Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and its life-threatening complication, pulmonary embolism (PE), are among the most frequent causes of morbidity and mortality in developed countries. In the United States alone, the number of deaths due to VTE approaches 300,000 annually [1]. Blood flow restriction or stasis is considered a major factor driving DVT [2]. Regardless of its initial cause (bed-ridden position, long-haul flights, limb paralysis, etc.), delayed blood renewal in stasis is believed to produce limited oxygen supply to the vein walls (hypoxia), especially in the valvular sinus, which triggers thrombus development [2].
Certain circumstances may lead to an imbalance between tissue demand and actual oxygen supply. This can be caused by tissue requirement exceeding the capacity of oxygen delivery systems (e.g., physical exercise) or inadequate oxygen content in the ambient air. The latter case can be found in situations such as mountain climbing or commercial flights where the cabin is pressurized to a level corresponding to an altitude of 1.5 – 2.5 kilometers [3, 4]. Indeed, clinical studies have linked recent air travel of >4 hours to increased risk of developing DVT [5] and traveling patients with pro-thrombotic mutations predisposing to DVT are at even higher risk for thrombosis [6]. Moreover, an "absolute" risk for VTE in a ratio of 1 event per about 4,500 flights has been reported [7]. Even in healthy individuals, oxyhemoglobin saturation is decreased by 5 – 10% during flight, whereas in patients with chronic obstructive pulmonary disease a greater decrease has been reported [4].
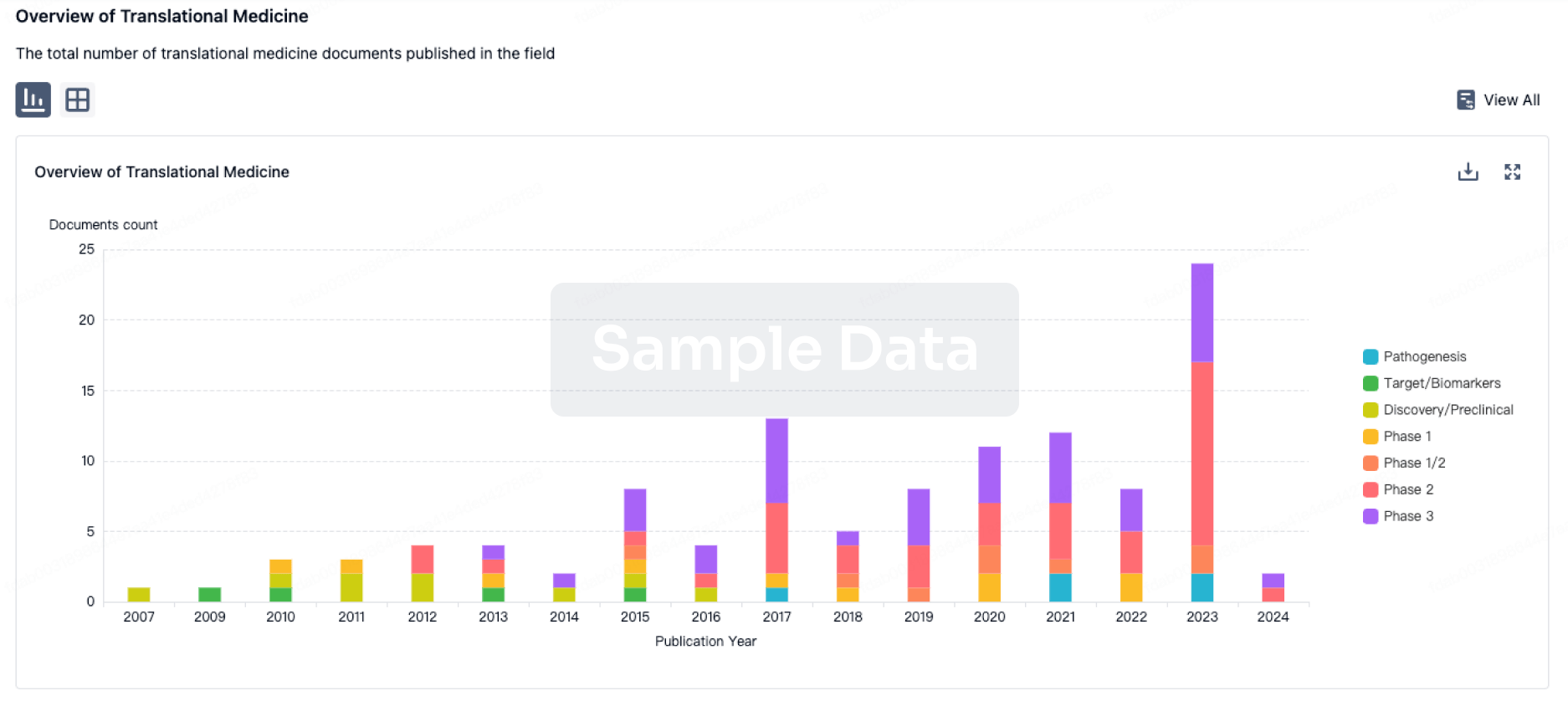
In the majority of cases, hypoxia is followed by restoration of oxygen supply, i.e., reoxygenation. Hypoxia-reoxygenation (H/R), which is known to be harmful to tissues [8, 9], is proposed to be an exacerbating factor for thrombus development in veins although this causal relationship has not been directly proven. A crucial role of the reoxygenation phase in DVT can be suggested because thrombotic events frequently occur after landing [7, 10]. We report that exposure to 6% oxygen for 24 hours followed by 1–3 hours of reoxygenation in normal room air led to significantly increased thrombus prevalence in a mouse model of DVT. Eleven of 15 mice (73%) developed a thrombus after one hour stenosis of the inferior vena cava (IVC) as compared to 1 of 8 (13%) in control animals maintained in normoxic conditions (Figure A,B) (P<0.01). Weight and length of the thrombi from animals that underwent H/R significantly exceeded those in the control group. Thus, mice that were subjected to IVC stenosis after H/R demonstrated a clear pro-thrombotic phenotype.
Figure
Hypoxia/Reoxygenation (H/R) promotes DVT. Mice subjected to H/R or normoxia followed by 1 h of IVC stenosis were euthanized and thrombi examined. Thrombus weight and length are shown in WT (normoxic), n=8; WT (H/R), n=15; WT (H/R + GPG-290), n=6; TgGP1bα/IL4R, ...
Endothelial cells contain Weibel-Palade bodies (WPB) that store multiple thrombosis- and inflammation-related constituents, such as von Willebrand factor (VWF) and P-selectin [11–13] and hypoxia is a known inducer of WPB secretion [14]. von Willebrand factor is a large multimeric protein that mediates platelet adhesion and recruitment via its binding to receptors GPIbα and GPIIb-IIIa on the platelet surface [15]. Using a mouse model, we have recently demonstrated that release of WPB is a central event in the initiation of DVT [16]. This implies that DVT is most likely a thrombo-inflammatory pathology rather than a disease entirely based on defects of the hemostatic system. Liberation of VWF and platelet recruitment through the VWF/GPIbα axis was of particular importance. Therefore, we hypothesized that H/R would activate these pathways and thus promote DVT. Indeed, we confirmed that exposure to hypoxia for 24 hours followed by reoxygenation significantly elevated plasma VWF levels in our hypoxia model (data not shown). We therefore tested whether H/R exerts its pro-thrombotic effect through VWF. We administered GPG-290, a chimeric protein that prevents GPIbα interaction with VWF to wild-type (WT) mice as well as utilized mice that lack either the extracellular domain of GPIbα or VWF. Infusion of GPG-290 abolished the pro-thrombotic effect of H/R (Figure A,B). Mice lacking the extracellular domain of GPIbα and VWF−/− mice were protected against H/R-promoted DVT (22 and 0% of mice with a thrombus, respectively; thrombus analysis is shown in figure C,D). Thus, VWF released from WPBs and platelet binding through GPIbα are likely implicated in H/R-induced DVT.
It has been reported that hypoxia does not induce a pro-coagulant shift sufficient to explain thrombosis [17, 18]. In our model, we have confirmed these reports as the time to clotting onset was increased and clotting rate reduced in recalcified whole blood samples after H/R (Figure E,F), suggesting slower fibrin formation compared to normoxic samples.
Here, we demonstrate that H/R accelerates thrombosis in a mouse model of DVT. Interestingly, increased incidence of DVT under H/R conditions occurs despite decreased ex vivo blood clotting. The process is dependent on VWF-mediated interactions indicating that H/R enhances WPB secretion initiating rapid thrombosis in the stenosis model [16]. Many factors are proposed to lead to DVT in long flights, such as hypoxia in the cabin, dehydration and motionless limbs [4]. We demonstrate that hypoxia is at least partially responsible for this unfortunate side effect of travel.