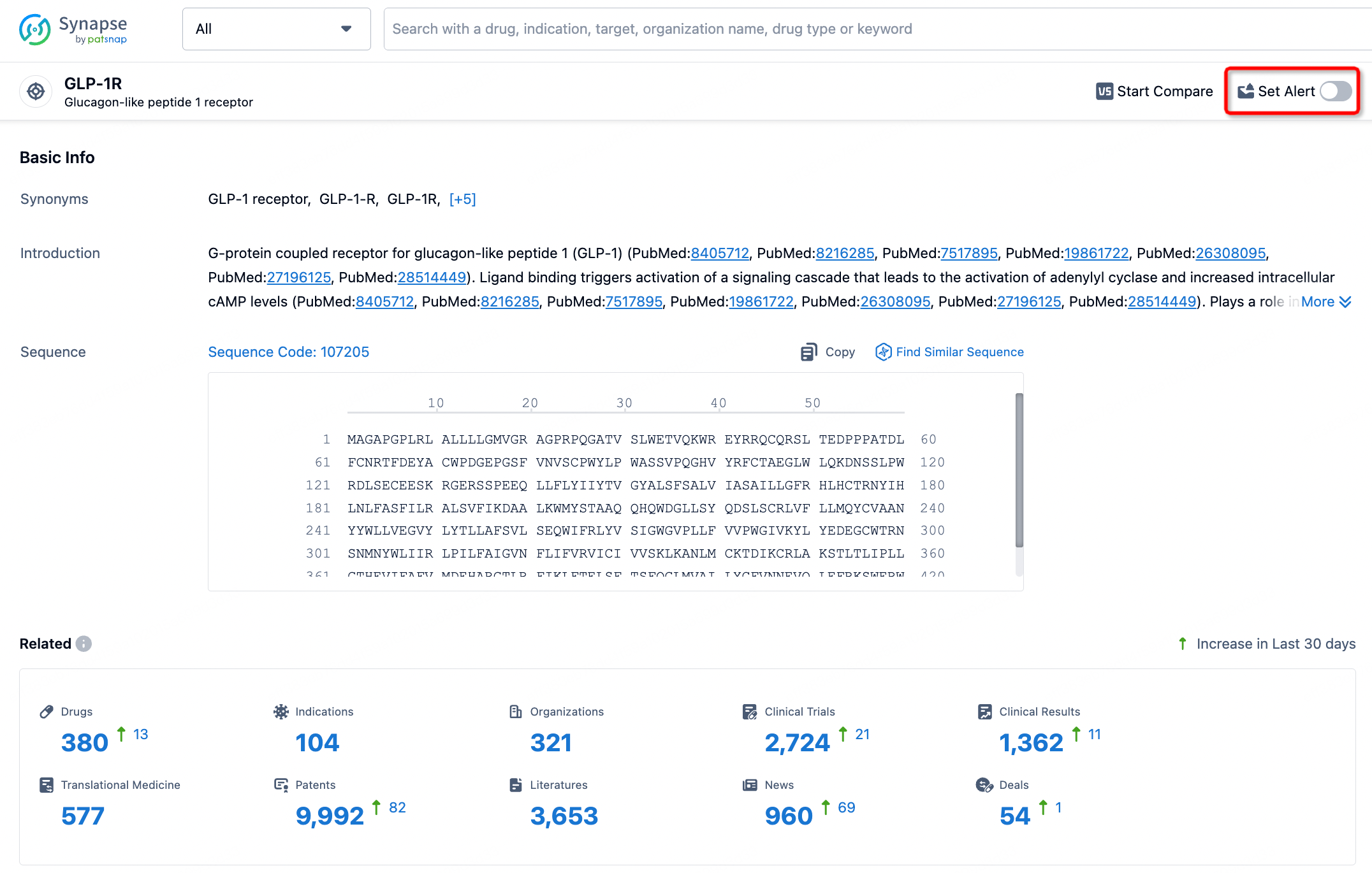
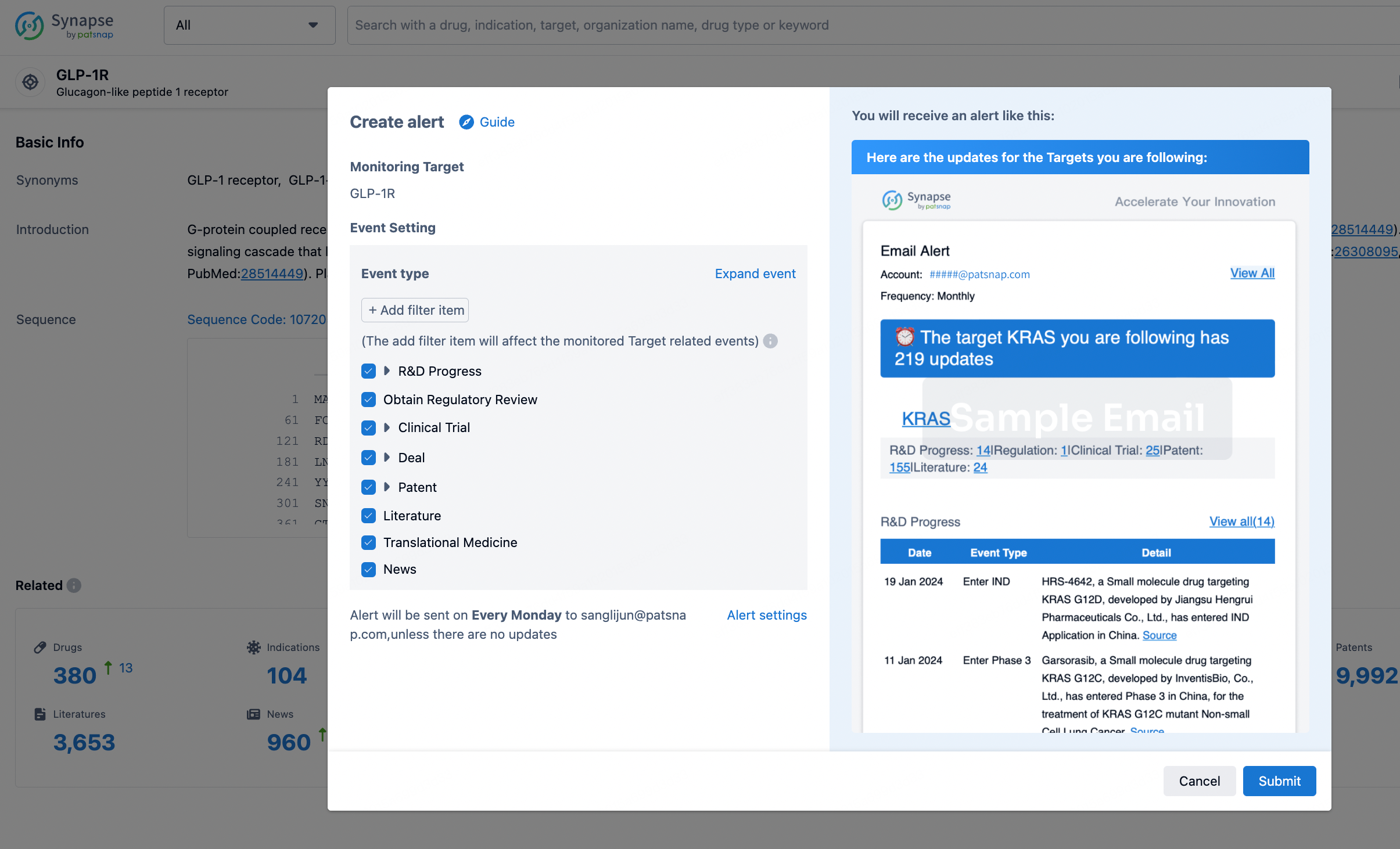
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.