Request Demo
Last update 08 May 2025
Euthyroid Sick Syndromes
Last update 08 May 2025
Basic Info
Synonyms EUTHYROID SICK SYNDROME <LOW T3/ LOW T4 SYNDROME>, EUTHYROID SICK SYNDROME LOW T3 LOW T4 SYNDROME, Euthyroid Sick Syndrome + [27] |
Introduction Conditions of abnormal THYROID HORMONES release in patients with apparently normal THYROID GLAND during severe systemic illness, physical TRAUMA, and psychiatric disturbances. It can be caused by the loss of endogenous hypothalamic input or by exogenous drug effects. The most common abnormality results in low T3 THYROID HORMONE with progressive decrease in THYROXINE; (T4) and TSH. Elevated T4 with normal T3 may be seen in diseases in which THYROXINE-BINDING GLOBULIN synthesis and release are increased. |
Analysis
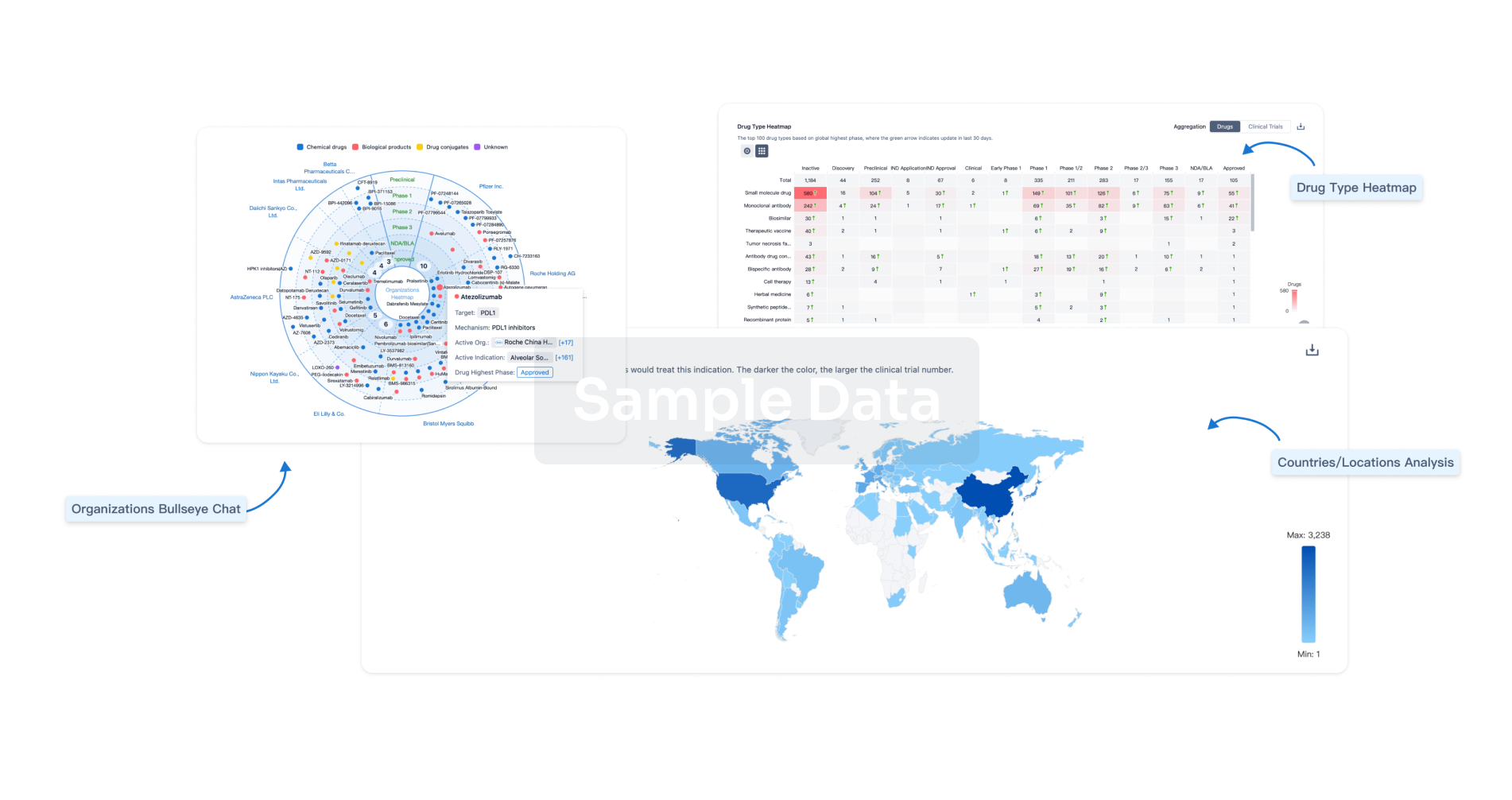
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free