Request Demo
Last update 17 Dec 2025
Monoclonal antibody(Normunity)
Last update 17 Dec 2025
Overview
Basic Info
Originator Organization |
Active Organization |
Inactive Organization- |
License Organization- |
Drug Highest PhasePreclinical |
First Approval Date- |
Regulation- |
Related
100 Clinical Results associated with Monoclonal antibody(Normunity)
Login to view more data
100 Translational Medicine associated with Monoclonal antibody(Normunity)
Login to view more data
100 Patents (Medical) associated with Monoclonal antibody(Normunity)
Login to view more data
9
Literatures (Medical) associated with Monoclonal antibody(Normunity)01 Sep 2025·Therapeutic Advances in Medical Oncology
Efficacy and safety of vascular-targeting agents in advanced soft tissue sarcoma: a systematic review and network meta-analysis
Article
Author: Cheng, Hong ; Xu, Hangcheng ; Wang, Jiayu ; Xu, Binghe ; Sa, Qiang ; Gao, Renchi ; Wang, Yan ; Zhou, Yiran
Background::
Soft tissue sarcomas (STS) are rare, heterogeneous tumors with poor prognosis, often characterized by high recurrence rates and limited response to conventional chemotherapy in advanced stages. Vascular-targeting agents (VTA) have shown promising efficacy for STS in numerous clinical trials; however, the optimal agent and combination strategies remain undetermined.
Objectives::
This work aims to compare the clinical efficacy and adverse events of different VTA-containing regimens for patients with STS.
Design::
This study is a systematic review and network meta-analysis.
Data sources and methods::
We searched PubMed, Embase, and the Cochrane Library for eligible randomized clinical trials. All trials with VTA as monotherapy or VTA-included regimens in the experimental or control groups were selected, except for some specific histological subtypes. Pooled hazard ratios (HRs) for survival data and odds ratios for objective response rate (ORR), disease control rate (DCR), and treatment-related adverse events with credible intervals were generated using R software. A Bayesian random-effects model was applied to rank different treatments based on the surface under the cumulative ranking curve (SUCRA) values.
Results::
Seventeen articles covering 15 studies were included. Pairwise comparisons demonstrated prolonged progression-free survival (PFS) for tyrosine kinase inhibitor (TKI) versus placebo (HR 0.50, 95% confidence interval (CI) 0.32–0.83) and prolonged overall survival (OS) for monoclonal antibody plus chemotherapy versus placebo (HR 0.42, 95% CI 0.19–0.89). Vascular-disrupting agents (VDA) plus chemotherapy were ranked highest for OS (87.05%) and ORR (89.66%). TKI plus chemotherapy and TKI plus immunotherapy had higher SUCRA values for PFS (68.21%) and DCR (82.29%). TKI-based regimens were associated with higher incidences of hypertension, diarrhea, and elevated transaminase levels, whereas chemotherapy-based strategies resulted in higher incidences of hematological toxicity and constipation.
Conclusion::
VTA-containing regimens showed promising activity and tolerability in patients with advanced STS. Combination regimens with TKI showed better efficacy for PFS and DCR. Novel VDA combined with chemotherapy showed potential to prolong OS and improve ORR.
Trial registration::
PROSPERO website (registration number: CRD42024588134).
01 Feb 2025·JTO clinical and research reports
Afatinib and Necitumumab in EGFR-Mutant NSCLC with Acquired Resistance to Tyrosine Kinase Inhibitors
Article
Author: Horn, Leora ; Wakelee, Heather A ; Iams, Wade T ; Myall, Nathaniel J ; Reckamp, Karen L ; Shyr, Yu ; Neal, Joel W ; Berry, Lynne D ; Padda, Sukhmani K ; Whisenant, Jennifer G ; York, Sally
Introduction:
Although tyrosine kinase inhibitors (TKIs) are effective against NSCLC harboring sensitizing EGFR gene mutations, acquired resistance is inevitable. Preclinical studies suggest that combining EGFR TKI and monoclonal antibody therapies may have activity in EGFR-mutated NSCLC that has progressed on TKI therapy alone. Therefore, we prospectively evaluated afatinib plus necitumumab in patients with EGFR-mutated NSCLC.
Methods:
This was a phase 1, dose-escalation, dose-expansion trial assessing the safety and efficacy of afatinib plus necitumumab. Patients had advanced or metastatic EGFR-mutated NSCLC with progression after (1) first-generation TKI if T790M negative, (2) subsequent line third-generation TKI if T790M positive, or (3) third-generation TKI in the first-line setting. Dose-escalation followed a 3+3 design. The primary end point of dose-expansion was objective response rate.
Results:
A total of 22 patients with EGFR-mutated NSCLC were enrolled. The maximum tolerated dose was afatinib 40 mg oral daily plus necitumumab 600 mg intravenous on days 1 and 15 every 28 days. There were no grade 4 to 5 adverse events observed, and seven patients (32%) experienced grade 3 treatment-related adverse events (three rash; one each oral mucositis, diarrhea, headache, ventricular arrhythmia, and tachycardia). In the entire cohort, there were no responses observed, the median progression-free survival was 1.8 months, and the disease control rate was 36% but varied between the subgroups.
Conclusions:
Afatinib plus necitumumab was safe but had limited activity in patients with EGFR-mutated NSCLC. Biomarker studies may identify patient subgroups that are more likely to benefit.
01 Apr 2024·Multiple Sclerosis Journal-Experimental Translational and Clinical
The patient-reported wearing-off phenomenon with monoclonal antibody treatments for multiple sclerosis
Article
Author: Marian, Lindsey M ; Conway, Devon S ; Harris, Kathleen A
Background:
Many patients report a wearing-off phenomenon with monoclonal antibody treatment for multiple sclerosis in which perceived benefits wear off before the next dose is due.
Objectives:
To determine prevalence of the wearing-off effect, symptoms experienced, impact on treatment satisfaction, and associated patient characteristics.
Methods:
Patients receiving natalizumab, ocrelizumab, ofatumumab, or rituximab at a tertiary multiple sclerosis center were invited to take an online survey interrogating their monoclonal antibody experience. Additional history and patient characteristic data were collected. Logistic regression was used to determine if patient characteristics predicted the wearing-off effect and linear regression to evaluate the impact of the wearing-off effect on treatment satisfaction. The models were adjusted for age, disease duration, race, sex, body mass index, education, and depression as measured by the Patient Health Questionnaire-9.
Results:
We received 258 qualifying responses and 141 (54.7%) patients reported the wearing-off phenomenon. The most common symptom was fatigue (47.7%). Higher Patient Health Questionnaire-9 scores were significantly associated with the wearing-off phenomenon (OR = 1.02, p = 0.005). The wearing-off effect (β = −0.52, p = 0.04) and higher Patient Health Questionnaire-9 (β = −0.09, p < 0.01) scores were associated with significantly reduced treatment satisfaction.
Conclusion:
The wearing-off phenomenon is common, associated with depression, and reduces treatment satisfaction. Research addressing mitigation strategies is needed.
1
News (Medical) associated with Monoclonal antibody(Normunity)23 Sep 2025
CHENGDU, China, Sept. 23, 2025 /PRNewswire/ -- The 2025 European Society for Medical Oncology (ESMO) Congress will take place in Berlin, Germany, from October 17 to 21. Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd. ("Kelun-Biotech", HKEX: 6990) will present results from multiple clinical studies at the congress, including data from its TROP2 ADC sacituzumab tirumotecan (sac-TMT), HER2 ADC A166 (trastuzumab botidotin), and CLDN18.2 ADC SKB315. Among these,
two Phase III clinical studies of sac-TMT were selected for the Latest Breakthrough Abstracts (LBA) and presented as oral reports, including one featured in the Presidential Symposium; one Phase III clinical study of A166 was selected for LBA and presented as oral report.
Abstract titles of these studies have been published on the official website of ESMO. The study results to be presented include:
Title: Sacituzumab tirumotecan (sac-TMT) vs platinum-based chemotherapy in EGFR-mutated (EGFRm) non-small cell lung cancer (NSCLC) following progression on EGFR-TKIs: results from the randomized, multi-center phase 3 OptiTROP-Lung04 study
Presentation Type: Presidential Symposium
Presentation #: LBA5
Date and Lecture Time: October 19, 4:52 PM to 5:04 PM local time
Title: Sacituzumab tirumotecan (sac-TMT) vs investigator's choice of chemotherapy (ICC) in previously treated locally advanced or metastatic hormone receptor-positive, HER2-negative (HR+/HER2-) breast cancer (BC): results from the randomized, multi-center phase 3 OptiTROP-Breast02 study
Presentation Type: Proffered Paper
presentation #: LBA23
Date and Lecture Time: October 18, 10:45 AM to 10:55 AM local time
Title: Trastuzumab botidotin vs trastuzumab emtansine (T-DM1) in HER2-positive unresectable or metastatic breast cancer: results from a randomized phase 3 study
Presentation Type: Proffered Paper
presentation #: LBA24
Date and Lecture Time: October 18, 10:55 AM to 11:05AM local time
Title: SKB315, a novel Claudin 18.2 (CLDN18.2) antibody-drug conjugate (ADC), in patients (pts) with advanced solid tumors including gastric/ gastroesophageal junction cancer (GC/GEJC): a phase 1 study
Presentation Type: Poster
Presentation #: 2139P
Date and Session Time: October 19, 9:00 AM to 5:00 PM local time
Title: Sacituzumab tirumotecan (sac-TMT) in Participants (pts) with Previously Treated, Advanced KRAS-Mutant NSCLC: Results from Cohort 5d of the SKB264-II-08 Study
Presentation Type: Poster
Presentation #: 1945P
Date and Session Time: October 18, 9:00 AM to 5:00 PM local time
Title: Sacituzumab tirumotecan (sac-TMT) + pembrolizumab[1] (pembro) for treatment-naïve advanced PD-L1 positive NSCLC: results from the Phase 2 MK-2870-003/SKB264-II-04 study
Presentation Type: Poster
Presentation #: 1949P
Date and Session Time: October 18, 9:00 AM to 5:00 PM local time
Title: Sacituzumab tirumotecan (sac-TMT) + Pembrolizumab in Metastatic Castration-Resistant Prostate Cancer (mCRPC): Results from Phase 2 MK-2870-002/SKB264-II-06 Study
Presentation Type: Poster
Presentation #: 2421P
Date and Session Time: October 18, 9:00 AM to 5:00 PM local time
Title: Sacituzumab tirumotecan (Sac-TMT) Monotherapy in Advanced/Metastatic Endometrial Carcinoma (EC): Results from a Phase 1/2 Study (MK-2870-001/KL264-01)
Presentation Type: Poster
Presentation #: 1111P
Date and Session Time: October 18, 9:00 AM to 5:00 PM local time
Title: Efficacy and Safety of sacituzumab tirumotecan (Sac-TMT) Monotherapy in Advanced/Metastatic Cervical Cancer: Results from a Phase 1/2 Study (MK-2870-001/KL264-01)
Presentation Type: Poster
Presentation #: 1168P
Date and Session Time: October 18, 9:00 AM to 5:00 PM local time
About sac-TMT
Sac-TMT, a core product of the Company, is a novel human TROP2 ADC in which the Company has proprietary intellectual property rights, targeting advanced solid tumors such as NSCLC, BC, gastric cancer (GC), gynecological tumors, among others. Sac-TMT is developed with a novel linker to conjugate the payload, a belotecan-derivative topoisomerase I inhibitor with a drug-to-antibody-ratio (DAR) of 7.4. Sac-TMT specifically recognizes TROP2 on the surface of tumor cells by recombinant anti-TROP2 humanized monoclonal antibodies, which is then endocytosed by tumor cells and releases the payload KL610023 intracellularly. KL610023, as a topoisomerase I inhibitor, induces DNA damage to tumor cells, which in turn leads to cell-cycle arrest and apoptosis. In addition, it also releases KL610023 in the tumor microenvironment. Given that KL610023 is membrane permeable, it can enable a bystander effect, or in other words kill adjacent tumor cells.
In May 2022, the Company licensed the exclusive rights to MSD (the tradename of Merck & Co., Inc., Rahway, NJ, USA) to develop, use, manufacture and commercialize sac-TMT in all territories outside of Greater China (includes Mainland China, Hong Kong, Macau, and Taiwan).
To date, 2 indications for sac-TMT have been approved and marketed in China for the treatment of adult patients with unresectable locally advanced or metastatic triple negative breast cancer (TNBC) who have received at least two prior systemic therapies (at least one of them for advanced or metastatic setting), EGFR mutation-positive locally advanced or metastatic non-squamous NSCLC following progression on EGFR-TKI therapy and platinum-based chemotherapy. In addition, two new indication applications for sac-TMT for the treatment of adult patients with EGFR-mutant locally advanced or metastatic NSCLC who progressed after treatment with EGFR-TKI therapy and with unresectable locally advanced, metastatic hormone receptor positive (HR+) and human epidermal growth factor receptor 2-negative (HER2-) BC who have received prior endocrine therapy and other systemic treatments in the advanced or metastatic setting were accepted by the Center for Drug Evaluation of NMPA, and were included in the priority review and approval process. As of today, the Company has initiated 9 registrational clinical studies in China. MSD has initiated 14 ongoing Phase 3 global clinical studies of sac-TMT as a monotherapy or with pembrolizumab or other anti-cancer agents for several types of cancer. These studies are sponsored and led by MSD.
About Trastuzumab Botidotin (A166)
Trastuzumab botidotin is a differentiated HER2 ADC in new drug application (NDA) registration stage to treat advanced HER2+ solid tumors. As an innovative HER2 ADC developed by the Company, it conjugates a novel, MMAF derivative (a highly cytotoxic tubulin inhibitor, Duo-5) via a stable, enzyme-cleavable linker to a HER2 monoclonal antibody with a DAR of 2. Trastuzumab botidotin specifically binds to HER2 on the surface of tumor cells and is internalized by tumor cells, releasing the toxin molecule Duo-5 inside the cell. Duo-5 induces tumor cell cycle arrest in the G2/M phase, leading to tumor cell apoptosis. After targeting HER2, trastuzumab botidotin can also inhibit the HER2 signaling pathway; it has antibody-dependent cell-mediated cytotoxicity (ADCC) activity.
Based on the results of a randomized, controlled, open-label Phase III study, the New Drug Application (NDA) for trastuzumab botidotin was accepted by the Center for Drug Evaluation (CDE) of the National Medical Products Administration (NMPA) in January 2025 for the treatment of adult patients with HER2+ unresectable or metastatic BC who have received at least one prior anti-HER2 therapy was accepted by the CDE of the NMPA. At a pre-specified interim analysis, trastuzumab botidotin monotherapy demonstrated a statistically significant and clinically meaningful improvement in the primary endpoint of progression-free survival (PFS) as assessed by the Blinded Independent Central Review (BICR) compared with T-DM1.
Currently, Kelun-Biotech has initiated an open, multi-center Phase II clinical study of trastuzumab botidotin in the treatment of HER2+ unresectable or metastatic BC that previously received a topoisomerase inhibitor ADC.
About SKB315
SKB315 is a novel CLDN18.2 ADC targeting advanced solid tumors configured with a proprietary, in-house developed humanized CLDN18.2 mAb and a differentiated payload-linker design. Currently, Kelun-Biotech has initiated the exploration in combination with immunotherapy for gastric/gastroesophageal junction cancer (GC/GEJC) while advancing monotherapy studies for tumors expressing CLDN18.2, such as GC/GEJC and pancreatic cancer.
About Kelun-Biotech
Kelun-Biotech (6990.HK) is a holding subsidiary of Kelun Pharmaceutical (002422.SZ), which focuses on the R&D, manufacturing, commercialization and global collaboration of innovative biological drugs and small molecule drugs. The company focuses on major disease areas such as solid tumors, autoimmune, inflammatory, and metabolic diseases, and in establishing a globalized drug development and industrialization platform to address the unmet medical needs in China and the rest of world. The Company is committed to becoming a leading global enterprise in the field of innovative drugs. At present, the Company has more than 30 ongoing key innovative drug projects, of which 3 projects have been approved for marketing, 2 projects are in the NDA stage and more than 10 projects are in the clinical stage. The company has established one of the world's leading proprietary ADC and novel DC platforms, OptiDC™, and has 1 ADC project approved for marketing,1 ADC project in NDA stage and multiple ADC and novel DC assets in clinical or preclinical research stage. For more information, please visit .
SOURCE Sichuan Kelun-Biotech Biopharmaceutical Co., Ltd.
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
Phase 3Phase 2Clinical ResultPhase 1Immunotherapy
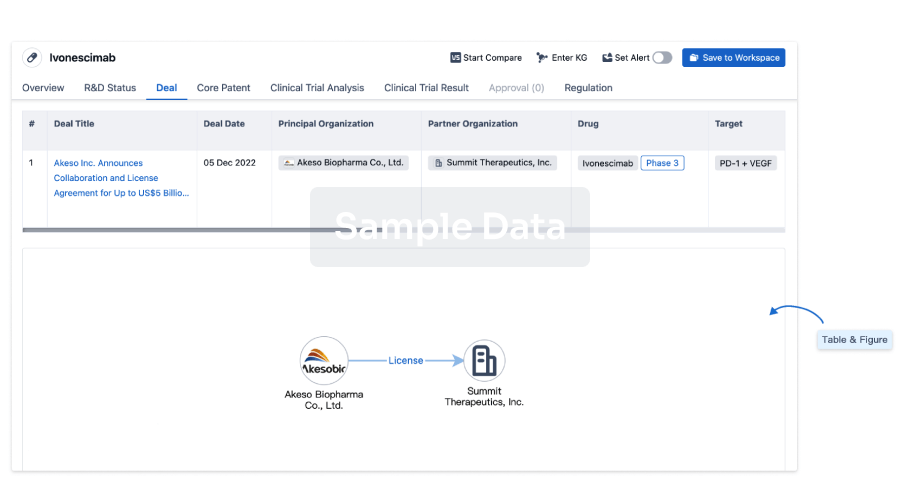
100 Deals associated with Monoclonal antibody(Normunity)
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Neoplasms | Preclinical | United States | 29 Oct 2022 |
Login to view more data
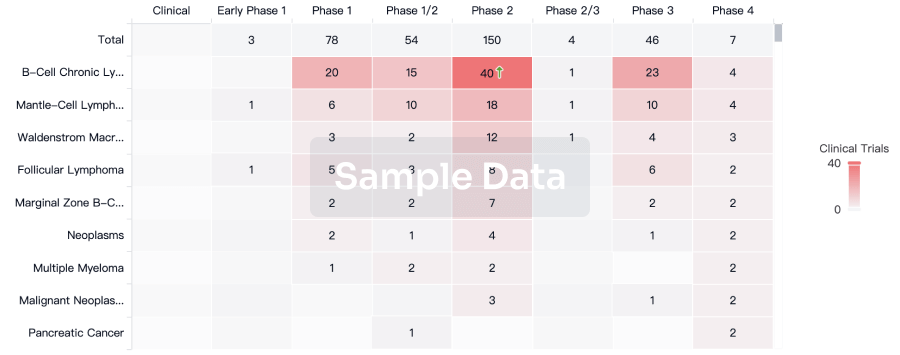
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
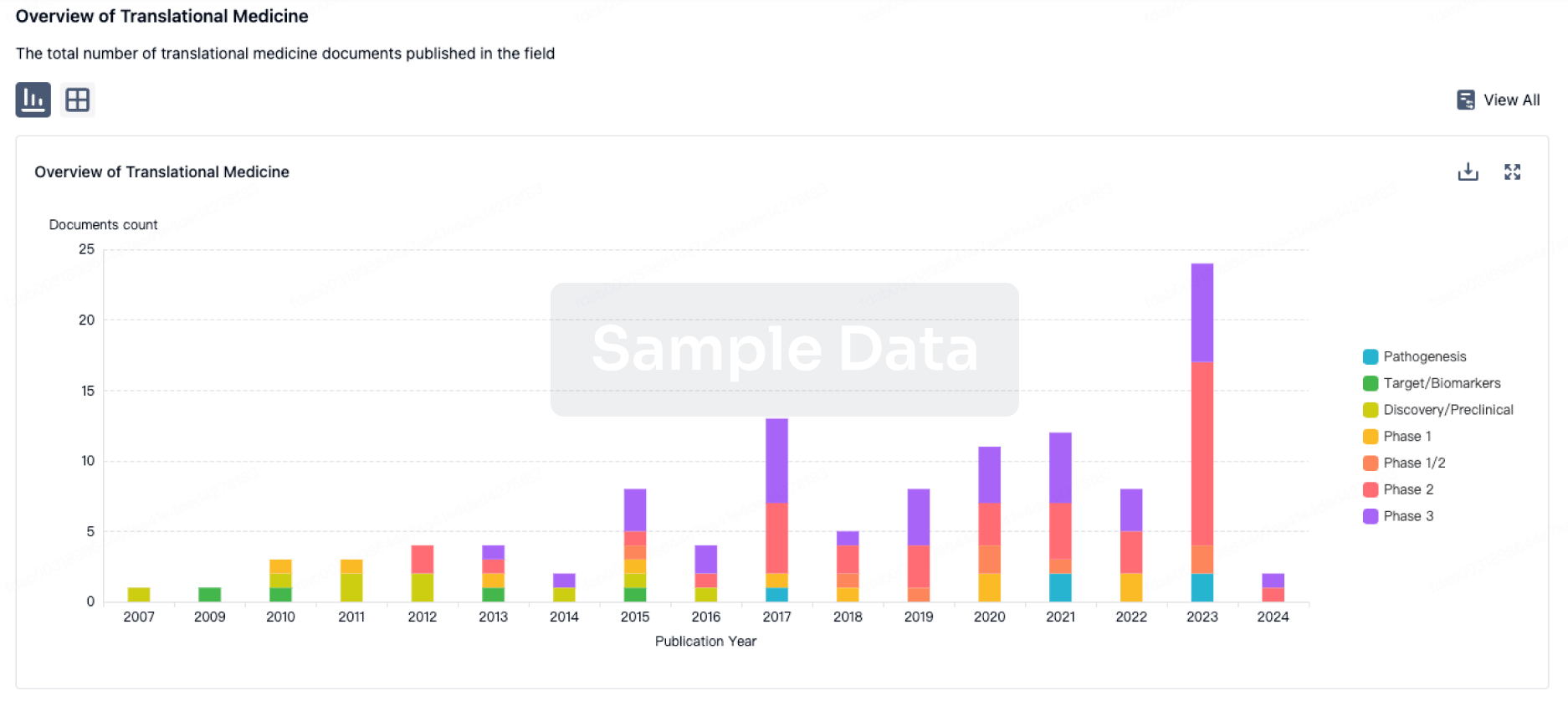
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
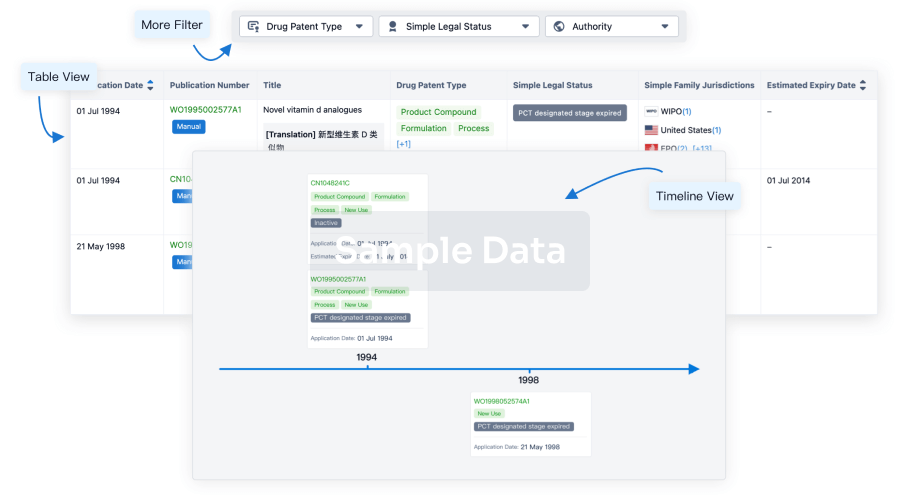
Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
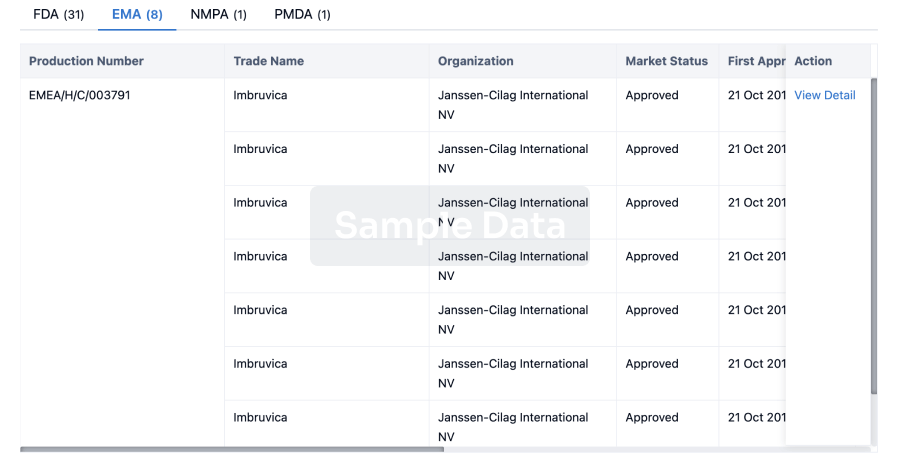
Approval
Accelerate your research with the latest regulatory approval information.
login
or
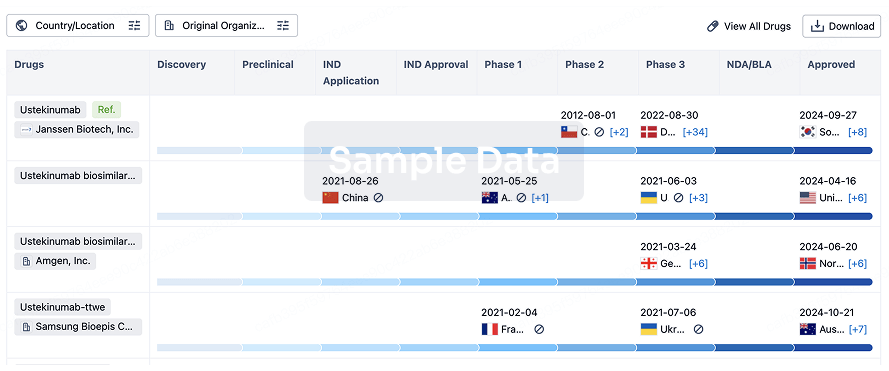
Biosimilar
Competitive landscape of biosimilars in different countries/locations. Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3.
login
or
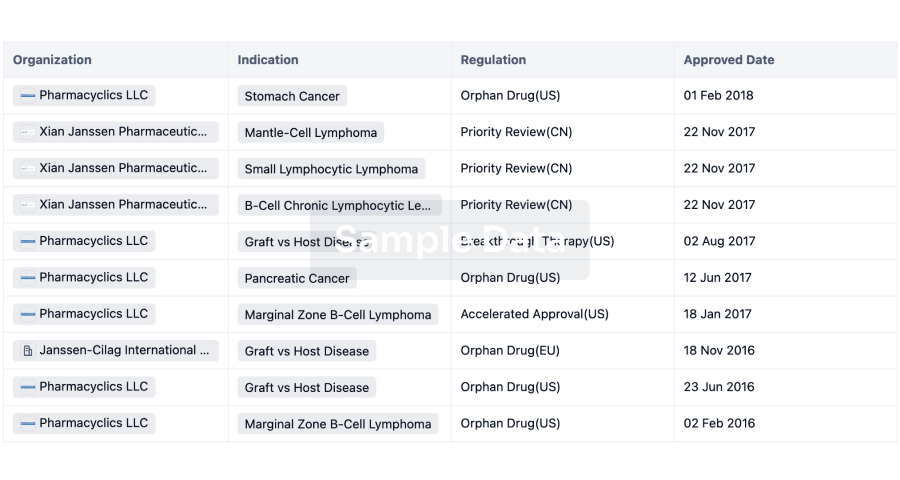
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
