Request Demo
What is the difference between live-attenuated and inactivated vaccines?
28 May 2025
Introduction
Vaccination has been a cornerstone in preventing infectious diseases, significantly reducing morbidity and mortality worldwide. Understanding the different types of vaccines is crucial for grasping how they work and their implications for public health. Two well-known types are live-attenuated vaccines and inactivated vaccines. This blog explores the differences between these two vaccine types, their mechanisms, applications, and considerations.
Live-Attenuated Vaccines
What Are Live-Attenuated Vaccines?
Live-attenuated vaccines contain versions of the living virus or bacteria that have been weakened under laboratory conditions. These pathogens are made less virulent, meaning they cannot cause the disease in healthy individuals but still provoke a strong immune response.
Mechanism of Action
When administered, live-attenuated vaccines mimic a natural infection, stimulating the immune system by producing a robust cellular and antibody-mediated response. Since they closely resemble the natural infection, the immune system gets a comprehensive picture of the pathogen, which leads to long-lasting immunity.
Benefits and Applications
Live-attenuated vaccines often provide lifelong immunity with just one or two doses. They have been used successfully for diseases such as measles, mumps, rubella (MMR), and chickenpox. The strong immune response they elicit is particularly beneficial in controlling outbreaks and providing community protection.
Considerations and Limitations
These vaccines are generally not suitable for individuals with weakened immune systems, such as those undergoing chemotherapy or living with HIV/AIDS. There is a small risk that the weakened virus could mutate back to a more virulent form, although this is extremely rare. Additionally, live-attenuated vaccines require careful storage and handling to maintain their efficacy.
Inactivated Vaccines
What Are Inactivated Vaccines?
Inactivated vaccines consist of viruses or bacteria that have been killed so that they cannot replicate or cause disease. These vaccines use various methods to inactivate the pathogen, such as heat, chemicals, or radiation.
Mechanism of Action
By introducing inactivated pathogens, the vaccine stimulates the immune system to recognize the pathogen and mount an immune response. However, since the pathogen is not alive, the immune response is generally less robust compared to live-attenuated vaccines, often necessitating booster shots.
Benefits and Applications
Inactivated vaccines are safe for individuals with compromised immune systems, as they cannot cause infection. They are used widely for diseases like influenza, hepatitis A, and rabies. These vaccines are stable and can be stored easily, which makes them accessible in various settings, including those with limited refrigeration facilities.
Considerations and Limitations
Inactivated vaccines typically require multiple doses and booster shots to maintain immunity. The immune response might not be as strong or long-lasting as that from live-attenuated vaccines, potentially requiring more frequent updates to vaccine formulations, particularly in the case of rapidly mutating viruses like influenza.
Comparative Analysis
Efficacy
Live-attenuated vaccines generally provoke stronger and longer-lasting immune responses, often with fewer doses required. In contrast, inactivated vaccines might need multiple doses and booster shots to sustain protection.
Safety
Inactivated vaccines are safer for immunocompromised individuals. Live-attenuated vaccines, while effective, are generally contraindicated in these populations due to the risk, however minimal, of causing illness.
Storage and Handling
Live-attenuated vaccines need stringent storage conditions to maintain their viability, typically requiring refrigeration. Inactivated vaccines, being more stable, are easier to store and handle.
Conclusion
Both live-attenuated and inactivated vaccines play crucial roles in preventing infectious diseases. Their differences highlight the importance of understanding vaccine types to make informed decisions about vaccination strategies. Each type has its unique advantages and considerations, shaping its use in various contexts and among different populations. As science progresses, continuous evaluation of these vaccines ensures that they remain effective tools in safeguarding public health.
Vaccination has been a cornerstone in preventing infectious diseases, significantly reducing morbidity and mortality worldwide. Understanding the different types of vaccines is crucial for grasping how they work and their implications for public health. Two well-known types are live-attenuated vaccines and inactivated vaccines. This blog explores the differences between these two vaccine types, their mechanisms, applications, and considerations.
Live-Attenuated Vaccines
What Are Live-Attenuated Vaccines?
Live-attenuated vaccines contain versions of the living virus or bacteria that have been weakened under laboratory conditions. These pathogens are made less virulent, meaning they cannot cause the disease in healthy individuals but still provoke a strong immune response.
Mechanism of Action
When administered, live-attenuated vaccines mimic a natural infection, stimulating the immune system by producing a robust cellular and antibody-mediated response. Since they closely resemble the natural infection, the immune system gets a comprehensive picture of the pathogen, which leads to long-lasting immunity.
Benefits and Applications
Live-attenuated vaccines often provide lifelong immunity with just one or two doses. They have been used successfully for diseases such as measles, mumps, rubella (MMR), and chickenpox. The strong immune response they elicit is particularly beneficial in controlling outbreaks and providing community protection.
Considerations and Limitations
These vaccines are generally not suitable for individuals with weakened immune systems, such as those undergoing chemotherapy or living with HIV/AIDS. There is a small risk that the weakened virus could mutate back to a more virulent form, although this is extremely rare. Additionally, live-attenuated vaccines require careful storage and handling to maintain their efficacy.
Inactivated Vaccines
What Are Inactivated Vaccines?
Inactivated vaccines consist of viruses or bacteria that have been killed so that they cannot replicate or cause disease. These vaccines use various methods to inactivate the pathogen, such as heat, chemicals, or radiation.
Mechanism of Action
By introducing inactivated pathogens, the vaccine stimulates the immune system to recognize the pathogen and mount an immune response. However, since the pathogen is not alive, the immune response is generally less robust compared to live-attenuated vaccines, often necessitating booster shots.
Benefits and Applications
Inactivated vaccines are safe for individuals with compromised immune systems, as they cannot cause infection. They are used widely for diseases like influenza, hepatitis A, and rabies. These vaccines are stable and can be stored easily, which makes them accessible in various settings, including those with limited refrigeration facilities.
Considerations and Limitations
Inactivated vaccines typically require multiple doses and booster shots to maintain immunity. The immune response might not be as strong or long-lasting as that from live-attenuated vaccines, potentially requiring more frequent updates to vaccine formulations, particularly in the case of rapidly mutating viruses like influenza.
Comparative Analysis
Efficacy
Live-attenuated vaccines generally provoke stronger and longer-lasting immune responses, often with fewer doses required. In contrast, inactivated vaccines might need multiple doses and booster shots to sustain protection.
Safety
Inactivated vaccines are safer for immunocompromised individuals. Live-attenuated vaccines, while effective, are generally contraindicated in these populations due to the risk, however minimal, of causing illness.
Storage and Handling
Live-attenuated vaccines need stringent storage conditions to maintain their viability, typically requiring refrigeration. Inactivated vaccines, being more stable, are easier to store and handle.
Conclusion
Both live-attenuated and inactivated vaccines play crucial roles in preventing infectious diseases. Their differences highlight the importance of understanding vaccine types to make informed decisions about vaccination strategies. Each type has its unique advantages and considerations, shaping its use in various contexts and among different populations. As science progresses, continuous evaluation of these vaccines ensures that they remain effective tools in safeguarding public health.
Discover Eureka LS: AI Agents Built for Biopharma Efficiency
Stop wasting time on biopharma busywork. Meet Eureka LS - your AI agent squad for drug discovery.
▶ See how 50+ research teams saved 300+ hours/month
From reducing screening time to simplifying Markush drafting, our AI Agents are ready to deliver immediate value. Explore Eureka LS today and unlock powerful capabilities that help you innovate with confidence.
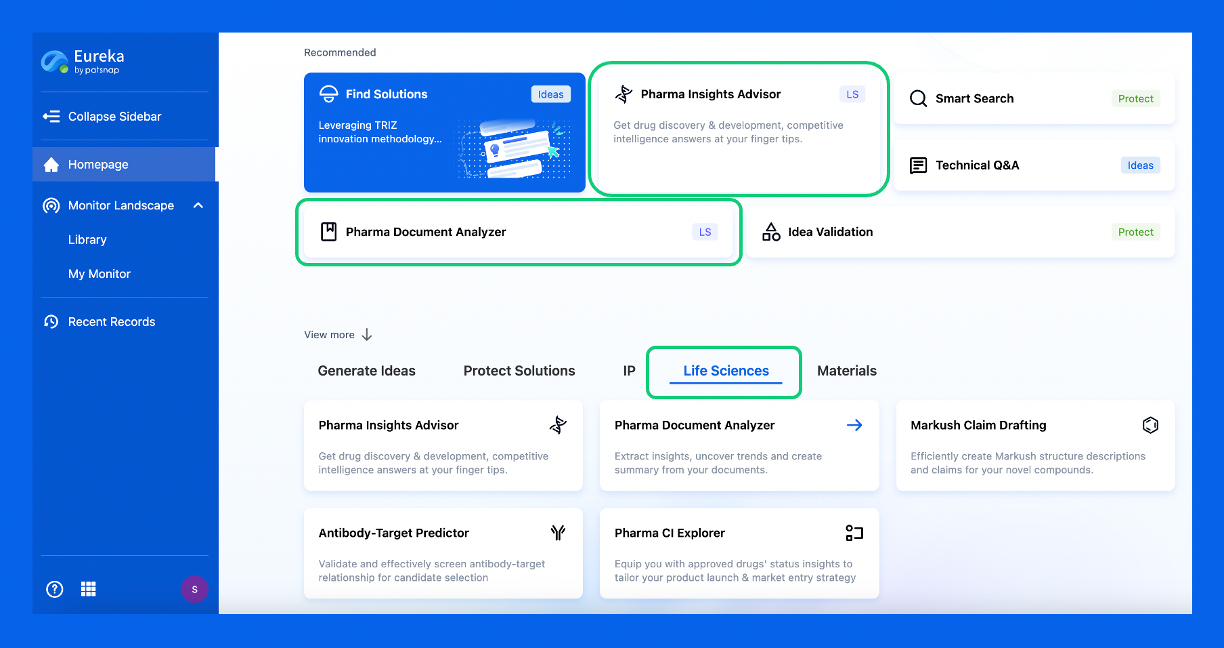
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.