Request Demo
Last update 08 May 2025
Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-Negative
Last update 08 May 2025
Basic Info
Synonyms JAK3 Deficiency, SCID, T CELL-NEGATIVE, B CELL-POSITIVE, NK CELL-NEGATIVE, SCID, T Cell-Negative, B Cell-Positive, NK Cell-Negative + [4] |
Introduction An autosomal recessive severe combined immunodeficiency caused by mutation(s) in the JAK3 gene, encoding tyrosine-protein kinase JAK3. It is characterized by decreased concentrations of T-cells and NK-cells and normal concentrations of B-cells. |
Related
1
Clinical Trials associated with Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-NegativeNCT04370795
Matched Related and Unrelated Donor Stem Cell Transplantation for Severe Combined Immune Deficiency (SCID): Busulfan-based Conditioning With h-ATG, Radiation, and Sirolimus
Background:
Severe combined immune deficiency (SCID) is a group of conditions where the immune system does not work properly. The only cure for most SCIDs is a stem cell transplant (getting cells from a donor). These transplants can have serious complications. Before the transplant, people often get high doses of drugs and radiation to prepare the body to accept the cells from the donor. Researchers want to see if low doses of drugs alone without radiation work just as well as low doses of drugs with radiation for SCID patients getting stem cell transplants.
Objective:
To test a set of drugs with or without radiation given before a stem cell transplant.
Eligibility:
People ages 3-40 who have SCID and who have a stem cell donor - either related or unrelated.
Design:
Participants will be admitted to the hospital 10 days before transplant. They will undergo:
medical history
medication review
physical exam
blood and urine tests (may include a 24-hour urine collection)
heart, lung, and breathing tests
imaging scans
bone marrow sample
nutrition assessment
dental exam
eye exam
meeting with a social worker.
Participants will get a plastic port called a central line. It is a hollow tube that is placed in the upper chest. It will be used to give medicines and take blood.
All participants will take chemotherapy drugs. Some will get radiation.
Participants will have a stem cell transplant. They will get the cells as an infusion through their central line. They will stay in the hospital for 30 days after transplant.
Participants must stay within 1 hour of NIH for 3 months after transplant. During this time, they will have follow-up visits at NIH at least once a week. Then they will have follow-up visits once or twice a year for 5-6 years.
Severe combined immune deficiency (SCID) is a group of conditions where the immune system does not work properly. The only cure for most SCIDs is a stem cell transplant (getting cells from a donor). These transplants can have serious complications. Before the transplant, people often get high doses of drugs and radiation to prepare the body to accept the cells from the donor. Researchers want to see if low doses of drugs alone without radiation work just as well as low doses of drugs with radiation for SCID patients getting stem cell transplants.
Objective:
To test a set of drugs with or without radiation given before a stem cell transplant.
Eligibility:
People ages 3-40 who have SCID and who have a stem cell donor - either related or unrelated.
Design:
Participants will be admitted to the hospital 10 days before transplant. They will undergo:
medical history
medication review
physical exam
blood and urine tests (may include a 24-hour urine collection)
heart, lung, and breathing tests
imaging scans
bone marrow sample
nutrition assessment
dental exam
eye exam
meeting with a social worker.
Participants will get a plastic port called a central line. It is a hollow tube that is placed in the upper chest. It will be used to give medicines and take blood.
All participants will take chemotherapy drugs. Some will get radiation.
Participants will have a stem cell transplant. They will get the cells as an infusion through their central line. They will stay in the hospital for 30 days after transplant.
Participants must stay within 1 hour of NIH for 3 months after transplant. During this time, they will have follow-up visits at NIH at least once a week. Then they will have follow-up visits once or twice a year for 5-6 years.
Start Date07 May 2025 |
Sponsor / Collaborator |
100 Clinical Results associated with Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-Negative
Login to view more data
100 Translational Medicine associated with Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-Negative
Login to view more data
0 Patents (Medical) associated with Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-Negative
Login to view more data
55
Literatures (Medical) associated with Severe Combined Immunodeficiency, Autosomal Recessive, T Cell-Negative, B Cell-Positive, NK Cell-Negative01 Apr 2025·Journal for ImmunoTherapy of Cancer
JAK3A573VandJAK3M511Imutations in peripheral T-cell lymphoma mediating resistance to anti-PD-1 therapy through the STAT3/PD-L1 pathway
Article
Author: Yang, Mengwei ; Tang, Le ; Zhang, Lei ; Han, Xiaohong ; Shi, Yuankai ; Lou, Ning ; Gao, Ruyun ; Yao, Jiarui ; Xie, Zucheng
13 Sep 2023·Human Mutation
Combination of Synonymous and Missense Mutations in JAK3 Gene Contributes to Severe Combined Immunodeficiency in One Child
Article
Author: Wang, Xingcui ; Zhang, Haozheng ; Zhang, Kaihui ; He, Qiuxia ; Tian, Rujin ; Lin, Guiyu ; Liu, Qinghua ; Gao, Min ; Bai, Lu ; Wang, Dong ; Abdalla, Mohnad ; Lv, Yuqiang ; Liu, Yi
01 Jun 2022·Leukemia
JAK3 mutations and mitochondrial apoptosis resistance in T-cell acute lymphoblastic leukemia
Article
Author: Devidas, Meenakshi ; Wood, Brent ; Stevenson, Kristen E ; Hunger, Stephen P ; Teachey, David T ; Meijerink, Jules P ; Letai, Anthony ; Yamagata, Natsuko ; Burns, Melissa ; Landrigan, Jack ; Barthe, Anais ; Gutierrez, Alejandro ; Silverman, Lewis B ; Chonghaile, Triona Ni ; Loh, Mignon L ; Bodaar, Kimberly
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
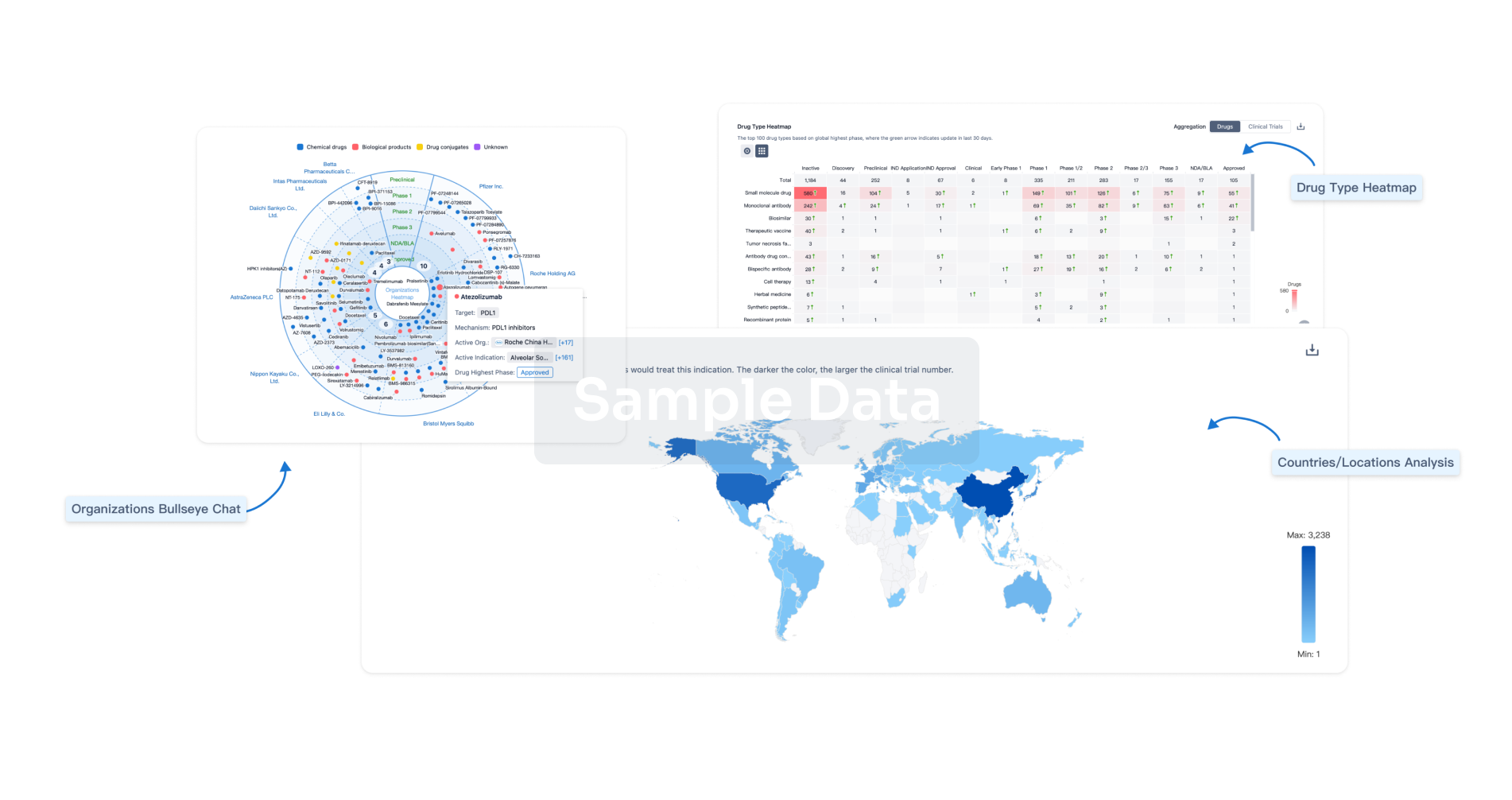
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free