In the wide world of traditionally undruggable proteins, one group stands out as the trickiest to catch. These squiggly molecules seem to have no stable structure, and their squirminess makes capturing a proper molecular picture of them, let alone grabbing hold of them with a drug, close to impossible.
That was until
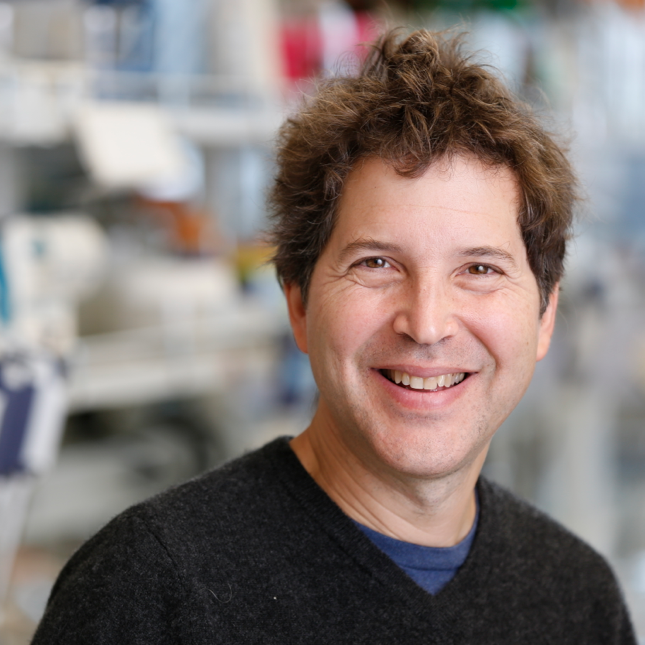
David Baker
set his sights on them. “I think we’ve kind of solved that problem,” he told
Endpoints News
.
Baker, who
won the Nobel Prize in Chemistry
last year for his work designing proteins with computers and artificial intelligence, has revealed two new strategies that use AI to develop artificial proteins that bind to the so-called intrinsically disordered proteins (IDPs) or similarly slippery segments called intrinsically disordered regions (IDRs).
“They’re interesting drug targets” involved in numerous biological processes and diseases, Baker said. But computational methods that “dock” small molecules into rigid protein structures don’t work for the wobbly IDPs, and the unstructured proteins often aggregate or degrade when injected into an animal, making antibody drug development a pain as well. “They’ve just been essentially undruggable,” Baker added.
His new methods, one of which was published Thursday in
Science
and the other as a preprint on
bioRxiv
, give biologists new tools for manipulating and studying the famously wily proteins. Baker’s lab used the approaches to develop binders against proteins involved in cancer, diabetes, pain and more.
Although the new protein binders are not ready for prime-time drug development, Baker is no novice when it comes to spinning research into a biotech company. He has played a founding role in
more than 20 companies
, including
Xaira Therapeutics
, which
launched with $1 billion last year
to develop protein therapies based on generative AI technologies invented in his lab at the University of Washington.
Baker said Xaira remains focused on using AI to make antibody drugs, and the new work developing binders for IDPs could become the basis of a new company. “We’re definitely thinking about that,” he said, adding that he is brainstorming the best drug targets for the potential company to focus on.
Baker’s lab came up with two ways to develop artificial proteins that would bind to IDPs and IDRs. The method revealed in the preprint, which is currently under peer review, is a new application of Baker’s generative AI software called RFdiffusion that first debuted in
late 2022
and helped
kick off the modern era of AI-driven protein design
.
RFdiffusion is analogous to AI image generators, but instead of asking the computer to make a picture, scientists ask it to create the structure of a three-dimensional protein. If the structure of one protein is known, they can ask the AI to create another protein that binds to it. “The problem with using that for an unstructured protein is that there is no structure to provide,” Baker said.
In lieu of a structure, the researchers simply input the amino acid sequence of the disordered protein. The AI model then runs through possible shapes for both the IDP and the binder simultaneously. “The structure of the binder is kind of moving around to hold on to the target, and the target itself is fluctuating, sampling different states,” Baker said. “So there is kind of like a dance together.”
The lab used the approach to create binders to multiple IDPs, including a protein called amylin that aggregates into fibrils in type 2 diabetes. The binder broke up amylin fibrils in a lab dish.
This method of having the binder and disordered protein “dance” until they match up doesn’t work well for all IDPs, Baker said. That’s because the AI sometimes pushes the disordered protein to fold up into protein structures called alpha helices and beta sheets, giving the binder something more concrete to grasp. But some of the disordered proteins, as their name implies, can’t be coaxed to fold into these structures.
To deal with the unruliest IDPs, the researchers formed a library of 1,000 pre-made binders with pockets that would recognize just a tiny stretch of amino acids. By stringing together these protein pockets, Baker’s lab was able to make strong binders to 39 of the 43 disordered proteins it tested the method against. One of those proteins, called dynorphin, is involved in pain. When the dynorphin binder was added to human cells growing in a dish, it blocked pain signaling.
In a separate study posted on
bioRxiv
as a preprint, Baker’s lab used the method to design binders against the specific mutant forms of the infamous Ras proteins (including two versions of KRAS) that are widely implicated in cancer. Baker said his lab is also using the new methods to design binders against another famously undruggable cancer protein called MYC.
“We can robustly make designs for many different targets,” Baker said. “It’s gone from being not possible to solve to actually almost easier than the folded protein problem.”