Request Demo
Last update 08 May 2025
Angiosarcoma of the Breast
Last update 08 May 2025
Basic Info
Synonyms Angiosarcoma of Breast, Angiosarcoma of the Breast, Angiosarcoma of the breast + [13] |
Introduction A malignant vascular neoplasm arising from the breast. |
Related
2
Clinical Trials associated with Angiosarcoma of the BreastNCT03017573
Prospective Biobanking Study in Cancer Patients Aiming at Better Understand the Link Between the Molecular Alterations of the Tumor Itself, Its Microenvironment and Immune Response (SCANDARE)
SCANDARE is a prospective biobanking study on tumor (+/- nodes), plasma and blood samples at different time points in ovarian, triple negative breast, Head and Neck Cancer, advanced stage treatment-naïve cervical cancer and sarcoma (breast angiosarcoma and uterine sarcoma) cancers. This study will allowed to identify new molecular and/or immunological biomarkers associated with clinical and biological features of the tumors. All patients will receive standard treatment according to the stage of the diseases and usual procédures.
Start Date06 Jan 2017 |
Sponsor / Collaborator |
EUCTR2012-005846-39-DE
Phase II, multicenter, open-label, single-arm trial in advanced and relapsed Angiosarcomas, to evaluate the efficacy of pazopanib (Votrient) in combination with standard of care treatment paclitaxel ( Evaluation of Votrient in angiosarcoma - EVA) - EVA (Evaluation of Votrient in angiosarcoma)
Start Date22 Jul 2014 |
Sponsor / Collaborator- |
100 Clinical Results associated with Angiosarcoma of the Breast
Login to view more data
100 Translational Medicine associated with Angiosarcoma of the Breast
Login to view more data
0 Patents (Medical) associated with Angiosarcoma of the Breast
Login to view more data
377
Literatures (Medical) associated with Angiosarcoma of the Breast01 Mar 2025·Virchows Archiv
TRPS1 expression in breast angiosarcoma
Article
Author: Papp, Eszter ; Kulka, Janina ; Pancsa, Tamás ; Cserni, Gábor ; Schubert, Anna ; Kuthi, Levente ; Varga, Linda ; Kovács, Kristóf Attila ; Chien, Yi-Che Chang ; Kálmán, Endre ; Almási, Szintia ; Pósfai, Boglárka
25 Jan 2025·Cureus
Secondary Breast Angiosarcoma Five Years After Radiation Therapy for Ductal Carcinoma In Situ
Article
Author: Brown, Pierpont ; Wyer, Abigayle ; Grabill, Nathaniel ; Louis, Mena ; Strom, Priscilla
01 Dec 2024·European Journal of Surgical Oncology
Timeline of surgery in localized angiosarcoma of the breast: Improving outcome following multidisciplinary treatment optimization
Article
Author: Gronchi, Alessandro ; Folli, Secondo ; Cortinovis, Umberto ; Vingiani, Andrea ; Casali, Paolo G ; Stacchiotti, Silivia ; Collini, Paola ; Fiore, Marco ; Allajbej, Albina ; Listorti, Chiara ; Palassini, Elena ; Sangalli, Claudia ; Mariani, Luigi ; Casali, Paolo G. ; Gennaro, Massimiliano
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
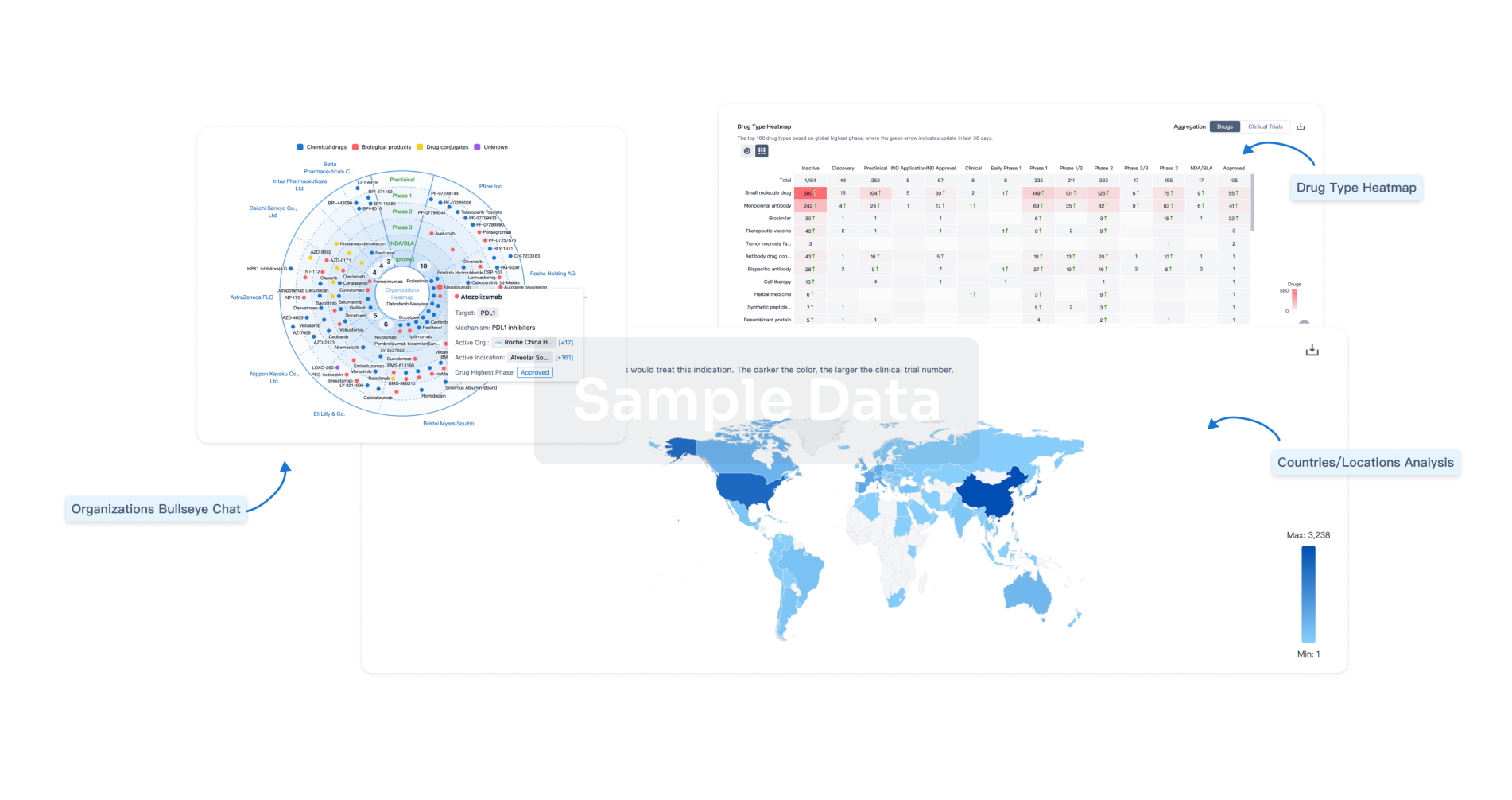
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
