Request Demo
Last update 08 May 2025
Mouth, Edentulous
Last update 08 May 2025
Basic Info
Synonyms Absence of teeth, Absence of teeth (finding), EDENTULOUS + [21] |
Introduction Total lack of teeth through disease or extraction. |
Related
1
Drugs associated with Mouth, EdentulousTarget- |
Mechanism Tissue replacements |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhaseWithdrawn |
First Approval Ctry. / Loc. United States |
First Approval Date09 Mar 2012 |
485
Clinical Trials associated with Mouth, EdentulousACTRN12622001255774
Efficacy of Poly Ether Ketone (PEK) framework to reinforce digital dental prostheses to prevent prostheses fracture for edentulous adult requiring dental rehabilitation
Start Date01 Jun 2025 |
Sponsor / Collaborator |
DRKS00035718
Effect of complete dentures on 3-dimensional labial soft tissue support in edentulous patients, evaluated with facial scans. - Face Scans
Start Date30 Apr 2025 |
Sponsor / Collaborator- |
NCT06870929
Effect of Different Intraoral Scanning Approaches on the Passive Fit of Mandibular All-on-Four Screw-Retained Frameworks
Although an intraoral scanner IOS can offer the clinician a completely digital workflow, achieving trustworthy digital scans in edentulous jaws is challenging because of the lack of fixed anatomical landmarks. From this perspective, several methods have been proposed to improve the accuracy of digital scanning, however, related results remain inconclusive, and previously proposed devices have had limitations, such as bulkiness, excessive manufacturing requirements, and poor commercial applicability.
Thus, this study aims to clinically compare the effect of conventional versus photogrammetry intraoral scanning methods on the passive fit of mandibular all-on four screw-retained frameworks.
Thus, this study aims to clinically compare the effect of conventional versus photogrammetry intraoral scanning methods on the passive fit of mandibular all-on four screw-retained frameworks.
Start Date03 Mar 2025 |
Sponsor / Collaborator |
100 Clinical Results associated with Mouth, Edentulous
Login to view more data
100 Translational Medicine associated with Mouth, Edentulous
Login to view more data
0 Patents (Medical) associated with Mouth, Edentulous
Login to view more data
48
Literatures (Medical) associated with Mouth, Edentulous01 Dec 2024·Journal of Oral and Maxillofacial Surgery
Effect of Statins on Patients With Osteoradionecrosis of the Jaw
Article
Author: Kusumoto, Junya ; Sakakibara, Akiko ; Furudoi, Shungo ; Akashi, Masaya ; Muraki, Yumi
01 Jan 2024·International Journal of Dentistry
A Cross‐Sectional Study
Article
Author: Lidani, Rangel ; Gebler Philippi, Analucia ; Meiriely de Almeida Lopes, Naiany ; Floriani, Franciele ; Pauletto, Patrícia ; Luchi Klöppel, Naiara ; De Luca Canto, Graziela ; André Mezzomo, Luis
01 Mar 2023·Journal of dentistry (Shiraz, Iran)
Impact of Complete Denture and Mandibular Advancement Device in the Management of Completely Edentulous Obstructive Sleep Apneic Individuals: A Systematic Review with Meta-Analysis.
Article
Author: Kumar, V Anand ; Krishnamurthy, Preetha ; Banu, Fathima
Analysis
Perform a panoramic analysis of this field.
login
or
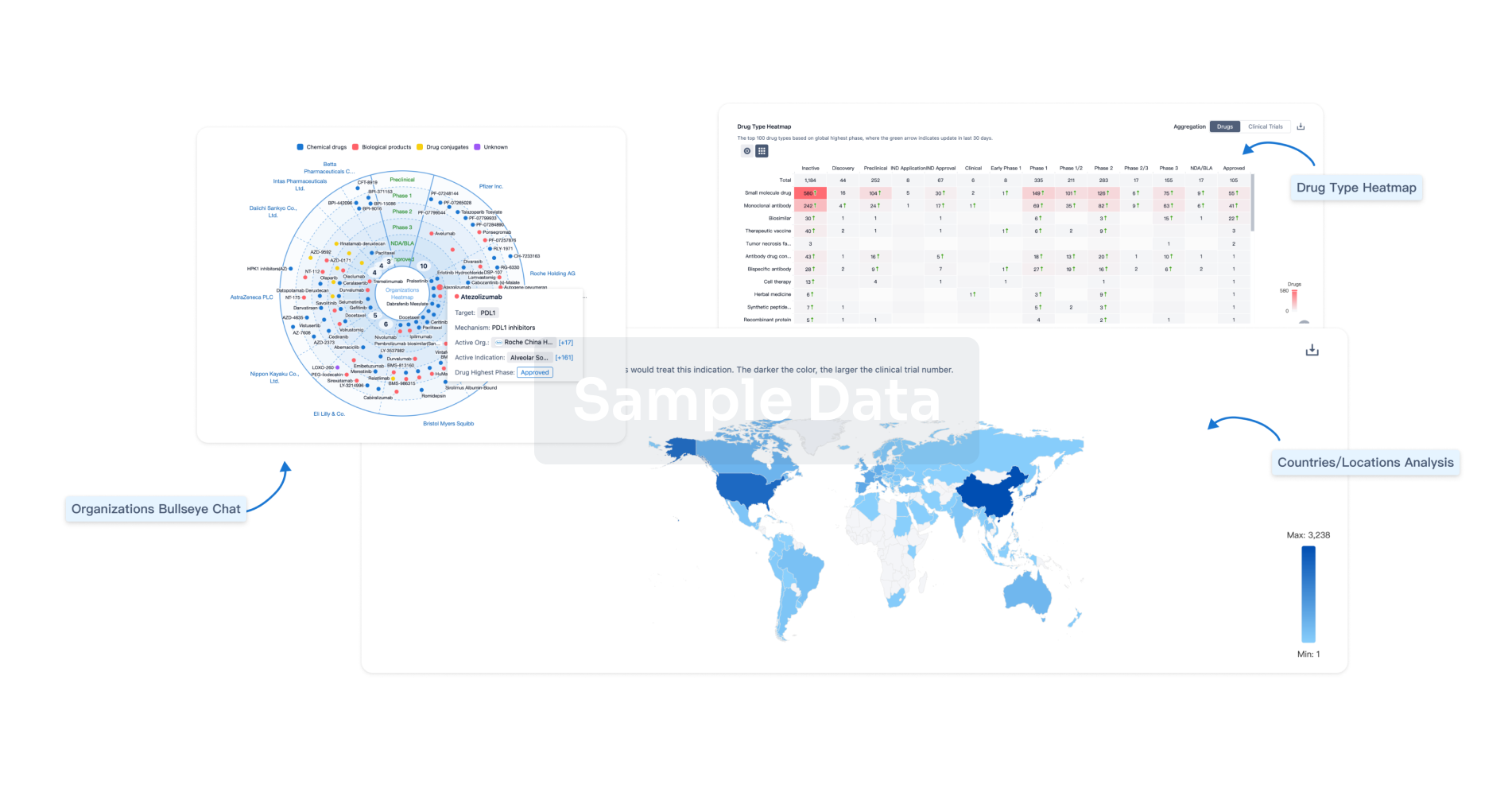
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


