Request Demo
Last update 01 Mar 2026
Bevasiranib
Last update 01 Mar 2026
Overview
Basic Info
Drug Type siRNA |
Synonyms Bevasiranib sodium, CAND 5 |
Target |
Action inhibitors |
Mechanism VEGF-A inhibitors(Vascular endothelial growth factor A inhibitors), RNA interference |
Active Indication |
Originator Organization |
Active Organization |
Inactive Organization |
License Organization- |
Drug Highest PhasePhase 2 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Boost your research with our RNA technology data.
login
or
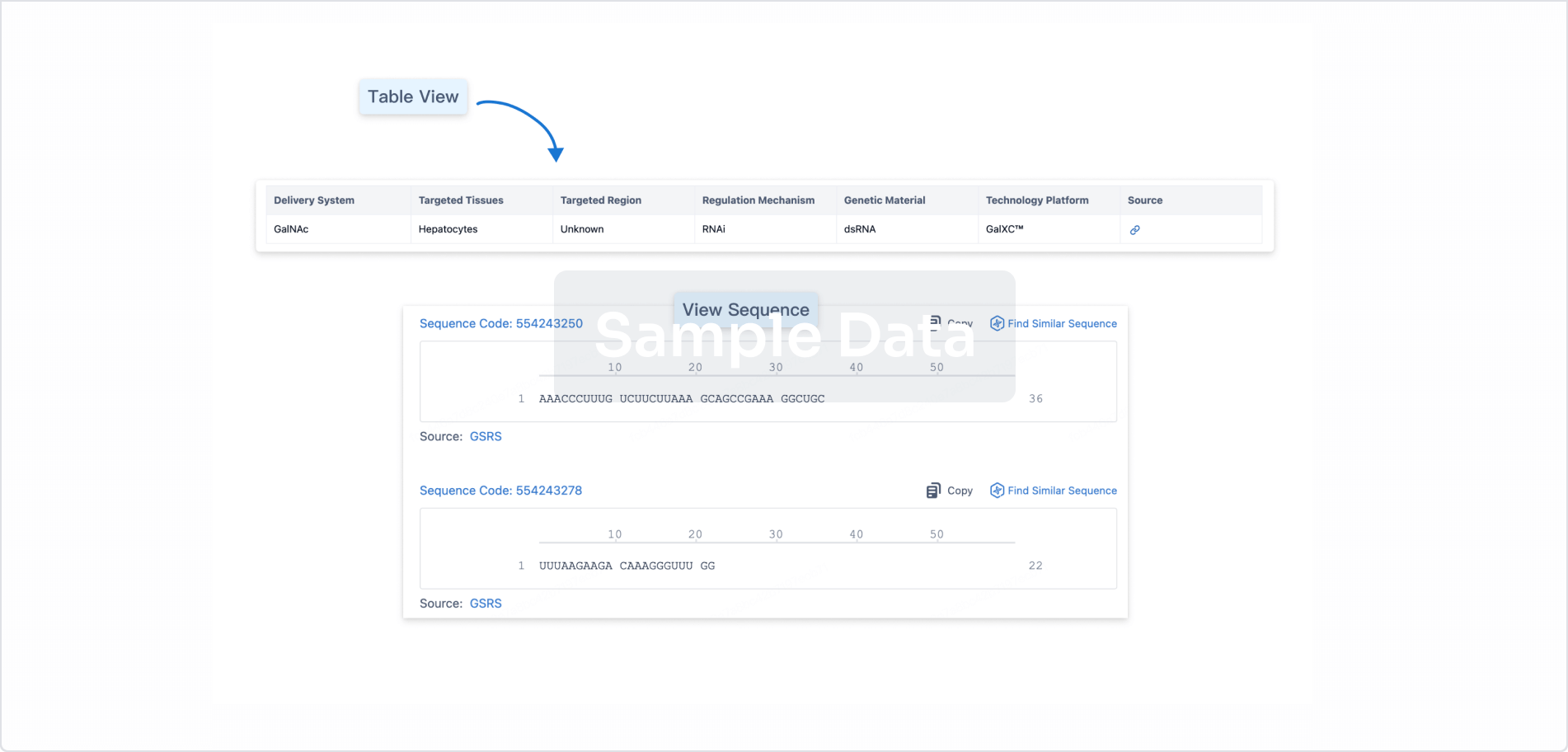
Sequence Code 29500879
Source: *****
Sequence Code 29500886
Source: *****
Related
5
Clinical Trials associated with BevasiranibNCT00557791
A Phase 3, Randomized, Double-masked, Parallel-assignment and Dose-finding Study of Intravitreal Bevasiranib Sodium, Administered Every 8 Weeks as Maintenance Therapy Following Three Injections of Lucentis® Compared With Lucentis® Monotherapy Every 4 Weeks in Patients With Exudative Age-Related Macular Degeneration (AMD).
The purpose of this study is to compare the safety and effectiveness of three doses of intravitreal bevasiranib sodium as maintenance therapy for Age-Related Macular Degeneration following initiation of anti-VEGF therapy with three doses of Lucentis®.
Start Date01 Nov 2009 |
Sponsor / Collaborator |
NCT00499590
A Phase 3, Randomized, Double-masked, Parallel-assignment Study of Intravitreal Bevasiranib Sodium, Administered Every 8 or 12 Weeks as Maintenance Therapy Following Three Injections of Lucentis® Compared With Lucentis® Monotherapy Every 4 Weeks in Patients With Exudative Age-Related Macular Degeneration (AMD).
The purpose of this study is to compare the safety and effectiveness of bevasiranib given either every 8 weeks or every 12 weeks after an initial pre-treatment with 3 injections of Lucentis® (ranibizumab injection) compared to Lucentis® given every 4 weeks to people with wet AMD. Patients will be assigned at random (like tossing a coin) to receive one of three treatments options for 104 weeks.
Start Date01 Aug 2007 |
Sponsor / Collaborator |
NCT00306904
A Phase II, Pharmacokinetic, Randomized, Double-Masked, Controlled, Dose Comparison Study of Cand5 for Intravitreal Injection for the Treatment of Diabetic Macular Edema
The purpose of this study is to evaluate the pharmacokinetics, safety and preliminary efficacy of 3 doses of Cand5. Cand5 is a small interfering RNA molecule that selectively silences the mRNA encoding for VEGF. The target population are patients with diabetic macular edema.
Start Date01 Jan 2006 |
Sponsor / Collaborator |
100 Clinical Results associated with Bevasiranib
Login to view more data
100 Translational Medicine associated with Bevasiranib
Login to view more data
100 Patents (Medical) associated with Bevasiranib
Login to view more data
5
Literatures (Medical) associated with Bevasiranib01 Mar 2011·Asian journal of andrologyQ2 · MEDICINE
Selective cell death mediated by small conditional RNAs: a novel therapeutic approach to cancer therapy
Q2 · MEDICINE
ArticleOA
Author: Oh, William K ; Tsao, Che-Kai
Targeted molecular therapy has been an elusive goal in the treatment of neoplastic diseases. While chemotherapy has improved the outcome of many cancers, a non-selective cytotoxic approach invariably causes damage to normal cells, resulting in side effects and limiting treatment efficacy. This is evident in the evolution of treatment for castration-resistant prostate cancer (CRPC). For instance, while mitoxantrone, docetaxel and cabazitaxel have all shown therapeutic activity and have been FDA-approved for use in CRPC, response rates and duration of benefit remain limited and side effects associated with treatment are significant. Thus the development of specific targeted therapeutic agents which minimize toxicity to normal cells while killing malignant cells has been a high-priority endeavor. Sipuleucel-T, the first therapeutic cancer vaccine to demonstrate effectiveness in a phase III clinical trial, uses native antigen-presenting cells after incubation with a novel prostate cancer antigen (prostatic acid phosphatase), inducing an immune response against castration-resistant cells. Kantoff et al.1 demonstrated that treatment of metastatic CRPC patients with sipuleucel-T resulted in a 22% reduction in the risk of death, and a 4.1-month improvement in median survival, compared with placebo. In addition, most treatment-related adverse events were transient and of low grade. Hence, increasing treatment target specificity may provide a desirable therapeutic effect while minimizing unwanted adverse events, in this case by inducing a cancer-specific immune response.
The discovery that gene expression can be controlled by interfering with messenger RNA (mRNA) has encouraged the development of targeted molecular therapy against various diseases.2 Through base pairing with mRNA, technologically engineered double-stranded RNA can trigger silencing of complementary mRNA sequences. Such ‘interference RNA' or RNAi has the ability to alter gene expression and has revolutionized research efforts in targeted molecular therapy. An example that has entered the clinic is bevasiranib, a vascular endothelial growth factor-targeted small inhibitory RNA (siRNA), currently in phase III trials of macular degeneration. Despite its therapeutic potential, however, a number of issues need to be addressed. For instance, genome-wide monitoring in microarray experiments has clearly demonstrated that siRNA-treated cells have off-target silencing of a large number of genes.3 In addition, some synthetic siRNAs contain sequence motifs which can trigger unwanted inflammatory responses.4
Seeking to overcome some of these shortcomings, Venkataraman et al.5 formulated a method of therapeutic regulation that is conditional, using small conditional RNAs (scRNAs) that activate protein kinase R-induced apoptosis only upon detection of a targeted cancer mutation.6 The authors designed three transducers of a hybridization chain reaction, each consisting of two scRNAs, which recognize mRNA sequences in three specific human cancer cell lines: the endothelial growth factor receptor commonly found in glioblastoma, EWS/FLI1 in Ewing Sarcoma and the TPC/HPR fusion located on t(6;16)(q22;q12) in prostate carcinoma. Within the cancer cell, hybridization of the targeted cancer marker induces a chain reaction resulting in the activation of a protein kinase R-induced immune response and cell death. Selectivity for the cancer cells was high, with a 20- to 100-fold reduction in the population of malignant cells. In addition, the investigators confirmed the proposed mechanism of action via a series of experiments. For instance, incubation of the target transducer and a control cancer cell line that produced wild-type transcript did not result in cancer cell population reduction, confirming selectivity for mutant transcript-triggered cell death. The authors concluded that unlike conventional RNAi, scRNA performs mechanical transduction, functionally decouples diagnosis and treatment, and is conditional.
Despite possible advantages regarding this approach, the proposed scRNA faces several challenges as investigators attempt to bring this technology to clinical treatment of cancer. First, despite enhancing selectivity by decoupling diagnosis and treatment, scRNAs (like siRNAs) may cause off-target effects and induce pro-inflammatory responses in vivo.6 Second, introducing ectopic scRNAs into cells may disrupt the intrinsic cellular machinery. Grimm et al. observed such an effect when mice receiving targeted siRNAs died from liver damage associated with reduced expression of liver specific micro-RNAs.7 Third, given the variability of genetic abnormalities observed in solid tumors, targeting a single RNA sequence to induce apoptosis may not be ideal. For instance, expression of t(6;16)(q22;q12) in metastatic prostate adenocarcinoma is limited to a subset of cancers and thus may benefit only a small group of patients. Thus, tumor genotyping to program patient-specific scRNAs may be needed for this method to be effective. Fourth, effective in vitro delivery remains a significant obstacle.8 Due to its negative charge, target scRNAs cannot cross into cells without further manipulation. Even while several approaches had been shown to be effective, therapeutic dosage delivery will have to be carefully tailored.
This study highlights the potential of RNA therapeutics, leading to conditional activation of transducers and consequently cancer cell apoptosis. Using modern RNA technology, the authors successfully generated a potential therapeutic approach that targets only malignant cells while not affecting normal cells. While further studies in animal models are needed, the goal of targeted molecular therapy in the treatment of cancer may move a step forward with such RNA-based therapies.
01 Jan 2010·Ophthalmology and eye diseases
Bevasiranib for the Treatment of Wet, Age-Related Macular Degeneration
Article
Author: Mousa, Shaker A. ; Garba, Adinoyi O.
Age- related Macular Degeneration (AMD) is the leading cause of severe visual impairment in people 65 years and older in industrialized nations. Exudative, or “wet”, AMD is a late form of AMD (as distinguished from atrophic, so-called dry, AMD) and is responsible for over 60% of all cases of blindness due to AMD. It is widely accepted that vascular endothelial growth factor (VEGF) is a key component in the pathogenesis of choroidal neo-vascularization (CNV), which is a precursor to wet AMD. The current gold-standard for treating wet AMD is the monoclonal antibody fragment ranibizumab (trade name Lucentis), which targets VEGF. Other agents used to treat wet AMD include pegaptanib (Macugen), bevacizumab (Avastin; off-label use), and several other experimental agents. The advent of small interfering RNA (siRNA) has presented a whole new approach to inhibiting VEGF. This article reviews the status of a novel siRNA-based therapeutic, bevasiranib, for the treatment of wet AMD. Bevasiranib is believed to work by down regulating VEGF production in the retina. Studies in human cell-lines and animal models have shown that VEGF siRNAs are effective in inhibiting VEGF production. Although there is a lack of sufficient published data on human studies supporting the use of bevasiranib for wet AMD, available data indicates that due to its unique mechanism of action, bevasiranib might hold some promise as a primary or adjunct treatment for wet AMD.
01 Jun 2009·Retina (Philadelphia, Pa.)Q2 · MEDICINE
COMBINATION THERAPY USING THE SMALL INTERFERING RNA BEVASIRANIB
Q2 · MEDICINE
Article
Author: LAWRENCE SINGERMAN
Bevasiranib, the first small interfering RNA agent developed for the treatment of neovascular age-related macular degeneration, has demonstrated clinical promise. Injected intravitreally, this small interfering RNA acts by inducing catalytic destruction of messenger RNA to silence gene expression. Bevasiranib targets the production of vascular endothelial growth factor (VEGF) protein. It does not affect existing VEGF protein, suggesting that it may offer a synergistic effect when given in combination with anti-VEGF treatments, such as ranibizumab. The safety of bevasiranib has been supported by preclinical and clinical research.
1
News (Medical) associated with Bevasiranib07 Jul 2023
At the beginning of the year, GSK announced its decision to discontinue investments in the field of cell and gene therapies and shift its focus to small nucleic acid drugs. This news immediately brought small nucleic acid drugs into the spotlight, capturing people's attention and enthusiasm.
In fact, in December 2022, GSK entered into a partnership with nucleic acid therapeutics company Wave Life Sciences, with GSK providing a total investment of $3.3 billion to support the development of small nucleic acid drugs. This collaboration allows GSK to advance at least eight projects in this field. So, what are small nucleic acid drugs, and why are they highly valued by industry giants?
Small Nucleic Acid Drugs: A Battleground in the Pharmaceutical IndustrySmall nucleic acid drugs, also known as oligonucleotide drugs, generally refer to nucleotide sequences of up to 30 base pairs. Their mechanism of action involves specific nucleotide sequences targeting mRNA to silence gene expression of target proteins, thereby achieving therapeutic effects. In a narrow sense, small nucleic acid drugs refer to RNA interference drugs (siRNA), while in a broader sense, they also include antisense oligonucleotides (ASO), microRNAs (miRNA), small activating RNAs (saRNA), mRNA, RNA aptamers, and others. Currently, small nucleic acid drugs mainly consist of siRNA and ASO.
Due to their ability to target specific proteins at the post-transcriptional level, small nucleic acid drugs offer the potential to develop therapeutic drugs for "undruggable" diseases, making them of significant clinical importance.
Furthermore, as small nucleic acid drugs directly regulate protein expression at the upstream level, they overcome the issue of drug resistance associated with targeted protein drugs. They also possess the potential to cure diseases and achieve long-term therapeutic effects.
In contrast to traditional small molecules and antibody drugs that require recognition of protein conformation, small nucleic acid drugs only need to target disease-causing gene sequences and design corresponding RNA fragments. This advantage results in shorter development cycles and faster drug target screening. Moreover, small nucleic acid drugs have well-defined mechanisms of action and do not rely on complex protein structures, leading to a higher success rate in development.
According to a recent report published by research firm Research And Markets, the global market for small nucleic acid drugs reached $6.1 billion in 2022 and is projected to reach $19.9 billion by 2030, with a compound annual growth rate of 15.9%.
Given the numerous advantages of small nucleic acid drugs and the vast market potential, industry insiders predict that they will become a battleground in the global pharmaceutical industry.
Breaking Free from the Shackles of Rare Diseases: 14 Small Nucleic Acid Drugs Currently on the MarketSince the establishment of Ionis, an antisense oligonucleotide development company, in 1987, small nucleic acid drugs have undergone more than 30 years of development. However, the road to developing small nucleic acid drugs has not always been smooth. Issues such as instability, immunogenicity, low cellular uptake efficiency, endosomal escape challenges, and significant side effects have previously hindered the progress of small nucleic acid drugs.
In 2009, OPKO, a pharmaceutical company in Miami, terminated Phase III clinical trials of the siRNA drug bevasiranib for the treatment of wet age-related macular degeneration due to its lack of efficacy. Additionally, many companies focused on small nucleic acid drugs withdrew from the field due to challenges in drug delivery and off-target toxicity.
In 2010, Roche announced its withdrawal from the RNA interference (RNAi) field after investing $500 million. In 2011, Pfizer terminated its RNAi program, and the same year, Merck shut down its RNAi research center. Meanwhile, Novartis announced the termination of its collaboration with RNAi development company Alnylam. The successive exit of major pharmaceutical companies led to a downturn in small nucleic acid drug development. However, some companies continued to persevere.
With breakthroughs in key technologies such as chemical modifications and delivery systems, small nucleic acid drugs have entered a new phase of development. As of now, there are 14 small nucleic acid drugs approved and on the market worldwide, including 9 antisense oligonucleotides (ASOs), 4 siRNA drugs, and 1 nucleic acid aptamer. Approximately 80% of these drugs were approved after 2015, and their therapeutic applications primarily focus on rare diseases.
Entering the Field of Chronic Diseases: Small Nucleic Acid Drugs Reach New HeightsDue to the long-lasting effects and resistance avoidance of small nucleic acid drugs, the industry is gradually recognizing their value in the field of chronic diseases.
In the cardiovascular disease field, Alnylam and Novartis' Inclisiran, a siRNA drug targeting PCSK9, received FDA approval in December 2021 for the treatment of atherosclerotic cardiovascular disease. PCSK9 is an important target involved in regulating low-density lipoprotein cholesterol (LDL-C).
Clinical trials have shown that subcutaneous injections of Inclisiran every six months significantly reduce LDL-C levels. Compared to placebo, Inclisiran achieves a 48%-52% reduction in LDL-C, demonstrating a sustained and significant therapeutic effect. Furthermore, Inclisiran is well-tolerated. With its low injection frequency and high patient compliance, Inclisiran is considered a promising siRNA drug, with projected annual sales expected to exceed $3 billion, according to Evaluate Pharma.
Another major area of interest for small nucleic acid drugs in the field of chronic diseases is functional cure for hepatitis B. Functional cure refers to the sustained absence of HBsAg (hepatitis B surface antigen) and HBV DNA (hepatitis B virus DNA), as well as seroconversion of HBeAg (hepatitis B virus e antigen), with or without HBsAg seroconversion.
This results in improved liver inflammation and histopathological changes, as well as reduced incidence of end-stage liver diseases, including liver cancer. HBsAg clearance serves as a key indicator for functional cure in hepatitis B.
In terms of functional cure for hepatitis B, the most rapidly progressing development globally is the collaboration between GSK and Ionis for Bepirovirsen, an ASO drug that inhibits hepatitis B virus protein synthesis through RNA interference. The binding site of bepirovirsen exists in all hepatitis B virus mRNAs and pregenomic RNAs, thereby inhibiting the RNA, DNA, and protein expression of all hepatitis B viruses.
Bepirovirsen is currently in Phase III clinical trials, and preliminary results have shown that it can inhibit HBsAg protein expression while stimulating immune responses through Toll-like receptor 8 (TLR8), activating the immune system to clear the virus from the bloodstream.
Another fast-progressing drug is VIR-2218, jointly developed by Vir and Alnylam, which is an RNAi therapy targeting hepatitis B virus. Results from Phase I/II clinical trials demonstrate that VIR-2218 can dose-dependently reduce patients' HBsAg levels, with a reduction exceeding 1 log10 (10-fold) in HBsAg levels for 71% of patients.
Currently, reducing HBsAg remains a major challenge in hepatitis B treatment. If small nucleic acid drugs can prove their long-lasting efficacy and achieve functional cure in subsequent studies, it will be a significant breakthrough in hepatitis B treatment.
References
1.https://www.fiercebiotech.com/biotech/no-regrets-gsk-turning-its-back-cell-therapies-oligio-strategy-heats;
2. Jennifer Hardy,Stephanie Niman, Edward Pereira, et al. A Critical Review of the Efficacy and Safety of Inclisiran. Am J Cardiovasc Drugs. 2021; 21(6): 629-642.
3.Nabil G Seidah, et al. PCSK9: a key modulator of cardiovascular health. Circ Res. 2014 Mar 14;114(6):1022-36.
4.Meier MA, Calabrese D, Suslov A, Terracciano LM, Heim MH, Wieland S. Ubiquitous expression of HBsAg from integrated HBV DNA in patients with low viral load. J Hepatol. 2021;S0168-8278(21)00328-7.
5.https://www.gsk.com/en-gb/media/press-releases/gsk-presents-promising-new-data-for-bepirovirsen-an-investigational-treatment-for-chronic-hepatitis-b/.
100 Deals associated with Bevasiranib
Login to view more data
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| - | Bevasiranib | - |
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Choroidal Neovascularization | Phase 3 | Portugal | 25 Sep 2007 | |
| Wet age-related macular degeneration | Phase 3 | United States | 01 Aug 2007 | |
| Wet age-related macular degeneration | Phase 3 | Canada | 01 Aug 2007 | |
| Wet Macular Degeneration | Phase 3 | United States | 01 Aug 2007 | |
| Wet Macular Degeneration | Phase 3 | Canada | 01 Aug 2007 | |
| Diabetic macular oedema | Phase 2 | United States | 01 Jan 2006 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
Phase 3 | 338 | (Bevasiranib 8 Weeks) | hsfllnjtay(okuwrdwmza) = klztuwremt ogfxmqqroy (hyjajjsnbw, rhpawimwef - huxhdsbfbn) View more | - | 06 Oct 2014 | ||
(Bevasiranib 12 Weeks) | hsfllnjtay(okuwrdwmza) = mfrhclbtyd ogfxmqqroy (hyjajjsnbw, wujfyhhgsj - fwvnimwbde) View more |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or

Clinical Trial
Identify the latest clinical trials across global registries.
login
or

Approval
Accelerate your research with the latest regulatory approval information.
login
or

Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

