Request Demo
Last update 30 Sep 2025
Valziflocept
Last update 30 Sep 2025
Overview
Basic Info
Drug Type Recombinant protein |
Synonyms FcγRIIb, Human soluble Fc-gamma receptor IIb, Valziflocept (USAN) + [5] |
Target |
Action antagonists |
Mechanism CD32B antagonists(Low affinity immunoglobulin gamma Fc region receptor II-b antagonists) |
Active Indication- |
Inactive Indication |
Originator Organization |
Active Organization- |
Inactive Organization |
License Organization- |
Drug Highest PhaseDiscontinuedPhase 2 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Sequence Code 9555778
Source: *****
Related
5
Clinical Trials associated with ValzifloceptPER-050-16
A Phase 2b, Multidose, Multicenter, Double-blind, Placebocontrolled, 24 Week Study to Evaluate the Efficacy and Safety of Intravenous Infusion with Recombinant Human Soluble Fc-gamma IIB Receptor SM101 in Subjects with Systemic Lupus Erythematosus (SLE)
Start Date01 Jul 2017 |
Sponsor / Collaborator |
NCT02605525
A Phase 2 Study to Assess the Efficacy and Safety of Intravenous Infusion With Human Soluble Recombinant Fc-gamma Receptor IIB (SM101/BAX 1810) in Subjects With Immunoglobulin A Nephropathy (IgAN)
The purpose of this study is to assess the efficacy and safety of SM101 in the treatment of Immunoglobulin A nephropathy (IgAN)
Start Date31 Dec 2015 |
Sponsor / Collaborator |
EUCTR2010-023396-25-BE
Phase IIa, 2:2:1 randomised, double-blind, placebo-controlled,parallel group, multi-centre clinical trial toinvestigate the safety, efficacy and pharmacokinetics ofrecombinant human soluble Fc-gamma receptor IIb(SM101) for intravenous application in the treatment ofsystemic lupus erythematosus (SLE) patients with orwithout a history of lupus nephritis - SMILE
Start Date13 Jul 2011 |
Sponsor / Collaborator |
100 Clinical Results associated with Valziflocept
Login to view more data
100 Translational Medicine associated with Valziflocept
Login to view more data
100 Patents (Medical) associated with Valziflocept
Login to view more data
8
Literatures (Medical) associated with Valziflocept15 Apr 2020·Avian diseasesQ4 · AGRICULTURAL & FORESTRY SCIENCE
Comparison of the Pathogenicity of Five Clostridium perfringens Isolates Using an Eimeria maxima Coinfection Necrotic Enteritis Disease Model in Commercial Broiler Chickens
Q4 · AGRICULTURAL & FORESTRY SCIENCE
Article
Author: Wang, Yunfei ; Liu, Liheng ; Lillehoj, Hyun ; Zhao, Hongyan ; Lu, Mingmin ; Lee, Youngsub ; Melville, Stephen ; Sun, Zhifeng ; Xianyu, Zhezi ; Li, Charles ; Gu, Changqin ; Yan, Xianghe
Clostridium perfringens (CP) is the etiologic agent of necrotic enteritis (NE) in broiler chickens that is responsible for massive economic losses in the poultry industry in response to voluntary reduction and withdrawal of antibiotic growth promoters. Large variations exist in the CP isolates in inducing intestinal NE lesions. However, limited information is available on CP isolate genetics in inducing NE with other predisposing factors. This study investigated the ability of five CP isolates from different sources to influence NE pathogenesis by using an Eimeria maxima (EM) coinfection NE model: Str.13 (from soil), LLY_N11 (healthy chicken intestine), SM101 (food poisoning), Del1 (netB+tpeL-) and LLY_Tpel17 (netB+tpeL+) for NE-afflicted chickens. The 2-wk-old broiler chickens were preinfected with EM (5 × 103 oocysts) followed by CP infection (around 1 × 109 colony-forming units per chicken). The group of the LLY_Tpel17 isolate with EM coinfection had 25% mortality. No mortality was observed in the groups infected with EM alone, all CP alone, or dual infections of EM/other CP isolates. In this model of EM/CP coinfections, the relative percentages of body weight gain showed statistically significant decreases in all EM/CP groups except the EM/SM101 group when compared with the sham control group. Evident gut lesions were only observed in the three groups of EM/LLY_N11, EM/Del1, and EM/LLY_Tpel17, all of which possessed an essential NE pathogenesis locus in their genomes. Our studies indicate that LLY_Tpel17 is highly pathogenic to induce severe gut lesions and would be a good CP challenge strain for studies investigating pathogenesis and evaluating the protection efficacy for antibiotic alternative approaches.
01 May 2016·Journal of clinical immunologyQ2 · MEDICINE
The FcγR/IgG Interaction as Target for the Treatment of Autoimmune Diseases
Q2 · MEDICINE
Review
Author: Sondermann, Peter
FcγRs are a crucial component of the antibody response as they mediate the cellular effector functions in response to IgG-containing immune complexes (ICs). Therefore, they also play a central role in the pathogenesis of autoimmune diseases which offers an attractive option to specifically target this class of molecules and their interaction with IgG for treatment of immune disorders. In detail, two strategies are discussed in this article. SM101, a soluble FcγR that is already in clinical development competes with the interaction of IgG with membrane FcγRs. Oppositely, SM201 recruits the inhibitory FcγRIIB for a broad down-modulation of the immune system. The presented approaches for the treatment of autoimmune diseases have the potential be more efficacious with fewer side effects than the currently used therapeutic options.
01 Mar 2015·The Journal of investigative dermatologyQ1 · MEDICINE
Recombinant Soluble CD32 Suppresses Disease Progression in Experimental Epidermolysis Bullosa Acquisita
Q1 · MEDICINE
Letter
Author: Zillikens, Detlef ; Möckel, Nicole ; Vorobyev, Artem ; Pipi, Elena ; Sondermann, Peter ; van Beek, Nina ; Ludwig, Ralf J ; Iwata, Hiroaki
TO THE EDITOR: Epidermolysis bullosa acquisita (EBA) is a prototypic organ-specific autoimmune disease, which is characterized by chronic mucocutaneous subepidermal blistering (Gupta et al., 2012; Schmidt and Zillikens, 2013).The autoimmune response is directed against a 290-kDa protein located at the dermal-epidermal junction (DEJ), which has been identified as the type VII collagen (Woodley et al., 1988).Despite major achievements in the understanding of EBA pathogenesis (Gupta et al., 2012), therapy of EBA patients remains difficult, and, because of the low incidence of the disease, data from clin. trials are still missing.Most commonly corticosteroids in combination with other (immunosuppressive) drugs are used (Engineer and Ahmed, 2001), which is associated with severe and potentially life-threatening adverse reactions.Therefore, there is a great and so far unmet medical need for effective and safe treatment options in EBA.We have recently established a mouse model of EBA induced by immunization with an immunodominant domain located within the non-collagenous 1 domain of murine type VII collagen (Iwata et al., 2013).Induction of skin blistering in exptl. EBA depends on the expression of activating Fc gamma receptor (FcγR; Kasperkiewicz et al., 2012).The detrimental contribution of FcγR binding to tissue-deposited immune complexes (ICs) has been well documented in models of autoantibody-mediated diseases, such as rheumatoid arthritis (Kleinau et al., 2000), immune-mediated thrombocytopenia (McKenzie et al., 1999), and autoimmune bullous dermatoses (Ludwig et al., 2013).On the basis of these findings, FcγR seems to be a promising therapeutic target for the treatment of autoantibody-mediated inflammatory diseases.Currently, several novel compounds targeting the interaction of ICs with FcγR are pursued either in preclin. model systems or in clin. trials.Notably, pharmacol. modifications of IgG glycosylation at the Fc fragment, which alters IgG's affinity to FcγR, have prophylactic and therapeutic effects in several models of autoimmunity (Collin and Ehlers, 2013).Other potentially promising FcγR targeting strategies, such as competitive binding of ICs by recombinant soluble FcγR2B (soluble CD32, sCD32, and SM101) in idiopathic thrombocytopenia or systemic lupus erythematosus, are already evaluated in phase I/II clin. trials (http://www.controlled-trials.com/isrctn/search.htmlsrch=SM101).Here, we evaluated whether treatment with sCD32 has therapeutic effects in exptl. EBA. sCD32 binds to IC and thereby blocks the binding of FcγR expressed on the surface of immune cells.Eventually, effector cells cannot be activated via FcγR (Ierino et al., 1993).First, we investigated the effect of sCD32 on activating FcγR-dependent reactive oxygen species (ROS) release from IC-activated neutrophils (Supplementary Materials and Methods online). sCD32 inhibited IC-induced neutrophil ROS production in a dose-dependent manner (Figure 1a).In detail, compared with pos. control, 0.01, 0.1, and 0.5 mg ml-1 sCD32 significantly reduced ROS production by 30, 65, and 75%, resp.Next, we tested whether sCD32 could hinder dermal-epidermal separation in an ex vivo model of autoimmune bullous dermatoses.Accordingly, in the presence of leukocytes, sCD32 successfully impaired FcγR-dependent dermal-epidermal separation on cryosections of human skin incubated with sera containing pathogenic antibodies against DEJ structures (Figure 1b and c; Supplementary Materials and Methods online).To validate this ex vivo inhibitory activity of sCD32 on antibody-induced tissue injury in vivo, we next induced exptl. EBA in mice by immunization with vWFA2 (Supplementary Materials and Methods online).After immunization, mice were allocated to sCD32 or phosphate-buffered saline (PBS) treatment if individual mice had 2% or more of their body-surface area affected by skin lesions (Supplementary Materials and Methods online).Compared with PBS-injected mice, sCD32 treatment led to a significantly lower clin. disease severity (Figure 2a, left, *P<0.05, t-test).At inclusion to treatment (week 0), average disease scores were not different between the groups (3.4±0.21% and 3.4±0.20%) of affected body-surface area in PBS and sCD32 treatment, resp.Cumulative disease severity expressed as area under the curve during the entire observation period was also significantly lower in sCD32-treated mice as compared with PBS control mice (Figure 2a, right, P=0.031, t-test).At the end of the 4-wk treatment period, PBS-treated mice showed diffuse erythema and crusts on the ear and tail, and hair loss around the eyes (Figure 2b, left).In contrast, less erythema on the ear and no disease on tail or around the eyes in mice treated with sCD32 were observed (Figure 2b, right).Histol., mice treated with sCD32 showed a significant decrease in the dermal leukocyte infiltration, compared with PBS-treated mice (P<0.05, Figure 2c). sCD32 treatment also led to an ∼20% reduction in circulating antigen-specific autoantibodies compared with PBS-treated mice (Figures 2d, P=0.048; t-test), whereas total IgG levels were not significantly different (data not shown).At the same time point, all mice showed similar IgG deposits at DEJ as determined by direct immunofluorescence (Figure 2e, upper).Representative pictures of direct immunofluorescence show IgG deposits at DEJ (Figure 2e, down).This discrepancy between circulating and tissue bound autoantibodies may be because of their different half-lives. sCD32 treatment has also demonstrated beneficial effects in models of other autoantibody-mediated diseases, such as nephritis in lupus-prone NZB/NZW F(1) hybrid mice (Werwitzke et al., 2008) and joint inflammation in collagen-induced arthritis (Magnusson et al., 2008).On the basis of our observations ex vivo and in vivo, the therapeutic effect of sCD32 can be attributed to both direct and indirect mechanisms, which mean the inhibition of neutrophil function and autoantibody production, resp.On the basis of our observation of therapeutic efficacy in exptl. EBA, it is tempting to speculate that sCD32 binds to the in situ deposited ICs.This assumption, however, needs further exptl. exploration.Regarding the effect on autoantibody production, controversial results have been reported.In the lupus-prone NZM/NZW mouse model neither prophylactic nor therapeutic treatment with sCD32 affected anti-double stranded DNA serum titers (Werwitzke et al., 2008).In contrast, sCD32 suppressed secondary and primary in vitro antibody responses (Varin et al., 1989) and caused a temporary decrease in collagen-specific autoantibodies in CIA (Magnusson et al., 2008).In support of these later observations, we here report a sustained reduction of antigen-specific but not of total circulating IgG in immunization-induced EBA.This effect may be mediated through a blockade of the IgG2a-mediated enhancement of antibody and T-cell responses via increased antigen presentation to CD4+ T cells by FcγR-expressing antigen-presenting cells (Getahun et al., 2004).Taken together, our findings provide evidence for a beneficial role of sCD32 in exptl. EBA.As this model mostly reflects the inflammatory variant of EBA, our findings may pave the way for its clin. application in patients with autoimmune bullous dermatoses, where disease manifestation depends on an interaction of ICs with effector myeloid cells.
3
News (Medical) associated with Valziflocept12 Aug 2025
- Topline results from pivotal Phase 3 INDIGO trial in Immunoglobulin G4-Related Disease expected around year-end 2025 -
- Completed enrollment of Phase 2 MoonStone trial in Relapsing Multiple Sclerosis; results expected early in the fourth quarter 2025 -
- Enrollment of Phase 2 SunStone trial in Systemic Lupus Erythematosus expected to be completed by year-end 2025; topline results expected mid-2026 -
- Cash, cash equivalents and investments of $274.9 million as of June 30, 2025, expected to provide cash runway into the fourth quarter of 2026 -
WALTHAM, Mass., Aug. 12, 2025 (GLOBE NEWSWIRE) -- Zenas BioPharma, Inc. (“Zenas” or the “Company”) (Nasdaq: ZBIO), a clinical-stage global biopharmaceutical company committed to being a leader in the development and commercialization of transformative therapies for autoimmune diseases, today reported financial results for the second quarter ended June 30, 2025, and provided recent corporate updates.
“We are very pleased with the rapid advancement of our broad obexelimab development program, including the completion of enrollment for the Phase 2 MoonStone trial in patients with Relapsing Multiple Sclerosis this past quarter. We look forward to reporting the results from the primary analysis of the trial, and importantly, the topline results from the Phase 3 INDIGO trial of obexelimab in patients with IgG4-RD,” said Lonnie Moulder, Founder and Chief Executive Officer of Zenas. “Given the differentiated profile of obexelimab, along with our extensive development capabilities and commercialization experience, we are well positioned to execute on the significant opportunity ahead to potentially impact the lives of patients living with autoimmune diseases worldwide.”
Recent corporate highlights
Obexelimab, a CD-19 x FcγRIIb inhibitor of B cell function
Immunoglobulin G4-Related Disease (IgG4-RD): Advanced the Phase 3 INDIGO trial, a global registration-directed, multicenter, randomized, double-blind, placebo-controlled trial, to evaluate the efficacy and safety of obexelimab in patients with IgG4-RD. INDIGO is the largest clinical trial conducted in patients living with IgG4-RD to date. Target enrollment of the INDIGO trial concluded in November 2024, and Zenas expects to report topline results around year-end 2025. Relapsing Multiple Sclerosis (RMS): Completed enrollment of the Phase 2 MoonStone trial, a multicenter, randomized, double-blind, placebo-controlled trial, to evaluate the efficacy and safety of obexelimab in patients with RMS. Zenas expects to report results from this trial, including the 12-week primary endpoint results, early in the fourth quarter of 2025.Systemic Lupus Erythematosus (SLE): Continued enrollment of the Phase 2 SunStone trial, a multicenter, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of obexelimab in patients with SLE. Zenas expects to complete enrollment of the Phase 2 SunStone trial by year-end 2025 and report topline results in mid-2026.
Second quarter 2025 financial results
As of June 30, 2025, the Company’s cash, cash equivalents and investments were $274.9 million. The Company expects that its cash, cash equivalents and investments, as of June 30, 2025, will fund its operating expenses and capital expenditure requirements into the fourth quarter of 2026.Research and development (R&D) expenses were $43.0 million for the quarter ended June 30, 2025, compared to $33.8 million for the quarter ended June 30, 2024. The increase of $9.2 million in R&D expenses primarily relates to an increase in costs related to the clinical development of obexelimab and an increase in personnel costs partially offset by a decrease in costs related to our partnered programs.General and administrative (G&A) expenses were $12.1 million for the quarter ended June 30, 2025, compared to $5.9 million for the quarter ended June 30, 2024. The increase of $6.2 million in G&A expenses was due to an increase in personnel costs, including stock-based compensation expense, pre-commercialization activities including hiring and other expenses associated with operating as a public company.Net loss was $52.2 million for the quarter ended June 30, 2025, compared to net loss of $38.0 million for the quarter ended June 30, 2024.
About ObexelimabObexelimab is a bifunctional monoclonal antibody designed to bind both CD19 and FcγRIIb, which are broadly present across B cell lineage, to inhibit the activity of cells that are implicated in many autoimmune diseases without depleting them. This unique mechanism of action and self-administered, subcutaneous injection regimen may broadly and effectively address the pathogenic role of B cell lineage in chronic autoimmune disease.
Obexelimab has been evaluated in five completed clinical trials in a total of 198 subjects who received obexelimab either as an intravenous infusion or as a subcutaneous injection. Obexelimab was well tolerated and demonstrated pharmacologic activity across these five clinical trials, providing the Company an initial clinical proof of concept for obexelimab as a potent B cell inhibitor for the treatment of patients living with certain autoimmune diseases. Currently, Zenas is conducting multiple Phase 2 and Phase 3 trials of obexelimab in several autoimmune diseases including Immunoglobulin G4-Related Disease, Relapsing Multiple Sclerosis and Systemic Lupus Erythematosus.
About Zenas BioPharma, Inc.Zenas is a clinical-stage global biopharmaceutical company committed to becoming a leader in the development and commercialization of transformative therapies for patients with autoimmune diseases. Our core business strategy combines our experienced leadership team with a disciplined product candidate acquisition approach to identify, acquire and develop product candidates globally that we believe can provide superior clinical benefits to patients living with autoimmune diseases. Zenas’ lead product candidate, obexelimab, is a bifunctional monoclonal antibody designed to bind both CD19 and FcγRIIb, which are broadly present across B cell lineage, to inhibit the activity of cells that are implicated in many autoimmune diseases without depleting them. We believe that obexelimab’s unique mechanism of action and self-administered, subcutaneous injection regimen may broadly and effectively address the pathogenic role of B cell lineage in chronic autoimmune disease. For more information about Zenas BioPharma, please visit www.zenasbio.com and follow us on LinkedIn.
Forward looking statementsThis press release contains “forward-looking statements” which involve risks, uncertainties and contingencies, many of which are beyond the control of the Company, which may cause actual results, performance, or achievements to differ materially from anticipated results, performance, or achievements. All statements other than statements of historical facts contained in this press release are forward-looking statements. In some cases, forward-looking statements can be identified by terms such as “may,” “will,” “should,” “expect,” “plan,” “anticipate,” “could,” “intend,” “target,” “project,” “contemplate,” “believe,” “estimate,” “predict,” “potential” or “continue” or the negative of these terms or other similar expressions, although not all forward-looking statements contain these words. Forward-looking statements include, but are not limited to, statements concerning the timing and results of ongoing and future clinical trials, including expectations on the timing of reporting INDIGO trial topline results, results of the 12-week primary endpoint analysis for the MoonStone trial and the anticipated timing of completing enrollment and reporting topline results for the SunStone trial; the ability to potentially impact the treatment of autoimmune diseases; its growth strategy; and cash runway guidance. The forward-looking statements in this press release speak only as of the date of this press release and are subject to a number of known and unknown risks, uncertainties and assumptions that could cause the Company’s actual results to differ materially from those anticipated in the forward-looking statements, including, but not limited to: the Company’s limited operating history, incurrence of substantial losses since the Company’s inception and anticipation of incurring substantial and increasing losses for the foreseeable future; the Company’s need for substantial additional financing to achieve the Company’s goals; the uncertainty of clinical development, which is lengthy and expensive, and characterized by uncertain outcomes, and risks related to additional costs or delays in completing, or failing to complete, the development and commercialization of the Company’s current product candidates or any future product candidates; delays or difficulties in the enrollment and dosing of patients in clinical trials; the impact of any significant adverse events or undesirable side effects caused by the Company’s product candidates; potential competition, including from large and specialty pharmaceutical and biotechnology companies, many of which already have approved therapies in the Company’s current indications; the Company’s ability to realize the benefits of the Company’s current or future collaborations or licensing arrangements and ability to successfully consummate future partnerships; the Company’s ability to obtain regulatory approval to commercialize any product candidate in the United States or any other jurisdiction, and the risk that any such approval may be for a more narrow indication than the Company seeks; the Company’s dependence on the services of the Company’s senior management and other clinical and scientific personnel, and the Company’s ability to retain these individuals or recruit additional management or clinical and scientific personnel; the Company’s ability to grow the Company’s organization, and manage the Company’s growth and expansion of the Company’s operations; risks related to the manufacturing of the Company’s product candidates, which is complex, and the risk that the Company’s third-party manufacturers may encounter difficulties in production; the Company’s ability to obtain and maintain sufficient intellectual property protection for the Company’s product candidates or any future product candidates the Company may develop; the Company’s reliance on third parties to conduct the Company’s preclinical studies and clinical trials; the Company’s compliance with the Company’s obligations under the licenses granted to the Company by others, for the rights to develop and commercialize the Company’s product candidates; significant political, trade, regulatory developments, including changes in relations between the U.S. and China; risks related to the operations of the Company’s suppliers, many of which are located outside of the United States, including the Company’s current sole contract manufacturing organization for drug substance and drug product, WuXi Biologics (Hong Kong) Limited, which is located in China; and other risks and uncertainties described in the section “Risk Factors” in the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2025, as well as other information we file with the Securities and Exchange Commission. The forward-looking statements in this press release are inherently uncertain, speak only as of the date of this press release and may prove incorrect. These statements are based upon information available to the Company as of the date of this press release and while the Company believes such information forms a reasonable basis for such statements, such information may be limited or incomplete, and our statements should not be read to indicate that the Company has conducted an exhaustive inquiry into, or review of, all potentially available relevant information. Because forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified and some of which are beyond the Company’s control, these forward-looking statements should not be relied upon as guarantees of future events. The events and circumstances reflected in the forward-looking statements may not be achieved or occur and actual future results, levels of activity, performance and events and circumstances could differ materially from those projected in the forward-looking statements. Moreover, the Company operates in an evolving environment. New risks and uncertainties may emerge from time to time, and management cannot predict all risks and uncertainties. Except as required by applicable law, the Company does not undertake to publicly update or revise any forward-looking statements contained herein, whether as a result of any new information, future events, changed circumstances or otherwise.
The Zenas BioPharma word mark, logo mark, and the “lightning bolt” design are trademarks of Zenas BioPharma, Inc. or its affiliated companies.
Zenas BioPharma, Inc. CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS (in thousands except share and per share amounts) Unaudited
Three Months Ended June 30, 2025 2024 Revenue:
License and collaboration revenue $— $— Total revenue — — Operating expenses:
Research and development 43,027 33,807 General and administrative 12,136 5,895 Total operating expenses 55,163 39,702 Loss from operations (55,163) (39,702) Other income, net:
Other income, net 2,960 1,725 Total other income, net 2,960 1,725 Income tax (provision) benefit (20) — Net loss to common stockholders $(52,223) $(37,977) Net loss per share attributable to common stockholders - basic and diluted $(1.25) $(24.23) Weighted-average common stock outstanding - basic and diluted 41,865,400 1,567,269
Zenas BioPharma, Inc.SELECTED CONSOLIDATED BALANCE SHEET DATA(in thousands)Unaudited
June 30
2025 Cash, cash equivalents and investments $274,893 Working capital 225,359 Total assets 293,085 Accumulated deficit (473,187)Total stockholders’ equity 239,626
Investor and Media Contact:Argot PartnersZenas@argotpartners.com
Phase 2Phase 3Financial StatementImmunotherapyClinical Result
15 May 2025
- Topline results from pivotal Phase 3 INDIGO trial in Immunoglobulin G4-Related Disease expected around year-end 2025 - - Phase 2 MoonStone trial in Relapsing Multiple Sclerosis enrollment concluding; topline results expected early in the fourth quarter 2025 - - Enrollment of Phase 2 SunStone trial in Systemic Lupus Erythematosus expected to be completed by year-end 2025; topline results expected mid-2026 - - Strengthened leadership team with appointments of Lisa von Moltke, M.D., Head of Research and Development and Chief Medical Officer, and Haley Laken, Ph.D., Chief Scientific Officer - - Cash, cash equivalents and investments of $314.2 million as of March 31, 2025, expected to provide financial runway into the fourth quarter of 2026 - WALTHAM, Mass., May 15, 2025 (GLOBE NEWSWIRE) -- Zenas BioPharma, Inc. (“Zenas” or the “Company”) (Nasdaq: ZBIO), a clinical-stage global biopharmaceutical company committed to being a leader in the development and commercialization of therapies for autoimmune diseases, today reported financial results for the first quarter ended March 31, 2025, and provided recent corporate updates. “We are pleased with the continued momentum of our obexelimab program across ongoing Phase 2 and Phase 3 clinical trials, for which we expect to report topline results later this year from trials in patients with relapsing multiple sclerosis and IgG4-RD,” said Lonnie Moulder, Founder and Chief Executive Officer of Zenas. “With a strengthened team following the recent additions of Lisa and Haley, we are well positioned to execute on our clinical trials and advance obexelimab as a differentiated B cell inhibitor with a potentially safer, more potent and convenient profile for patients.” Recent corporate highlights Obexelimab, a CD-19 x FcγRIIb inhibitor of B cell function Immunoglobulin G4-Related Disease (IgG4-RD): Advanced the Phase 3 INDIGO trial, a global registration-directed, multicenter, randomized, double-blind, placebo-controlled trial, to evaluate the efficacy and safety of obexelimab in patients with IgG4-RD. INDIGO is the largest clinical trial conducted in patients living with IgG4-RD to date. In the fourth quarter of 2024, Zenas completed the target enrollment of the INDIGO trial and expects to report topline results from the INDIGO trial around year-end 2025.Relapsing Multiple Sclerosis (RMS): Patient screening concluding with the final subject expected to be enrolled in early-June in the Phase 2 MoonStone trial, a multicenter, randomized, double-blind, placebo-controlled trial, to evaluate the efficacy and safety of obexelimab in patients with RMS. The Company expects to report topline results from this trial, including the 12-week primary endpoint results, early in the fourth quarter of 2025.Systemic Lupus Erythematosus (SLE): Continued enrolling in the Phase 2 SunStone trial, a multicenter, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of obexelimab in patients with SLE. Zenas expects to complete enrollment in this trial by year-end 2025 and report topline results in mid-2026. Other corporate highlights Beyond progress with obexelimab, during the first quarter and more recently, the Company: Strengthened its leadership team by appointing Lisa von Moltke, M.D., as Head of Research and Development and Chief Medical Officer, and Haley Laken, Ph.D., as Chief Scientific Officer. Dr. von Moltke brings over 30 years of U.S. and international drug development experience spanning multiple therapeutic areas, including autoimmune diseases, early- and late-stage clinical development, and commercialization at large and emerging growth companies. Dr. Laken brings over 25 years of leadership experience in research, development operations, research and development strategy and business development.Out-licensed regional rights to its thyroid eye disease program, including ZB001, an insulin-like growth factor-1 receptor (anti-IGF-1R) monoclonal antibody, to Zai Lab (Zai). Zenas received an upfront payment and is eligible to receive milestone payments and royalties in the future, as consideration for an exclusive sublicense to Zai to develop and commercialize ZB001 and related programs in Greater China. First quarter 2025 financial results As of March 31, 2025, the Company’s cash, cash equivalents and investments was $314.2 million. The Company expects that its cash, cash equivalents and investments, as of March 31, 2025, will fund its operating expenses and capital expenditure requirements into the fourth quarter of 2026.License and collaboration revenue was $10.0 million for the quarter ended March 31, 2025, related to the one-time non-refundable upfront cash payment received in connection with the sublicense agreement with Zai. The Company did not recognize any license and collaboration revenue during the quarter ended March 31, 2024.Research and development (R&D) expenses were $34.9 million for the quarter ended March 31, 2025, compared to $22.6 million for the quarter ended March 31, 2024. The increase of $12.3 million in R&D expenses primarily relates to an increase in costs related to the clinical development and manufacturing of obexelimab.General and administrative (G&A) expenses were $12.4 million for the quarter ended March 31, 2025, compared to $4.9 million for the quarter ended March 31, 2024. The increase of $7.5 million in G&A expenses was due to an increase in personnel costs, including stock-based compensation expenses, pre-commercialization activities including hiring and other expenses including costs associated with operating as a public company.Net loss was $33.6 million for the quarter ended March 31, 2025, compared to net loss of $27.8 million for the quarter ended March 31, 2024. About ObexelimabObexelimab is a bifunctional monoclonal antibody designed to bind both CD19 and FcγRIIb, which are broadly present across B cell lineage, to inhibit the activity of cells that are implicated in many autoimmune diseases without depleting them. This unique mechanism of action and self-administered, subcutaneous injection regimen may broadly and effectively address the pathogenic role of B cell lineage in chronic autoimmune disease. Obexelimab has been evaluated in five completed clinical trials in a total of 198 patients who received obexelimab either as an intravenous infusion or as a subcutaneous injection. Obexelimab was well tolerated and demonstrated clinical activity across these five clinical trials, providing the Company an initial clinical proof of concept for obexelimab as a potent B cell inhibitor for the treatment of patients living with certain autoimmune diseases. Currently, Zenas is conducting multiple Phase 2 and Phase 3 trials of obexelimab in several autoimmune diseases including Immunoglobulin G4-Related Disease, Relapsing Multiple Sclerosis and Systemic Lupus Erythematosus. About Zenas BioPharma, Inc.Zenas is a clinical-stage global biopharmaceutical company committed to becoming a leader in the development and commercialization of transformative therapies for patients with autoimmune diseases. Our core business strategy combines our experienced leadership team with a disciplined product candidate acquisition approach to identify, acquire and develop product candidates globally that we believe can provide superior clinical benefits to patients living with autoimmune diseases. Zenas’ lead product candidate, obexelimab, is a bifunctional monoclonal antibody designed to bind both CD19 and FcγRIIb, which are broadly present across B cell lineage, to inhibit the activity of cells that are implicated in many autoimmune diseases without depleting them. We believe that obexelimab’s unique mechanism of action and self-administered, subcutaneous injection regimen may broadly and effectively address the pathogenic role of B cell lineage in chronic autoimmune disease. For more information about Zenas BioPharma, please visit www.zenasbio.com and follow us on LinkedIn. Forward looking statementsThis press release contains “forward-looking statements” which involve risks, uncertainties and contingencies, many of which are beyond the control of the Company, which may cause actual results, performance, or achievements to differ materially from anticipated results, performance, or achievements. All statements other than statements of historical facts contained in this press release are forward-looking statements. In some cases, forward-looking statements can be identified by terms such as “may,” “will,” “should,” “expect,” “plan,” “anticipate,” “could,” “intend,” “target,” “project,” “contemplate,” “believe,” “estimate,” “predict,” “potential” or “continue” or the negative of these terms or other similar expressions, although not all forward-looking statements contain these words. Forward-looking statements include, but are not limited to, statements concerning the timing and results of ongoing and future clinical trials, including expectations on the timing of reporting INDIGO trial topline results, the last patient to be enrolled in and the 12-week primary endpoint data for the MoonStone trial and the anticipated timing of completing enrollment and reporting topline results for the SunStone trial; its growth strategy; and cash runway guidance. The forward-looking statements in this press release speak only as of the date of this press release and are subject to a number of known and unknown risks, uncertainties and assumptions that could cause the Company’s actual results to differ materially from those anticipated in the forward-looking statements, including, but not limited to: the Company’s limited operating history, incurrence of substantial losses since the Company’s inception and anticipation of incurring substantial and increasing losses for the foreseeable future; the Company’s need for substantial additional financing to achieve the Company’s goals; the uncertainty of clinical development, which is lengthy and expensive, and characterized by uncertain outcomes, and risks related to additional costs or delays in completing, or failing to complete, the development and commercialization of the Company’s current product candidates or any future product candidates; delays or difficulties in the enrollment and dosing of patients in clinical trials; the impact of any significant adverse events or undesirable side effects caused by the Company’s product candidates; potential competition, including from large and specialty pharmaceutical and biotechnology companies, many of which already have approved therapies in the Company’s current indications; the Company’s ability to realize the benefits of the Company’s current or future collaborations or licensing arrangements and ability to successfully consummate future partnerships; the Company’s ability to obtain regulatory approval to commercialize any product candidate in the United States or any other jurisdiction, and the risk that any such approval may be for a more narrow indication than the Company seeks; the Company’s dependence on the services of the Company’s senior management and other clinical and scientific personnel, and the Company’s ability to retain these individuals or recruit additional management or clinical and scientific personnel; the Company’s ability to grow the Company’s organization, and manage the Company’s growth and expansion of the Company’s operations; risks related to the manufacturing of the Company’s product candidates, which is complex, and the risk that the Company’s third-party manufacturers may encounter difficulties in production; the Company’s ability to obtain and maintain sufficient intellectual property protection for the Company’s product candidates or any future product candidates the Company may develop; the Company’s reliance on third parties to conduct the Company’s preclinical studies and clinical trials; the Company’s compliance with the Company’s obligations under the licenses granted to the Company by others, for the rights to develop and commercialize the Company’s product candidates; significant political, trade, regulatory developments, including changes in relations between the U.S. and China; risks related to the operations of the Company’s suppliers, many of which are located outside of the United States, including the Company’s current sole contract manufacturing organization for drug substance and drug product, WuXi Biologics (Hong Kong) Limited, which is located in China; and other risks and uncertainties described in the section “Risk Factors” in the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2025, as well as other information we file with the Securities and Exchange Commission. The forward-looking statements in this press release are inherently uncertain, speak only as of the date of this press release and may prove incorrect. These statements are based upon information available to the Company as of the date of this press release and while the Company believes such information forms a reasonable basis for such statements, such information may be limited or incomplete, and our statements should not be read to indicate that the Company has conducted an exhaustive inquiry into, or review of, all potentially available relevant information. Because forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified and some of which are beyond the Company’s control, these forward-looking statements should not be relied upon as guarantees of future events. The events and circumstances reflected in the forward-looking statements may not be achieved or occur and actual future results, levels of activity, performance and events and circumstances could differ materially from those projected in the forward-looking statements. Moreover, the Company operates in an evolving environment. New risks and uncertainties may emerge from time to time, and management cannot predict all risks and uncertainties. Except as required by applicable law, the Company does not undertake to publicly update or revise any forward-looking statements contained herein, whether as a result of any new information, future events, changed circumstances or otherwise. The Zenas BioPharma word mark, logo mark, and the “lightning bolt” design are trademarks of Zenas BioPharma, Inc. or its affiliated companies. Zenas BioPharma, Inc.CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS(in thousands except share and per share amounts)Unaudited
Three Months Ended March 31, 2025 2024 Revenue:
License and collaboration revenue $10,000 $— Total revenue 10,000 — Operating expenses:
Research and development 34,915 22,645 General and administrative 12,415 4,933 Total operating expenses 47,330 27,578 Loss from operations (37,330) (27,578)Other income (expense), net:
Other income (expense), net 3,552 (222)Total other income (expense), net 3,552 (222)Income tax benefit 205 — Net loss to common stockholders $(33,573) $(27,800)Net loss per share attributable to common stockholders - basic and diluted $(0.80) $(17.89)Weighted-average common stock outstanding - basic and diluted 41,800,802 1,554,087
Zenas BioPharma, Inc.SELECTED CONSOLIDATED BALANCE SHEET DATA(in thousands)Unaudited
March 31, 2025Cash, cash equivalents and investments $314,214 Working capital 268,675 Total assets 333,766 Accumulated deficit (420,964)Total stockholders’ equity 284,317
Investor and Media Contact:Argot PartnersZenas@argotpartners.com
Phase 2Phase 3Financial StatementExecutive ChangePhase 1
19 Jan 2022
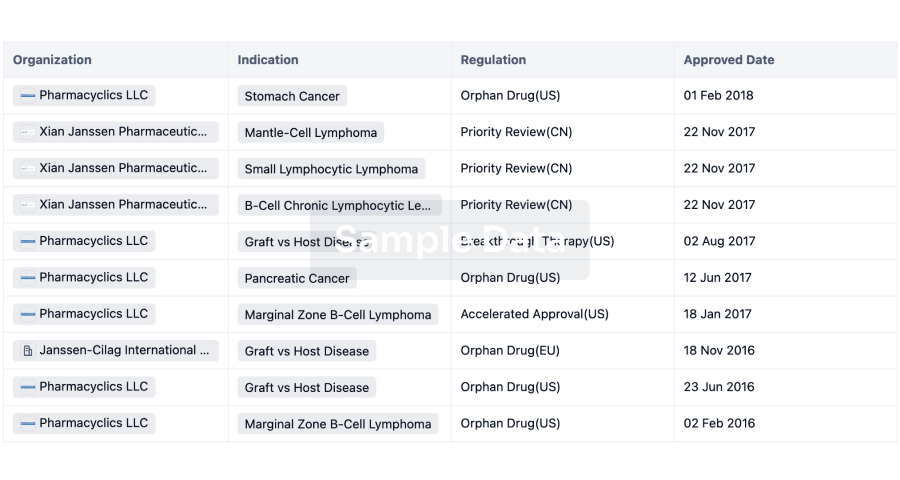
BioInvent International AB ("BioInvent") (Nasdaq Stockholm:BINV), a biotech company focused on the discovery and development of novel and first-in-class immune-modulatory antibodies for cancer immunotherapy, today announces that its anti-FcyRllB antibody BI-1206 has been granted Orphan Drug Designation (ODD) by the U.S. Food and Drug Administration (FDA) for the treatment of follicular lymphoma (FL), the most common form of slow-growing Non-Hodgkin lymphoma.
The FDA's Office of Orphan Drug Products grants orphan status to support the development of medicines for rare disorders that affect fewer than 200,000 people in the U.S. ODD provides benefits, including market exclusivity upon regulatory approval, exemption of FDA biologic license application fee and tax credits for qualified clinical trials. BI-1206 previously received ODD from the FDA for the treatment of mantle cell lymphoma (MCL) in January 2019.
BI-1206 is BioInvent's lead drug candidate and is currently being investigated in two Phase 1/2 trials. One is evaluating the BI-1206 combination with rituximab for the treatment of Non-Hodgkin lymphoma, which includes patients with FL, MCL and marginal zone lymphoma (MZL) who have relapsed or are refractory to rituximab. A second Phase 1/2 trial is investigating BI-1206 in combination with anti-PD1 therapy Keytruda® (pembrolizumab) in solid tumors.
"The granting of orphan drug status for BI-1206 for follicular lymphoma is another important step forward in the development of our lead drug candidate. The clinical update we presented recently clearly suggests BI-1206 may restore the response to rituximab in patients who have few treatment alternatives, with the results in follicular lymphoma being particularly impressive. We are looking forward to continuing to progress this anti-FcγRIIB antibody through clinical development to meet the needs of this underserved patient population," said Martin Welschof, CEO of BioInvent.
About BioInvent
BioInvent International AB (Nasdaq Stockholm: BINV) is a clinical-stage biotech company that discovers and develops novel and first-in-class immuno-modulatory antibodies for cancer therapy, with currently three drug candidates in four ongoing clinical programs in Phase 1/2 trials for the treatment of hematological cancer and solid tumors, respectively and a fifth program just initiating clinical development. The Company's validated, proprietary F.I.R.S.T™ technology platform simultaneously identifies both targets and the antibodies that bind to them, generating many promising new drug candidates to fuel the Company's own clinical development pipeline or for additional licensing and partnering.
The Company generates revenues from research collaborations and license agreements with multiple top-tier pharmaceutical companies, as well as from producing antibodies for third parties in the Company's fully integrated manufacturing unit.
CollaborateAntibodyOrphan DrugFirst in ClassImmunotherapy
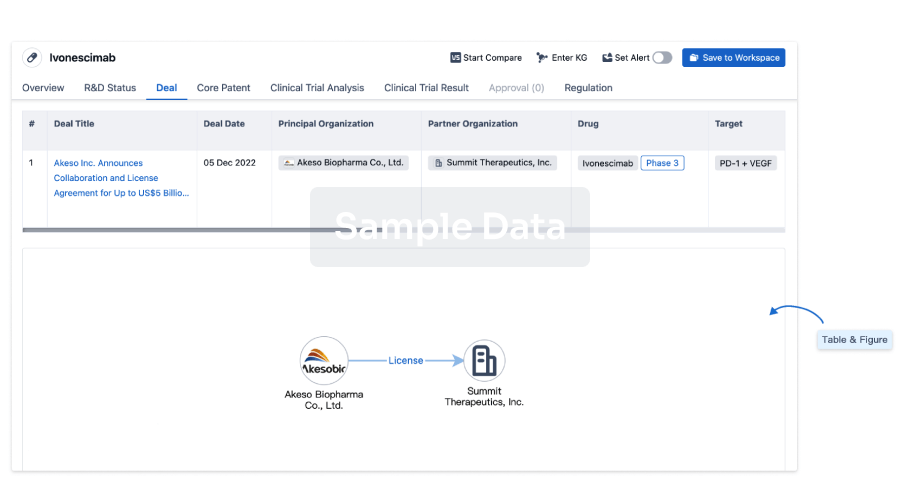
100 Deals associated with Valziflocept
Login to view more data
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D11339 | - | - | - |
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Glomerulonephritis, IGA | Phase 2 | - | 31 Dec 2015 | |
| Purpura, Thrombocytopenic, Idiopathic | Phase 2 | Belgium | - | |
| Purpura, Thrombocytopenic, Idiopathic | Phase 2 | Germany | - | |
| Purpura, Thrombocytopenic, Idiopathic | Phase 2 | Poland | - | |
| Purpura, Thrombocytopenic, Idiopathic | Phase 2 | Russia | - | |
| Purpura, Thrombocytopenic, Idiopathic | Phase 2 | Ukraine | - |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
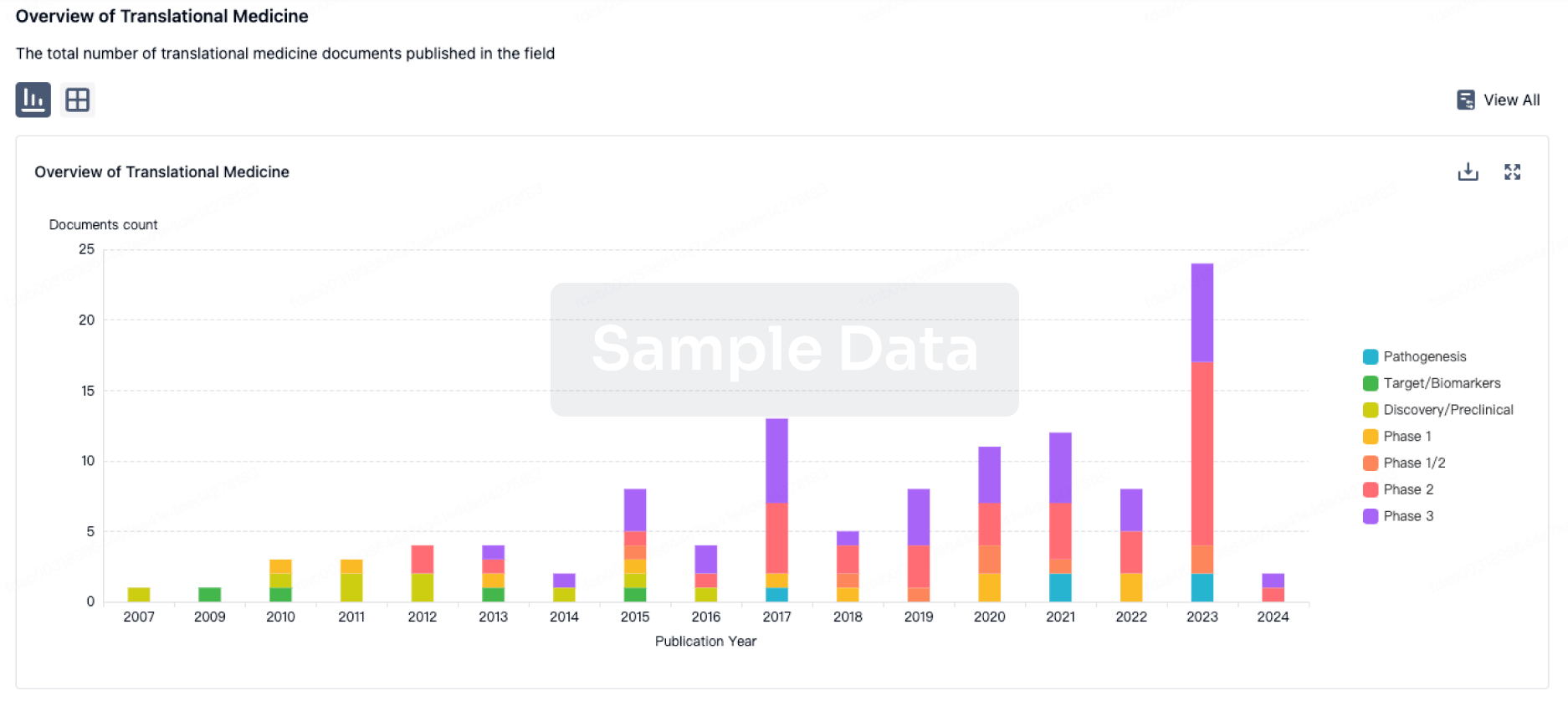
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
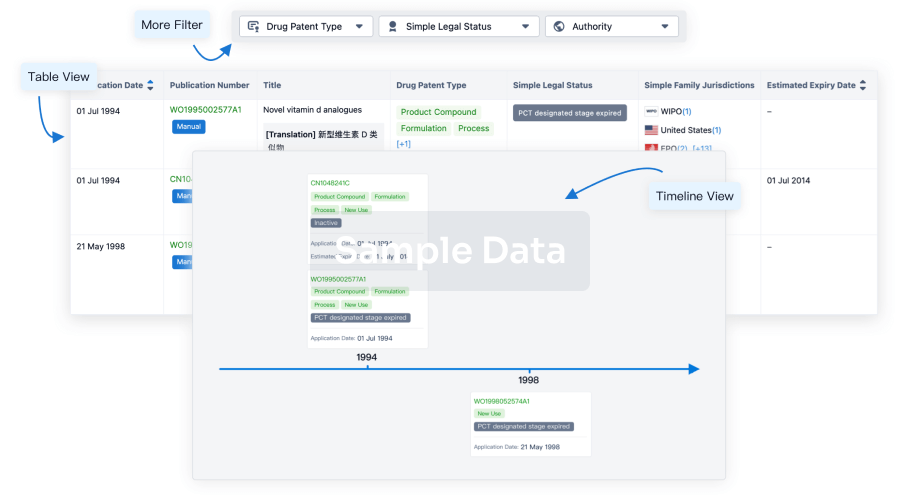
Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
Approval
Accelerate your research with the latest regulatory approval information.
login
or
Biosimilar
Competitive landscape of biosimilars in different countries/locations. Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


