Request Demo
What are SGSH replacements and how do they work?
25 June 2024
In the dynamic and ever-evolving field of pharmaceuticals and biotechnology, breakthroughs in drug development and metabolic engineering continually offer new hope and improved outcomes for patients with rare and debilitating conditions. One such area that has garnered significant attention is the development of SGSH replacements. SGSH, or N-sulfoglucosamine sulfohydrolase, is a crucial enzyme in the human body. Deficiency in this enzyme leads to mucopolysaccharidosis type IIIA (MPS IIIA), commonly known as Sanfilippo syndrome type A. This rare genetic disorder results in the accumulation of heparan sulfate, a substance that adversely affects cellular function, leading to severe neurological and systemic symptoms. This blog aims to demystify SGSH replacements, how they function, and their pivotal role in treating MPS IIIA.
SGSH replacements work on a relatively straightforward principle: supplementing or enhancing the deficient enzyme in patients with MPS IIIA. In healthy individuals, SGSH is involved in the degradation of heparan sulfate, a glycosaminoglycan. When SGSH is defective or absent, heparan sulfate accumulates, causing progressive cellular and tissue damage. SGSH replacements aim to restore this enzymatic function, thereby reducing the accumulation of heparan sulfate and mitigating the symptoms of MPS IIIA.
There are several approaches to SGSH replacement therapy. One of the most common strategies is enzyme replacement therapy (ERT), where the missing or malfunctioning enzyme is introduced into the patient's body through intravenous infusion. The exogenous enzyme can then be taken up by cells and transported to lysosomes, where it degrades heparan sulfate. Another promising approach is gene therapy, which involves introducing a functional copy of the SGSH gene into the patient’s cells, enabling them to produce the enzyme endogenously. This can be achieved through various vectors, including adeno-associated viruses (AAVs). Additionally, substrate reduction therapy (SRT) focuses on decreasing the synthesis of heparan sulfate to balance its accumulation and degradation. Each of these strategies has its own set of advantages and challenges, but collectively they offer a multifaceted approach to tackling MPS IIIA.
SGSH replacements are primarily used to address the debilitating symptoms associated with MPS IIIA. The condition is characterized by severe neurological manifestations, including developmental delay, cognitive decline, hyperactivity, and profound sleep disturbances. Over time, affected individuals may also experience hearing loss, vision problems, and skeletal abnormalities. By restoring SGSH activity, replacement therapies aim to prevent or reduce the accumulation of heparan sulfate, thereby slowing or halting the progression of these symptoms.
In clinical practice, the ultimate goals of SGSH replacement therapies are to improve the quality of life, extend life expectancy, and enhance neurological function for patients with MPS IIIA. For instance, ERT has shown promise in reducing heparan sulfate levels in the cerebrospinal fluid and peripheral tissues, which can translate to a slower progression of neurological symptoms. Gene therapy, still largely in experimental stages, holds the potential for a more permanent solution by enabling continuous production of SGSH within the patient’s cells. Some early-stage clinical trials have demonstrated improvements in motor function and cognitive abilities, offering a glimmer of hope for affected families.
Beyond the immediate clinical benefits, SGSH replacements also pave the way for advancements in our understanding of lysosomal storage disorders and the development of novel therapeutic approaches. The success of SGSH replacements could stimulate further research into combination therapies that address multiple pathways involved in MPS IIIA, potentially leading to even more effective treatments.
In conclusion, SGSH replacements represent a significant step forward in the treatment of Sanfilippo syndrome type A. By supplementing or enhancing the deficient enzyme, these therapies have the potential to mitigate the severe symptoms of MPS IIIA and vastly improve the quality of life for patients. As research continues to progress, it is hoped that these treatments will become more accessible and effective, offering new avenues of hope for those affected by this challenging condition.
SGSH replacements work on a relatively straightforward principle: supplementing or enhancing the deficient enzyme in patients with MPS IIIA. In healthy individuals, SGSH is involved in the degradation of heparan sulfate, a glycosaminoglycan. When SGSH is defective or absent, heparan sulfate accumulates, causing progressive cellular and tissue damage. SGSH replacements aim to restore this enzymatic function, thereby reducing the accumulation of heparan sulfate and mitigating the symptoms of MPS IIIA.
There are several approaches to SGSH replacement therapy. One of the most common strategies is enzyme replacement therapy (ERT), where the missing or malfunctioning enzyme is introduced into the patient's body through intravenous infusion. The exogenous enzyme can then be taken up by cells and transported to lysosomes, where it degrades heparan sulfate. Another promising approach is gene therapy, which involves introducing a functional copy of the SGSH gene into the patient’s cells, enabling them to produce the enzyme endogenously. This can be achieved through various vectors, including adeno-associated viruses (AAVs). Additionally, substrate reduction therapy (SRT) focuses on decreasing the synthesis of heparan sulfate to balance its accumulation and degradation. Each of these strategies has its own set of advantages and challenges, but collectively they offer a multifaceted approach to tackling MPS IIIA.
SGSH replacements are primarily used to address the debilitating symptoms associated with MPS IIIA. The condition is characterized by severe neurological manifestations, including developmental delay, cognitive decline, hyperactivity, and profound sleep disturbances. Over time, affected individuals may also experience hearing loss, vision problems, and skeletal abnormalities. By restoring SGSH activity, replacement therapies aim to prevent or reduce the accumulation of heparan sulfate, thereby slowing or halting the progression of these symptoms.
In clinical practice, the ultimate goals of SGSH replacement therapies are to improve the quality of life, extend life expectancy, and enhance neurological function for patients with MPS IIIA. For instance, ERT has shown promise in reducing heparan sulfate levels in the cerebrospinal fluid and peripheral tissues, which can translate to a slower progression of neurological symptoms. Gene therapy, still largely in experimental stages, holds the potential for a more permanent solution by enabling continuous production of SGSH within the patient’s cells. Some early-stage clinical trials have demonstrated improvements in motor function and cognitive abilities, offering a glimmer of hope for affected families.
Beyond the immediate clinical benefits, SGSH replacements also pave the way for advancements in our understanding of lysosomal storage disorders and the development of novel therapeutic approaches. The success of SGSH replacements could stimulate further research into combination therapies that address multiple pathways involved in MPS IIIA, potentially leading to even more effective treatments.
In conclusion, SGSH replacements represent a significant step forward in the treatment of Sanfilippo syndrome type A. By supplementing or enhancing the deficient enzyme, these therapies have the potential to mitigate the severe symptoms of MPS IIIA and vastly improve the quality of life for patients. As research continues to progress, it is hoped that these treatments will become more accessible and effective, offering new avenues of hope for those affected by this challenging condition.
How to obtain the latest development progress of all targets?
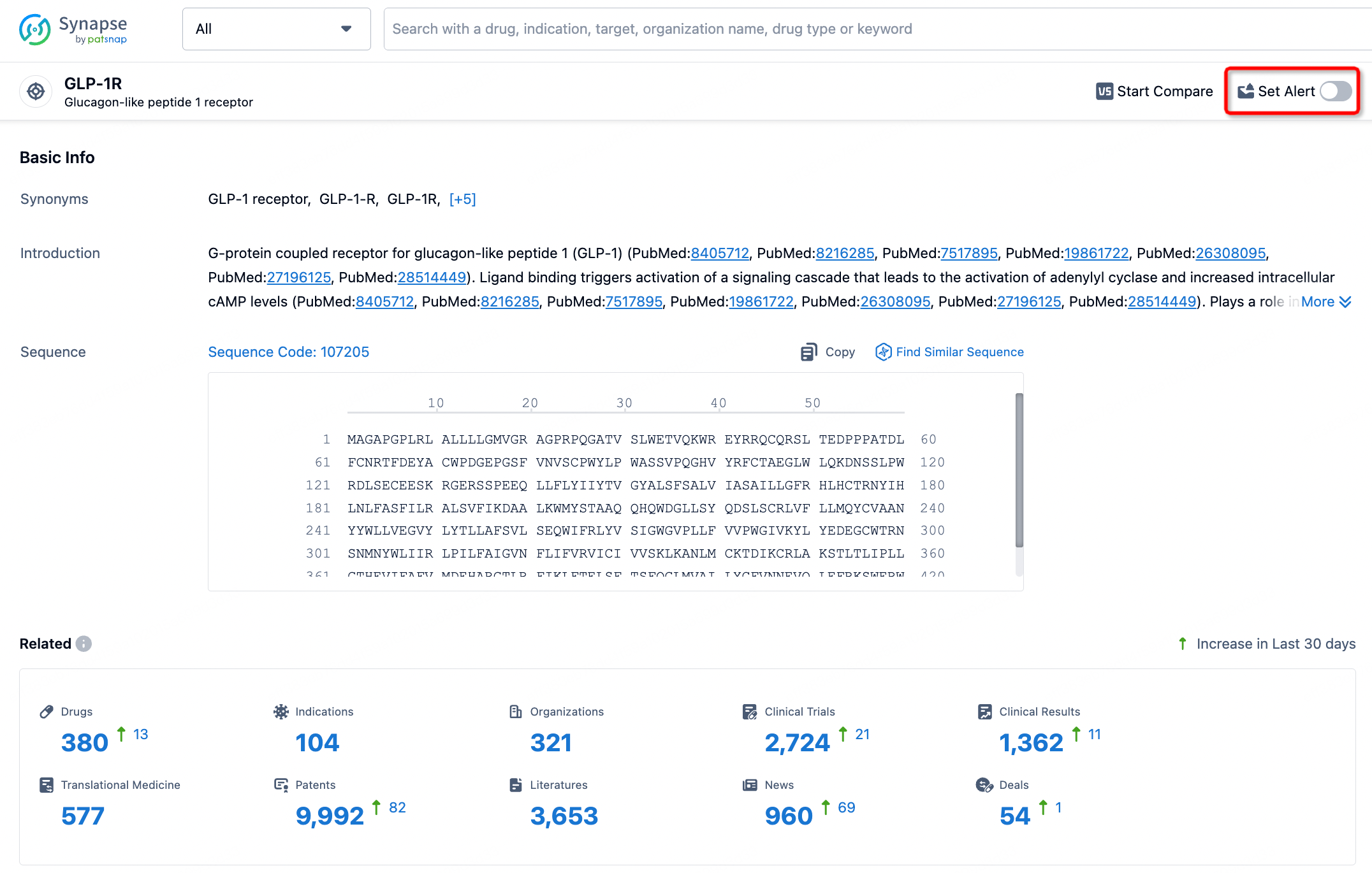
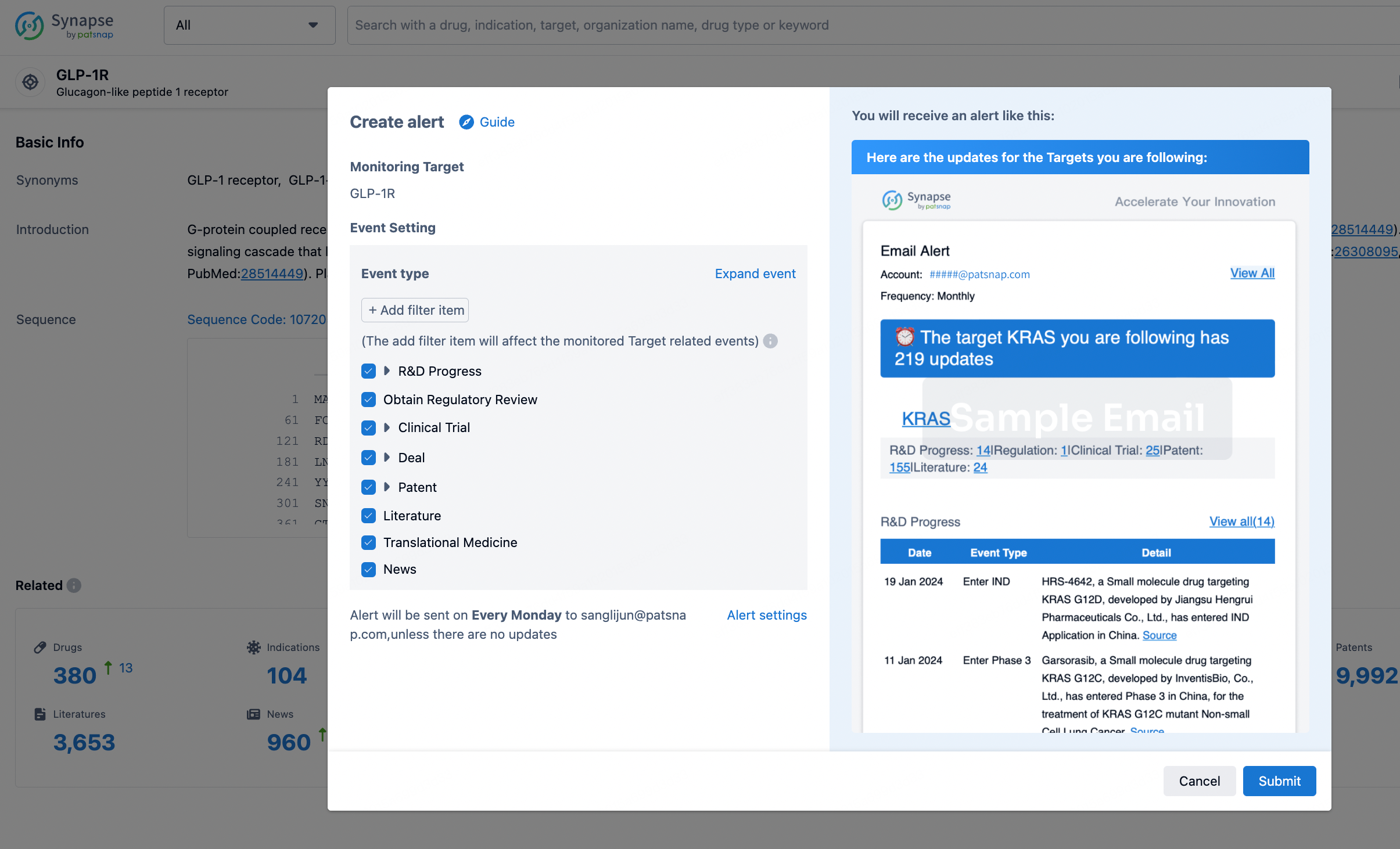
In the Synapse database, you can stay updated on the latest research and development advances of all targets. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.