Request Demo
Last update 08 May 2025
Progressive bulbar palsy
Last update 08 May 2025
Basic Info
Synonyms Bulbar Palsies, Progressive, Bulbar Palsy, Progressive, Bulbar palsy + [28] |
Introduction A motor neuron disease marked by progressive weakness of the muscles innervated by cranial nerves of the lower brain stem. Clinical manifestations include dysarthria, dysphagia, facial weakness, tongue weakness, and fasciculations of the tongue and facial muscles. The adult form of the disease is marked initially by bulbar weakness which progresses to involve motor neurons throughout the neuroaxis. Eventually this condition may become indistinguishable from AMYOTROPHIC LATERAL SCLEROSIS. Fazio-Londe syndrome is an inherited form of this illness which occurs in children and young adults. (Adams et al., Principles of Neurology, 6th ed, p1091; Brain 1992 Dec;115(Pt 6):1889-1900) |
Analysis
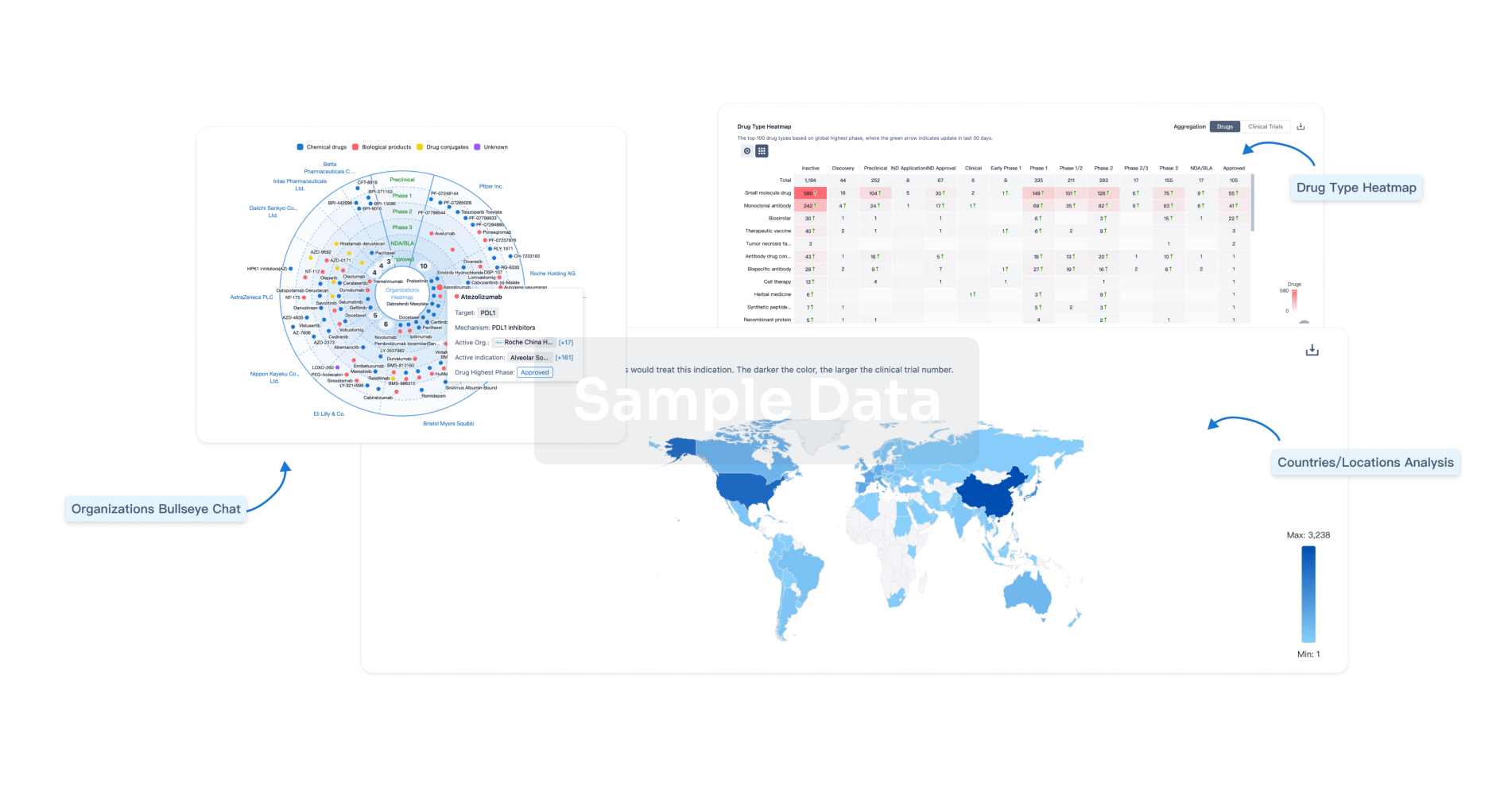
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free