Request Demo
Last update 08 May 2025
MTX-101 (Mozart Therapeutics)
Last update 08 May 2025
Overview
Basic Info
Drug Type Bispecific antibody |
Synonyms KIR independent CD8 Treg Modulator (Mozart Therapeutics) + [3] |
Target |
Action stimulants, inhibitors |
Mechanism CD8 stimulants(Cluster of differentiation 8 stimulants), KIR inhibitors(Killer cell immunoglobulin like receptors inhibitors) |
Active Indication |
Inactive Indication- |
Originator Organization |
Active Organization |
Inactive Organization- |
License Organization- |
Drug Highest PhasePhase 1 |
First Approval Date- |
Regulation- |
Login to view timeline
Related
1
Clinical Trials associated with MTX-101 (Mozart Therapeutics)NCT06324604
Safety, Pharmacokinetics, and Pharmacodynamics of MTX-101 in Healthy Adults and Patients
First in human study to understand the potential side effects of MTX-101, how long MTX-101 lasts in the human body, and how MTX-101 affects specific human immune cells.
Start Date13 Jun 2024 |
Sponsor / Collaborator |
100 Clinical Results associated with MTX-101 (Mozart Therapeutics)
Login to view more data
100 Translational Medicine associated with MTX-101 (Mozart Therapeutics)
Login to view more data
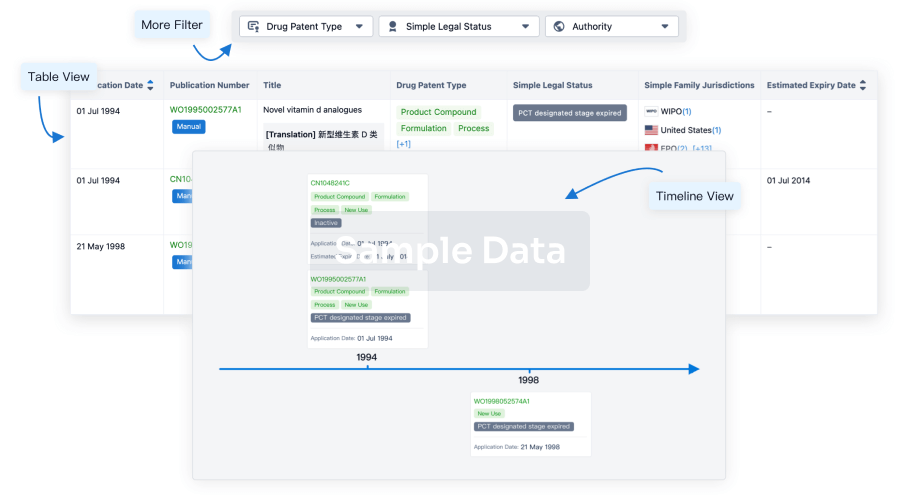
100 Patents (Medical) associated with MTX-101 (Mozart Therapeutics)
Login to view more data
1
Literatures (Medical) associated with MTX-101 (Mozart Therapeutics)Frontiers in Immunology
Preclinical characterization of MTX-101: a novel bispecific CD8 Treg modulator that restores CD8 Treg functions to suppress pathogenic T cells in autoimmune diseases
Article
Author: Therriault, Jon H. ; Swiderek, Kristine M. ; Pham, Minh N. ; Morgan, Nadine N. ; Gilbertson, Emily A. ; Gardell, Jennifer L ; Childs, Monica M. ; Chen, Alex ; Pham, Minh N ; Gardell, Jennifer L. ; McMahan, Catherine J ; McMahan, Catherine J. ; Crane, Courtney A ; Boster, Daniel R ; Patton, Daniel T ; Encarnacion, Kaelen ; Meengs, Brent ; Bowser, Justin ; Maurer, Meghan E. ; Boster, Daniel R. ; Therriault, Jon H ; Quach, Phoenicia ; Patton, Daniel T. ; Tan, Cong ; Morgan, Nadine N ; Maurer, Meghan E ; Bogatzki, Lisa ; Childs, Monica M ; Julien, Susan H ; Crane, Courtney A. ; Julien, Susan H. ; Gilbertson, Emily A ; Hermansky, Gleda ; Swiderek, Kristine M
11
News (Medical) associated with MTX-101 (Mozart Therapeutics)17 Mar 2025
Enrollment of Patients with Autoimmune Disease in Phase 1b Study has Begun
SEATTLE, March 17, 2025 /PRNewswire/ -- Mozart Therapeutics, the leading developer of CD8 Treg modulators for the treatment of autoimmune disease, today announce the successful completion of their Phase 1a study of MTX-101 in healthy adults. The randomized, blinded, placebo-controlled study evaluated MTX-101—a first-in-class autoimmune checkpoint inhibitor—as single and multiple doses in an ascending-dose design (NCT06324604).
Data from the study in healthy adults show MTX-101 is well tolerated. Most adverse events were low-grade and there were no serious adverse events. Participants receiving MTX-101 experienced transient and self-limited decreases in lymphocytes, which the Company believes are consistent with the study drug's mechanism of action and indicative of target engagement.
Data further demonstrate that MTX-101 has predictable, dose-dependent pharmacokinetics (PK) and receptor occupancy that are expected to enable a convenient and competitive dosing regimen. Pharmacodynamic data support proof of mechanism and show that MTX-101 is highly selective for regulatory CD8 T cells, and that engagement with MTX-101 results in CD8 Treg activation.
Mozart plans to present full data from the Phase 1a study at upcoming medical symposia.
"We are thrilled that the initial MTX-101 Phase 1 data in healthy adults confirm the mechanistic and safety findings from our pre- and nonclinical studies. This represents not only an important milestone for Mozart, but also a significant achievement as we work to advance a class of CD8 Treg modulators to restore durable immune homeostasis in autoimmune disease," said Katie Fanning, President and Chief Executive Officer of Mozart Therapeutics.
"Our observations from the healthy adults hold great promise for patients with autoimmune disease," echoed Jason Chien, M.D., M.S., Mozart's Chief Medical Officer. "The well-tolerated safety profile, antibody-like PK, and clear evidence of target engagement and activation represent an exciting novel class of therapeutics that has the potential to deliver substantial clinical benefit. With these data, we are quickly advancing MTX-101 in patients with type 1 diabetes and celiac disease."
The first patients with type 1 diabetes and celiac disease have been enrolled in Part B of the study, which is being conducted at multiple clinical sites in Australia. "MTX–101 has a novel mechanism of action that has great potential to improve the lives of people living with autoimmune disease," said Professor John Wentworth, M.D.; Endocrinologist, The Royal Melbourne Hospital Department of Medicine; Senior Clinical Research Fellow, St Vincent's Institute of Medical Research; Director, ANZ Type 1 Diabetes TrialNet. "This is why our type 1 diabetes community is so excited to participate in the MTX-101 development program and help determine its ability to decrease dependance on insulin injections."
About MTX-101
MTX-101 is an antigen-agnostic bispecific antibody targeting inhibitory KIR and CD8 expressed on regulatory CD8 T cells. This autoimmune checkpoint inhibitor aims to restore the intrinsic functions of CD8 Treg, acting early in the autoimmune disease process to suppress and eliminate pathogenic T cells, halt downstream inflammation, and prevent tissue destruction.
About Mozart Therapeutics
Mozart Therapeutics is focused on developing first-in-class disease-modifying therapies for autoimmune diseases, utilizing a novel approach to restoring immune system function by targeting the CD8 T regulatory network. The company is headquartered in Seattle, WA. For more information, visit and follow the company on LinkedIn @Mozart–tx.com.
SOURCE Mozart Therapeutics
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
Phase 1Clinical Result
19 Nov 2024
The growing comprehension of the pathogenesis of celiac disease has paved the way for the exploration of alternative treatment strategies. These novel approaches are aimed at addressing the condition at its root cause, targeting the underlying mechanisms that trigger the immune response in individuals with celiac disease. These innovative approaches hold the promise of transforming the landscape of celiac disease treatment in the near future.
LAS VEGAS, Nov. 19, 2024 /PRNewswire/ -- DelveInsight's
'
Celiac Disease Pipeline Insight 2024
' report provides comprehensive global coverage of pipeline celiac disease therapies in various stages of clinical development, major pharmaceutical companies are working to advance the pipeline space and future growth potential of the celiac disease pipeline domain.
Key Takeaways from the Celiac Disease Pipeline Report
DelveInsight's celiac disease pipeline report depicts a robust space with
25+ active players working to develop
30+ pipeline therapies for celiac disease treatment.
Key celiac disease companies such as
Takeda, Sanofi, Entero Therapeutics, Pfizer, Topas Therapeutics, Anokion SA, Protagonist Therapeutics, Equillium, Theriva Biologics, Chugai Pharmaceutical, Novartis, Immunic, Mozart Therapeutics, Nemysis Ltd, Barinthus Biotherapeutics, Parvus Therapeutics, Kallyope, AMYRA Biotech AG, Forte Biosciences, LAPIX Therapeutics, Ahead Therapeutics, Allero Therapeutics, STEMCELL Technologies, IM Therapeutics, Provid Pharmaceuticals, Sigmoid Pharma, Janssen Biotech, Inc., Lumen Bioscience, IGY Life Sciences, Ahead Therapeutics, ANTOLRX, Imcyse, and others are evaluating new celiac disease drugs to improve the treatment landscape.
Promising Celiac Disease pipeline therapies such as
TAK-101, TAK-062, PRV-015, Latiglutenase, TAK-227, Ritlecitinib, TPM-502, KAN 101, PTG-100, EQ 102, SYN-020, DONQ52, CALY-002, IMU-856, MTX-101, E 40-02, VTP-1000, PVT-301, Research Program: Celiac disease, AMY02, FB 102, LPX-TIGI, AT 1718, ALL-001, SQZ TACs, Research Program: small molecule therapeutics, Research Program: DQ2/8, Research Program: SmPillformulations, Research Program: autoimmune disease therapeutics, IgY-112, AT 1715, Research programme: Celiac disease, and others are under different phases of Celiac Disease clinical trials.
In October 2024, Topas Therapeutics announced positive topline results from its Phase IIa trial of TPM502, in patients with celiac disease. The study data serves as the first clinical proof of concept for Topas' proprietary nanoparticle platform and its potential to induce targeted, antigen-specific tolerogenic effects.
In September 2024, Barinthus Biotherapeutics plc, a clinical-stage biopharmaceutical company developing novel immunotherapeutic candidates that guide T cells to control disease, announced the initiation of its first-in-human Phase I trial of VTP-1000 in adults with coeliac disease.
In May 2024, Entero Therapeutics, Inc. (formerly First Wave BioPharma, Inc.) unveiled its new corporate name and website. The rebranding follows the recent business combination with ImmunogenX and reflects the Company's focus on addressing unmet needs in GI health that include celiac disease, an indication for which there are no approved medicines today.
In March 2024, First Wave BioPharma announced the acquisition of ImmunogenX in an all-stock transaction with the combined company focused on advancing a GI pipeline comprised of multiple, late-stage clinical assets, including latiglutenase, a potentially first-in-class, near Phase III-ready, targeted, oral biotherapeutic for celiac disease.
In February 2024, with the approval of the SQZ transaction, STEMCELL acquired substantially all of SQZ's assets including its entire portfolio of over 400 patents and trademarks, other intellectual property such as copyrights and trade secrets, proprietary equipment, and its head license with the Massachusetts Institute of Technology.
In January 2024, Calypso Biotech BV announced that it had entered into an agreement to be acquired by Novartis AG ('Novartis'). Calypso's shareholders received an upfront payment of $250 million upon closing and are eligible to receive development milestones of up to $175 million based on the achievement of certain predetermined milestones. The acquisition gives Novartis full rights to CALY-002. Novartis intends to further explore CALY-002 across a wide variety of autoimmune indications with high unmet medical needs.
Request a sample and discover the recent advances in celiac disease treatment drugs @
Celiac Disease Pipeline Report
The celiac disease pipeline report provides detailed profiles of pipeline assets, a comparative analysis of clinical and non-clinical stage celiac disease drugs, inactive and dormant assets, a comprehensive assessment of driving and restraining factors, and an assessment of opportunities and risks in the celiac disease clinical trial landscape.
Celiac Disease Overview
Celiac disease is a chronic autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. In individuals with celiac disease, the immune system mistakenly attacks the small intestine upon gluten consumption, leading to inflammation and damage to the intestinal lining, specifically the villi, which are essential for nutrient absorption. The exact cause of celiac disease is not fully understood, but it is known to involve a combination of genetic predisposition (usually associated with HLA-DQ2 or HLA-DQ8 genes) and environmental factors.
Common symptoms of celiac disease include digestive issues such as diarrhea, bloating, gas, constipation, and abdominal pain. However, some individuals experience non-digestive symptoms, like fatigue, anemia, joint pain, skin rashes, and even neurological issues such as headaches or depression. Because of this broad symptom range, celiac disease is often underdiagnosed or misdiagnosed as other conditions.
Diagnosis typically involves blood tests to detect specific antibodies (like tissue transglutaminase antibodies) and, if positive, is followed by an intestinal biopsy to confirm damage to the villi. Genetic testing may also be conducted in some cases to identify predispositions.
The primary treatment for celiac disease is a strict, lifelong gluten-free diet. By avoiding gluten, individuals with celiac disease can heal intestinal damage and prevent symptoms and complications. However, adherence to this diet requires vigilance, as even small amounts of gluten can trigger symptoms and damage.
Find out more about celiac disease treatment drugs @
Drugs for
Celiac Disease Treatment
A snapshot of the Celiac Disease Pipeline Drugs mentioned in the report:
Learn more about the emerging celiac disease pipeline therapies @
Celiac Disease Clinical Trials
Celiac Disease Therapeutics Assessment
The celiac disease pipeline report proffers an integral view of the celiac disease emerging novel therapies segmented by stage, product type, molecule type, mechanism of action, and route of administration.
Scope of the Celiac Disease Pipeline Report
Coverage: Global
Therapeutic Assessment By Product Type: Mono, Combination, Mono/Combination
Therapeutic Assessment By Clinical Stages: Discovery, Pre-clinical, Phase I, Phase II, Phase III
Therapeutics Assessment
By Route of Administration: Oral, Intravenous, Subcutaneous, Parenteral, Topical
Therapeutics Assessment
By Molecule Type: Recombinant fusion proteins, Small molecule, Monoclonal antibody, Peptide, Polymer, Gene therapy
Therapeutics Assessment
By Mechanism of Action: Gliadin inhibitors, Gluten modulators, Transglutaminase 2 inhibitors, Emt protein-tyrosine kinase inhibitors, Janus kinase 3 inhibitors, Alpha4beta7 integrin antagonists, Interleukin 15 inhibitors, Interleukin 21 inhibitors, Alkaline phosphatase replacements, HLA-DQ antigen inhibitors
Key Celiac Disease Companies: Takeda, Sanofi, Entero Therapeutics, Pfizer, Topas Therapeutics, Anokion SA, Protagonist Therapeutics, Equillium, Theriva Biologics, Chugai Pharmaceutical, Novartis, Immunic, Mozart Therapeutics, Nemysis Ltd, Barinthus Biotherapeutics, Parvus Therapeutics, Kallyope, AMYRA Biotech AG, Forte Biosciences, LAPIX Therapeutics, Ahead Therapeutics, Allero Therapeutics, STEMCELL Technologies, IM Therapeutics, Provid Pharmaceuticals, Sigmoid Pharma, Janssen Biotech, Inc., Lumen Bioscience, IGY Life Sciences, Ahead Therapeutics, ANTOLRX, Imcyse, and others.
Key Celiac Disease Pipeline Therapies: TAK-101, TAK-062, PRV-015, Latiglutenase, TAK-227, Ritlecitinib, TPM-502, KAN 101, PTG-100, EQ 102, SYN-020, DONQ52, CALY-002, IMU-856, MTX-101, E 40-02, VTP-1000, PVT-301, Research Program: Celiac disease, AMY02, FB 102, LPX-TIGI, AT 1718, ALL-001, SQZ TACs, Research Program: small molecule therapeutics, Research Program: DQ2/8, Research Program: SmPillformulations, Research Program: autoimmune disease therapeutics, IgY-112, AT 1715, Research programme: Celiac disease, and others.
Dive deep into rich insights for new drugs for celiac disease treatment, visit @
Celiac Disease Drugs
Table of Contents
For further information on the celiac disease pipeline therapeutics, reach out @
Celiac Disease Treatment Drugs
Related Reports
Celiac Disease Epidemiology
Celiac Disease Epidemiology Forecast – 2032 report delivers an in-depth understanding of the disease, historical and forecasted celiac disease epidemiology in the 7MM, i.e., the United States, EU5 (Germany, Spain, Italy, France, and the United Kingdom), and Japan.
Celiac Disease Market
Celiac Disease Market Insights, Epidemiology, and Market Forecast – 2034 report deliver an in-depth understanding of the disease, historical and forecasted epidemiology, market share of the individual therapies, and key celiac disease companies including
Entero Therapeutics, Amgen, Provention Bio, Takeda, among others.
Sjogren's Syndrome Market
Sjogren's Syndrome Market Insights, Epidemiology, and Market Forecast – 2034 report delivers an in-depth understanding of the disease, historical and forecasted epidemiology, as well as the market trends, market drivers, market barriers, and key Sjogren's syndrome companies including
Horizon Therapeutics (Amgen), Dompe Farmaceutici, Sylentis, MorphoSys, Resolve Therapeutics, OSE Immunotherapeutics, Servier, Novartis, Johnson & Johnson
, among others.
Sjogren's Syndrome Pipeline
Sjogren's Syndrome Pipeline Insight – 2024 report provides comprehensive insights about the pipeline landscape, pipeline drug profiles, including clinical and non-clinical stage products, and the key Sjogren's syndrome companies, including
Novartis, Horizon Therapeutics, Bristol-Myers Squibb, Rise Therapeutics, Resolve Therapeutics, Dompe Farmaceutici, among others.
About DelveInsight
DelveInsight is a leading Business Consultant and Market Research firm focused exclusively on life sciences. It supports pharma companies by providing comprehensive end-to-end solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve
.
Contact Us
Shruti Thakur
[email protected]
+14699457679
Logo:
SOURCE DelveInsight Business Research, LLP
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED

Clinical ResultPhase 2AcquisitionPhase 1Immunotherapy
07 Nov 2024
Preclinical Data Show MTX-101 Selectively Binds CD8 Treg, Restores Elimination of Autoreactive Cells, and Confirms Therapeutic Potential in Multiple Autoimmune Disease Models
Phase 1 Clinical Study Underway to Evaluate MTX-101 in Healthy Adults and Patients with Celiac Disease and Type 1 Diabetes
SEATTLE, Nov. 7, 2024 /PRNewswire/ -- Mozart Therapeutics, a clinical-stage biopharmaceutical company focused on the development of CD8 Treg modulators in autoimmune disease, announce today the publication of its first peer-reviewed publication entitled "Preclinical characterization of MTX-101: a novel bispecific CD8 Treg modulator that restores CD8 Treg functions to suppress pathogenic T cells in autoimmune diseases" in the journal Frontiers in Immunology. The publication extends on seminal work (Saligrama et al, 2019; Li et al, 2022) describing a cytolytic CD8 T cell subset (CD8 Treg) with anti-inflammatory effects that is dysfunctional in autoimmune diseases. The work furthers the understanding of the mechanisms underpinning CD8 Treg dysfunctions, as well as preclinical data for the Company's novel bispecific antibody, MTX-101. The data illustrate that MTX-101 selectively binds to human CD8 Treg, restoring their cytolytic functions, resulting in pathogenic CD4 T cell elimination in the periphery and disease-affected tissues ex vivo. Importantly, data demonstrate that the effects of MTX-101 are not broadly immunosuppressive and do not impair responses to viral and bacterial antigens. The full manuscript is available online (doi: 10.3389/fimmu.2024.1452537).
"The publication of our first manuscript is a significant milestone for Mozart Therapeutics. It highlights the hard work and commitment of our entire team to develop novel therapeutics with disease-modifying potential for patients with autoimmunity, and is in line with our mission to share our work with the scientific community. Collectively, our preclinical data provides a strong rationale for our ongoing clinical development of MTX-101 and confirms its broad therapeutic potential in early stage and/or indolent autoimmune diseases", said Courtney Crane, Ph.D., Senior Vice President of Biology and Translational Medicine at Mozart Therapeutics.
The publication comes at an important time as the Company is evaluating MTX-101 in a Ph1 study in healthy adults and patients with T1D and celiac disease. Mozart Therapeutics remains committed to understanding and correcting CD8 Treg dysfunctions as it advances a pipeline of therapeutic molecules that provide effective and durable solutions to clinicians and patients with autoimmunity.
About MTX-101
MTX-101 is a bispecific antibody targeting inhibitory KIR and CD8 expressed on regulatory CD8 T cells. This autoimmune checkpoint inhibitor aims to restore the intrinsic functions of regulatory CD8 T cells, acting early in the autoimmune disease process to suppress and eliminate pathogenic cells, halt downstream inflammation, and prevent tissue destruction. MTX-101 is currently being evaluated in a randomized, blinded, placebo-controlled Phase 1 trial (NCT06324604) in healthy adults (study Part A; enrollment complete) and in patients with type 1 diabetes mellitus or celiac disease (study Part B). The clinical study is evaluating the safety, pharmacokinetics, and pharmacodynamics of MTX-101; in Part B, disease-specific biomarkers will also be assessed.
About Mozart Therapeutics
Mozart Therapeutics is focused on developing first-in-class disease-modifying therapies for autoimmune diseases, utilizing a novel approach to restoring immune system function by targeting the CD8 T regulatory network. The company is headquartered in Seattle, WA. For more information, visit and follow the company on LinkedIn @Mozart–tx.com.
SOURCE Mozart Therapeutics
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED

Phase 1
100 Deals associated with MTX-101 (Mozart Therapeutics)
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Celiac Disease | Phase 1 | Austria | 13 Jun 2024 | |
| Celiac Disease | Phase 1 | Australia | 13 Jun 2024 | |
| Diabetes Mellitus, Type 1 | Phase 1 | Austria | 13 Jun 2024 | |
| Diabetes Mellitus, Type 1 | Phase 1 | Australia | 13 Jun 2024 | |
| Autoimmune Diseases | Preclinical | United States | 14 Jun 2024 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or

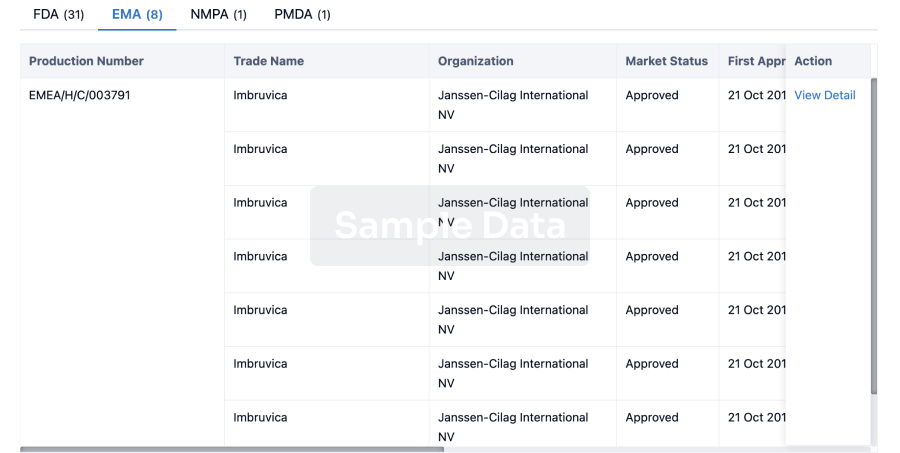
Approval
Accelerate your research with the latest regulatory approval information.
login
or
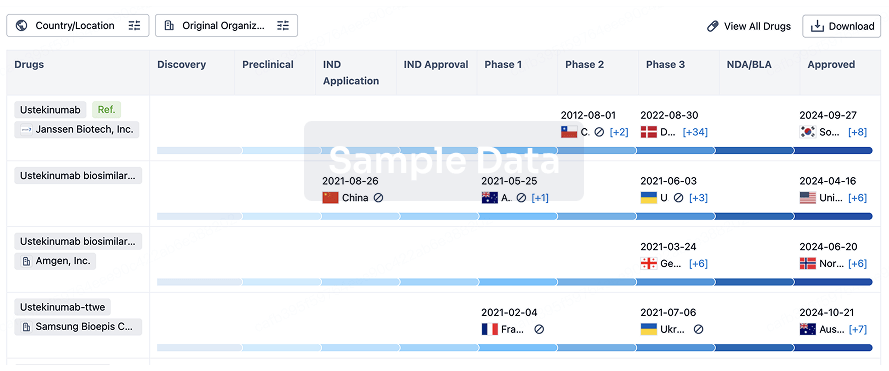
Biosimilar
Competitive landscape of biosimilars in different countries/locations. Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3.
login
or
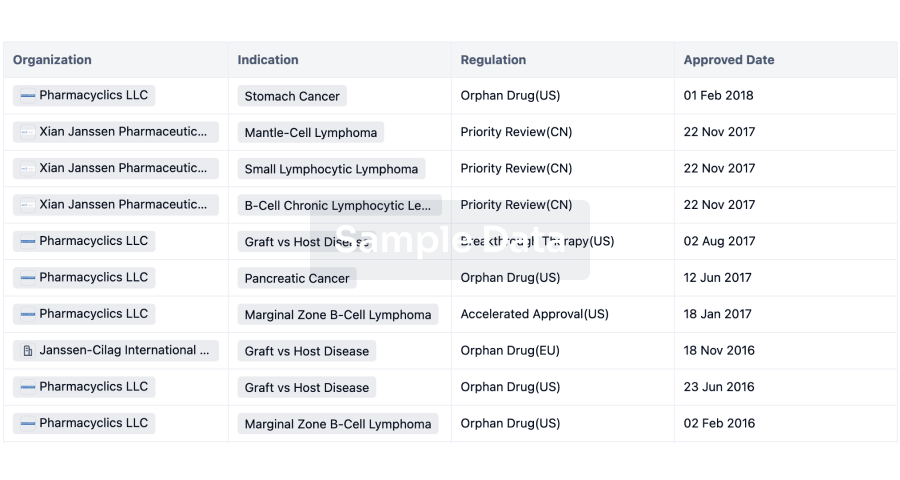
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
