Request Demo
What are PslG inhibitors and how do they work?
26 June 2024
PslG inhibitors are emerging as a promising area of research in the fight against bacterial infections, particularly those caused by biofilm-forming bacteria such as Pseudomonas aeruginosa. Biofilms are complex communities of bacteria that adhere to surfaces and are encased in a protective matrix. This matrix makes the bacteria highly resistant to antibiotics and the immune system, posing a significant challenge in treating infections. PslG inhibitors target the Psl polysaccharide, a key component of the biofilm matrix in Pseudomonas aeruginosa, thereby offering a novel approach to combating these stubborn infections.
How do PslG inhibitors work?
To understand the mechanism of PslG inhibitors, it is essential to first comprehend the role of the Psl polysaccharide in biofilm formation. Psl is one of the primary exopolysaccharides produced by Pseudomonas aeruginosa and plays a critical role in the initial stages of biofilm development, cell-cell adhesion, and maintaining the biofilm's structural integrity.
PslG is an enzyme naturally produced by Pseudomonas aeruginosa that specifically degrades the Psl polysaccharide. The enzyme cleaves the polysaccharide chains, thereby disrupting the biofilm matrix. Researchers have discovered that inhibiting PslG can prevent the degradation of Psl, thus hindering the bacterium’s ability to form and maintain biofilms.
PslG inhibitors are designed to bind to the PslG enzyme and block its activity. By inhibiting PslG, these compounds prevent the enzymatic breakdown of Psl polysaccharides, which results in weaker biofilm structures that are more susceptible to antibiotic treatment and immune clearance. In essence, PslG inhibitors do not kill the bacteria directly; instead, they render the biofilm more vulnerable and easier to eradicate.
What are PslG inhibitors used for?
The primary application of PslG inhibitors lies in the treatment of chronic and hard-to-treat bacterial infections. One of the most significant clinical challenges is the treatment of infections caused by biofilm-forming bacteria, which are notorious for their resistance to conventional antibiotics. Pseudomonas aeruginosa is a prime example, often associated with chronic infections in cystic fibrosis patients, burn wounds, chronic wounds, and medical device-related infections, such as those involving catheters and prosthetic implants.
PslG inhibitors have the potential to revolutionize the treatment of these infections by dismantling the biofilm’s protective barrier. This approach can enhance the efficacy of existing antibiotics, allowing them to penetrate the biofilm and kill the encased bacteria. Consequently, patients may require lower doses of antibiotics, reducing the risk of side effects and the development of antibiotic resistance.
Moreover, PslG inhibitors can be used prophylactically to prevent biofilm formation on medical devices. For instance, incorporating PslG inhibitors into the coatings of catheters, stents, and implants could significantly reduce the incidence of device-related infections. This preventive measure is particularly crucial in hospital settings, where biofilm-associated infections can lead to severe complications and extended hospital stays.
Another promising application of PslG inhibitors is in the field of wound care. Chronic wounds, such as diabetic foot ulcers and pressure sores, are often complicated by biofilm infections that impede healing. By disrupting the biofilm matrix, PslG inhibitors can promote more effective wound healing and reduce the risk of infection-related complications.
In conclusion, PslG inhibitors represent a novel and innovative approach to addressing the challenges posed by biofilm-associated bacterial infections. By targeting the structural integrity of biofilms, these inhibitors can enhance the efficacy of antibiotic treatments and offer new possibilities for preventing and managing chronic infections. As research in this area continues to advance, PslG inhibitors hold the promise of improving patient outcomes and reducing the burden of biofilm-related infections in clinical settings.
How do PslG inhibitors work?
To understand the mechanism of PslG inhibitors, it is essential to first comprehend the role of the Psl polysaccharide in biofilm formation. Psl is one of the primary exopolysaccharides produced by Pseudomonas aeruginosa and plays a critical role in the initial stages of biofilm development, cell-cell adhesion, and maintaining the biofilm's structural integrity.
PslG is an enzyme naturally produced by Pseudomonas aeruginosa that specifically degrades the Psl polysaccharide. The enzyme cleaves the polysaccharide chains, thereby disrupting the biofilm matrix. Researchers have discovered that inhibiting PslG can prevent the degradation of Psl, thus hindering the bacterium’s ability to form and maintain biofilms.
PslG inhibitors are designed to bind to the PslG enzyme and block its activity. By inhibiting PslG, these compounds prevent the enzymatic breakdown of Psl polysaccharides, which results in weaker biofilm structures that are more susceptible to antibiotic treatment and immune clearance. In essence, PslG inhibitors do not kill the bacteria directly; instead, they render the biofilm more vulnerable and easier to eradicate.
What are PslG inhibitors used for?
The primary application of PslG inhibitors lies in the treatment of chronic and hard-to-treat bacterial infections. One of the most significant clinical challenges is the treatment of infections caused by biofilm-forming bacteria, which are notorious for their resistance to conventional antibiotics. Pseudomonas aeruginosa is a prime example, often associated with chronic infections in cystic fibrosis patients, burn wounds, chronic wounds, and medical device-related infections, such as those involving catheters and prosthetic implants.
PslG inhibitors have the potential to revolutionize the treatment of these infections by dismantling the biofilm’s protective barrier. This approach can enhance the efficacy of existing antibiotics, allowing them to penetrate the biofilm and kill the encased bacteria. Consequently, patients may require lower doses of antibiotics, reducing the risk of side effects and the development of antibiotic resistance.
Moreover, PslG inhibitors can be used prophylactically to prevent biofilm formation on medical devices. For instance, incorporating PslG inhibitors into the coatings of catheters, stents, and implants could significantly reduce the incidence of device-related infections. This preventive measure is particularly crucial in hospital settings, where biofilm-associated infections can lead to severe complications and extended hospital stays.
Another promising application of PslG inhibitors is in the field of wound care. Chronic wounds, such as diabetic foot ulcers and pressure sores, are often complicated by biofilm infections that impede healing. By disrupting the biofilm matrix, PslG inhibitors can promote more effective wound healing and reduce the risk of infection-related complications.
In conclusion, PslG inhibitors represent a novel and innovative approach to addressing the challenges posed by biofilm-associated bacterial infections. By targeting the structural integrity of biofilms, these inhibitors can enhance the efficacy of antibiotic treatments and offer new possibilities for preventing and managing chronic infections. As research in this area continues to advance, PslG inhibitors hold the promise of improving patient outcomes and reducing the burden of biofilm-related infections in clinical settings.
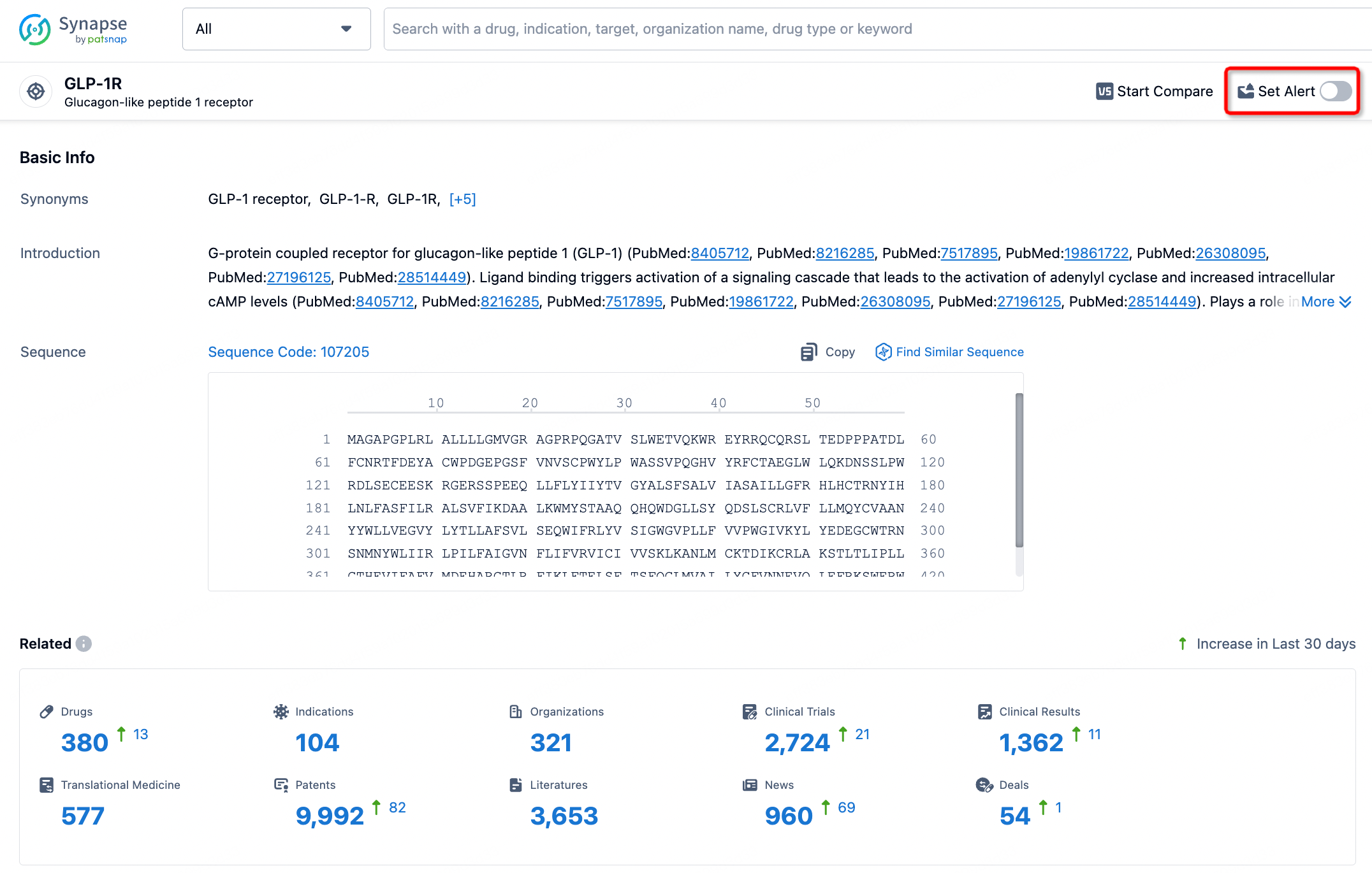
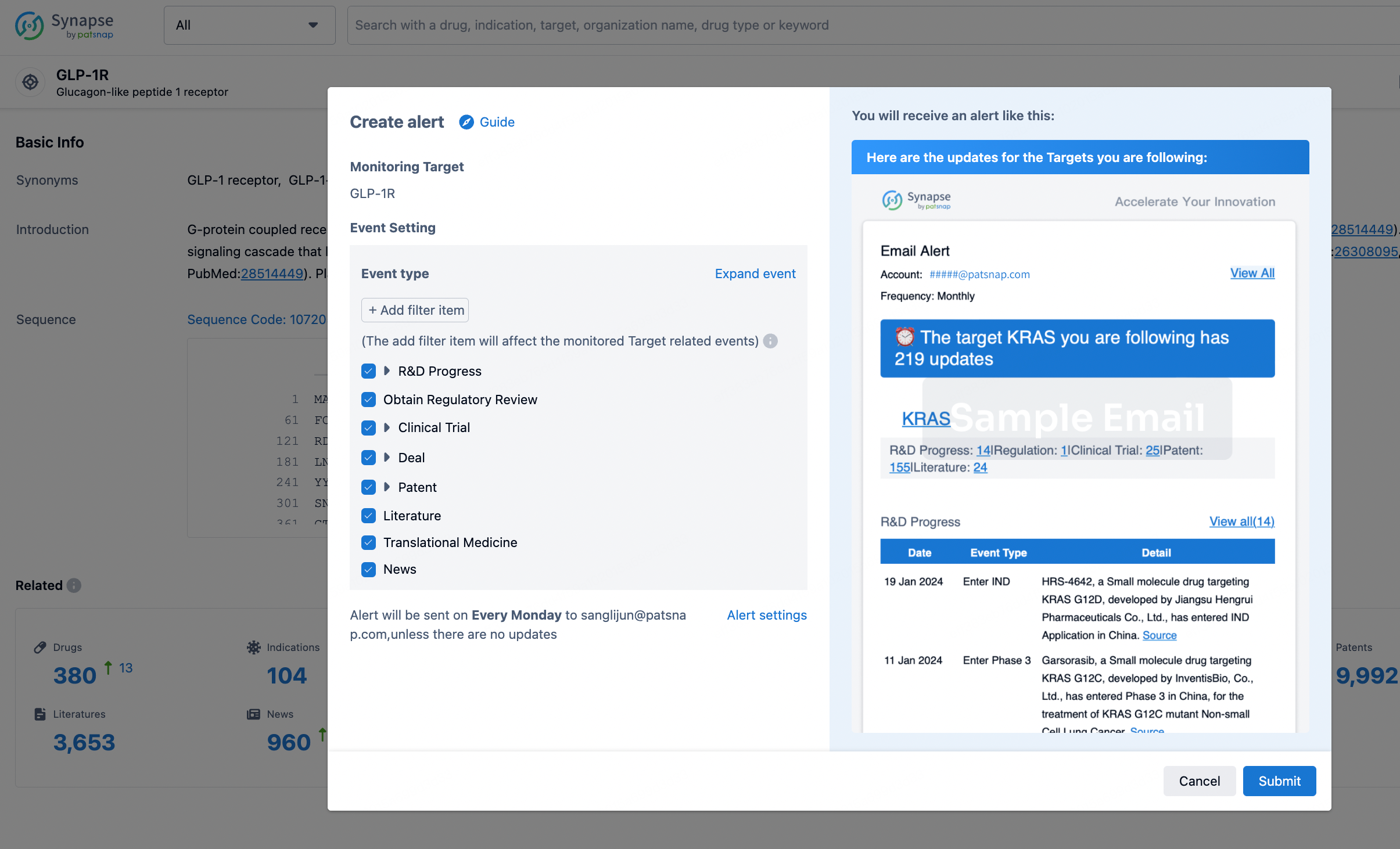
How to obtain the latest development progress of all targets?
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.