Request Demo
Last update 25 Oct 2025
Orludodstat
Last update 25 Oct 2025
Overview
Basic Info
Drug Type Small molecule drug |
Synonyms BAY 2402234 |
Target |
Action inhibitors |
Mechanism DHODH inhibitors(Dihydroorotate dehydrogenase inhibitors) |
Therapeutic Areas |
Active Indication- |
Inactive Indication |
Originator Organization |
Active Organization- |
Inactive Organization |
License Organization- |
Drug Highest PhaseDiscontinuedPhase 1 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Molecular FormulaC21H18ClF5N4O4 |
InChIKeyKNVJMHHAXCPZHF-JTQLQIEISA-N |
CAS Registry2225819-06-5 |
Related
2
Clinical Trials associated with OrludodstatNCT05061251
An Open-Label Surgical Window of Opportunity Study Evaluating Pharmacodynamic Response of Orally Administered BAY 2402234 in Subjects With Recurrent Glioma, IDH Mutant, Grade 3 or 4
This study aims to look at how BAY 2402234 responds in body in patients with recurrent glioma.
Start Date01 Dec 2021 |
Sponsor / Collaborator |
NCT03404726
An Open-label, Multicenter Phase 1 Study to Characterize the Safety, Tolerability, Preliminary Antileukemic Activity, Pharmacokinetics, and Maximum Tolerated Dose or Pharmacological Active Dose of BAY2402234 in Patients With Advanced Myeloid Malignancies
The primary objective is to determine the safety, tolerability, pharmacokinetics, maximum tolerated dose (MTD), or pharmacological active dose (PAD) of BAY2402234 in patients with acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), or chronic myelomonocytic leukemia (CMML).
The secondary objective is to evaluate evidence of clinical efficacy associated with BAY2402234 in patients with AML (defined as Complete remission, Complete remission with partial hematologic recovery), and MDS (defined as hematological improvement).
The secondary objective is to evaluate evidence of clinical efficacy associated with BAY2402234 in patients with AML (defined as Complete remission, Complete remission with partial hematologic recovery), and MDS (defined as hematological improvement).
Start Date29 Mar 2018 |
Sponsor / Collaborator |
100 Clinical Results associated with Orludodstat
Login to view more data
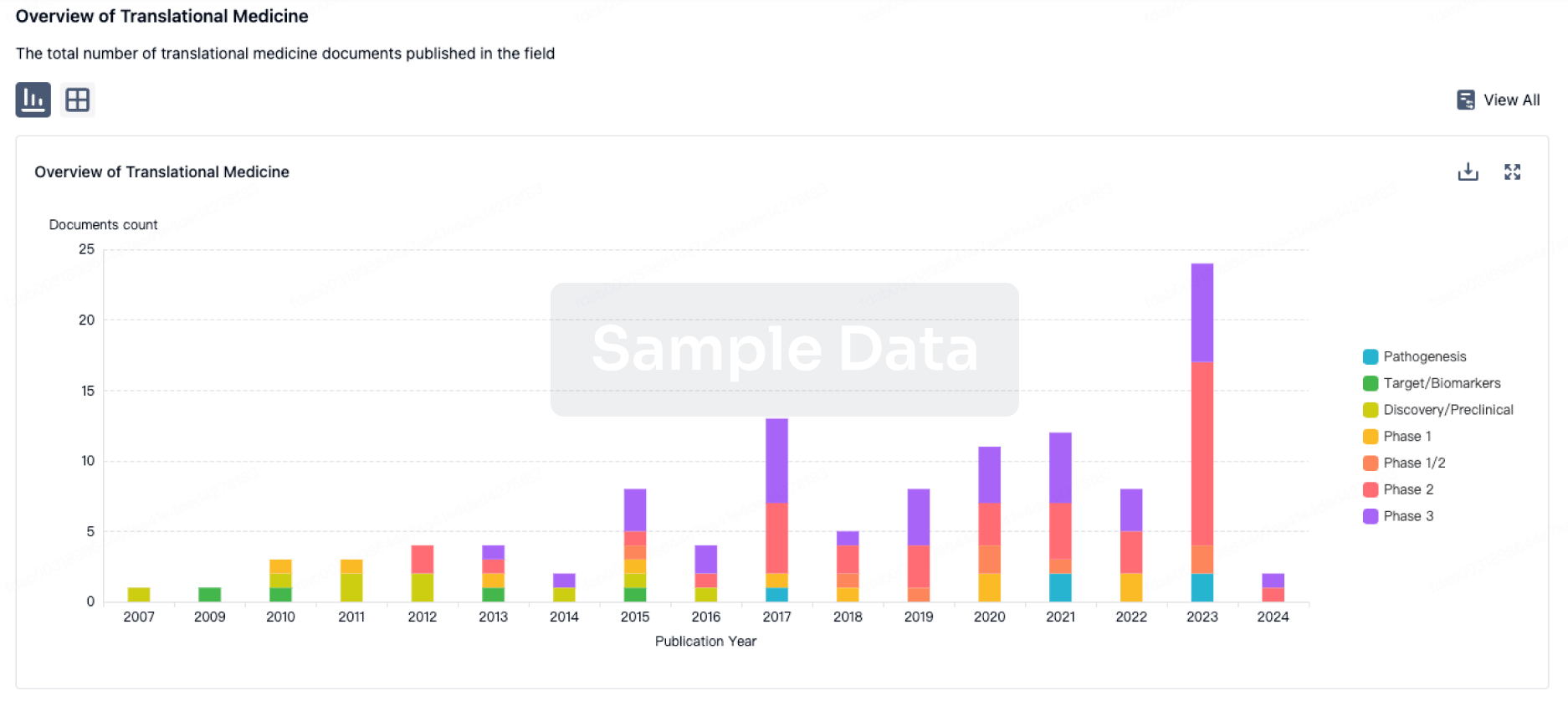
100 Translational Medicine associated with Orludodstat
Login to view more data
100 Patents (Medical) associated with Orludodstat
Login to view more data
26
Literatures (Medical) associated with Orludodstat01 Jun 2025·LIFE SCIENCES
Akt mitigates ER stress-instigated cardiac dysfunction via regulation of ferroptosis and mitochondrial integrity in a DHODH-dependent manner
Article
Author: Hu, Dandan ; Lin, Jie ; Shi, Wanting ; Xu, Kaishou ; Zhou, Na ; Ma, Li ; Reiter, Russel J ; Zhang, Yingmei ; Ren, Jun
ER stress evokes various types of cell death and myocardial dysfunction. This study aimed to discern the involvement of ferroptosis in chronic Akt activation-offered benefit, if any, against ER stress-triggered cardiac remodeling and contractile anomalies. Cardiac-selective expression of active mutant of Akt (AktOE) and wild-type (WT) mice were challenged with the ER stress instigator tunicamycin (1 mg/kg, 48 h) prior to assessment of cardiac morphology and function. Tunicamycin insult prompted cardiac remodeling (interstitial fibrosis), deranged echocardiographic (higher LVESD, dropped ejection fraction and fractional shortening), cardiomyocyte mechanical and intracellular Ca2+ features alongside mitochondrial injury (collapsed mitochondrial membrane potential and ultrastructural change), oxidative stress, compromised Akt-GSK3β signaling, ER stress (upregulated GRP78 and Gadd153), carbonyl formation, apoptosis and ferroptosis (decreased GPX4, SLC7A11). Intriguingly, tunicamycin-evoked anomalies (except GRP78 and Gadd153) were abrogated by Akt activation. Chronic Akt activation negated tunicamycin-induced downregulation of ferric flavin enzyme dihydroorotate dehydrogenase (DHODH), which catalyzes the fourth step of pyrimidine ab initio biosynthesis, and conversion of dihydroorotic acid to orotate. ER stress-induced myocardial anomalies were reversed by the newly identified PI3K activator triptolide, DHODH activator menaquinone-4 and pyrimidine booster coenzyme Q. In vitro experiment revealed that Akt activation- or triptolide-evoked beneficial responses against tunicamycin-induced cardiomyocyte anomalies were cancelled off by DHODH inhibitor BAY2402234 or ferroptosis inducer erastin. These findings support that chronic Akt activation rescues ER stress-evoked myocardial derangements through DHODH-dependent control of ferroptosis and mitochondrial homeostasis.
01 Jan 2025·Cell Reports Medicine
Metabolic profiling of patient-derived organoids reveals nucleotide synthesis as a metabolic vulnerability in malignant rhabdoid tumors
Article
Author: Proost, Natalie ; Morales-Rodriguez, Francisco ; van den Heuvel-Eibrink, Marry M ; Zaal, Esther A ; Drost, Jarno ; Berkers, Celia R ; van de Ven, Marieke ; Kes, Marjolein M G ; de Souza, Terezinha ; Jansen, Jeroen W A
Malignant rhabdoid tumor (MRT) is one of the most aggressive childhood cancers for which no effective treatment options are available. Reprogramming of cellular metabolism is an important hallmark of cancer, with various metabolism-based drugs being approved as a cancer treatment. In this study, we use patient-derived tumor organoids (tumoroids) to map the metabolic landscape of several pediatric cancers. Combining gene expression analyses and metabolite profiling using mass spectrometry, we find nucleotide biosynthesis to be a particular vulnerability of MRT. Treatment of MRT tumoroids with de novo nucleotide synthesis inhibitors methotrexate (MTX) and BAY-2402234 lowers nucleotide levels in MRT tumoroids and induces apoptosis. Lastly, we demonstrate in vivo efficacy of MTX in MRT patient-derived xenograft (PDX) mouse models. Our study reveals nucleotide biosynthesis as an MRT-specific metabolic vulnerability, which can ultimately lead to better treatment options for children suffering from this lethal pediatric malignancy.
01 Jul 2024·European journal of haematology
Pivotal role of dihydroorotate dehydrogenase as a therapeutic target in adult T‐cell leukemia
Article
Author: Ishikawa, Chie ; Mori, Naoki
Abstract:
Objectives:
We aimed to determine the role of dihydroorotate dehydrogenase (DHODH) in pathogenesis of adult T‐cell leukemia (ATL) caused by human T‐cell leukemia virus type 1 (HTLV‐1) and the effects of its inhibition on the de novo pyrimidine biosynthesis pathway.
Methods:
Cell proliferation, viability, cycle, and apoptosis were analyzed using WST‐8 assays, flow cytometry, and Hoechst 33342 staining. To elucidate the molecular mechanisms involved in the anti‐ATL effects of DHODH knockdown and inhibition, RT‐PCR and immunoblotting were conducted.
Results:
HTLV‐1‐infected T‐cell lines aberrantly expressed DHODH. Viral infection and the oncoprotein, Tax, enhanced DHODH expression, while knockdown of DHODH decreased HTLV‐1‐infected T‐cell growth. In addition, BAY2402234, a DHODH inhibitor, exerted an anti‐proliferative effect, which was reversed by uridine supplementation. BAY2402234 induced DNA damage and S phase arrest by downregulating c‐Myc, CDK2, and cyclin A and upregulating p53 and cyclin E. It also induced caspase‐mediated apoptosis by the upregulation of pro‐apoptotic and downregulation of anti‐apoptotic proteins. Furthermore, BAY2402234 induced caspase‐independent ferroptosis and necroptosis. It decreased phosphorylation of IKK, IκBα, PTEN, Akt, and its downstream targets, suggesting that inhibition of NF‐κB and Akt signaling is involved in its anti‐ATL action.
Conclusion:
These findings highlight DHODH as a potential therapeutic target for treating ATL.
2
News (Medical) associated with Orludodstat17 Nov 2022
New research out of McMaster University found a recently abandoned Bayer compound halted the growth of an aggressive form of pediatric medulloblastoma in mouse models.
Brain tumors have overtaken leukemia as the deadliest childhood cancer. The MYC gene-amplified type of medulloblastoma is the deadliest of the four subgroups, forming highly malignant tumors characterized by therapy resistance and disease recurrence. Even in the cases that are "curable," the cure comes at a steep price for this vulnerable population.
"We often use mortality as our success measure with cancer treatment," William Gwynne, a postdoc at McMaster and first author of the study, told BioSpace.
"Unfortunately, that's not an accurate measuring stick to how well we're doing with cancer treatment. Because even though 70% of medulloblastoma patients will be cured with standard of care - chemotherapy and radiation - almost 100% of them will have what we call neurotoxic second delay," he continued. This refers to a series of neurocognitive and developmental deficits.
Gwynne joined Dr. Sheila Singh's lab for his postdoc training, intrigued by her approach to studying cancer using a comparative developmental biology perspective. Singh is a pediatric neurosurgeon, so this is a need acutely felt in her own patient population.
The Singh Lab team utilized genome-wide CRISPR screening to compare medulloblastoma to neural stem cells.
They identified the genes highly essential for survival of the cancer cells, but non-essential to the stem cells. A collaboration with J. Rafael Montenegro-Burke from the University of Toronto dug into the metabolic profiles of the neural cells versus the medulloblastoma cells. Both the gene research and metabolic research pointed at the same thing, which got the research team "really, really excited."
An Excellent Druggable Target
"It turns out that this enzyme, DHODH, which fuels the production of these pyrimidine molecules, was an excellent druggable target," Gwynne said. "It was being pursued in other cancer types like leukemia. But nobody had pursued this in brain cancer yet."
The team utilized the DHODH inhibitor created by Bayer, BAY2402234, due to its ability to highly penetrate the blood-brain barrier, something other inhibitors like brequinar were unable to do.
The compound had been in a Bayer-sponsored trial for patients with acute myeloid leukemia, but in January the trial was terminated due to "lack of sufficient clinical benefit."
Gwynne pointed to selection of the "right patients" as being the potential key benefit of a DHODH inhibitor. The research zeroed in on a specific set of patients with MYC-driven medulloblastoma because the DHODH pathway is particularly high in those cells. Inhibiting the DHODH in these cells evokes metabolic stress to halt the cycle progression and induce cell death.
An important factor in any new research is reproducibility. Singh and Gwynne's research was published Nov. 10 in Cancer Cell. In August, two other papers were published in Cancer Cell, one targeting IDH mutant glioma and another studying a near-universally fatal brainstem tumor.
These two papers came to the same conclusion as Singh's lab. All three teams utilized BAY2402234 to inhibit DHODH for three different kinds of brain cancers, and all signs point to it being a promising approach to stopping brain tumor growth.
Gwynne and Singh are most excited about this potential new treatment approach because of its cancer-targeting effects with minimal impact on healthy cells.
Current, standard treatments like radiation and chemotherapy don't distinguish between normal and cancer cells. Neurotoxic effects from these therapies leave 40-100% of pediatric brain tumor survivors with cancer-related cognitive impairment.
"It's just amazing how this is really a cancer-selected metabolic vulnerability," Singh told BioSpace.
Neuro Stem Cells Relatively Untouched
"Only the cancer cells are disabled by this drug. The neuro stem cells are... relatively untouched by the drug at the same dose," she said. This is important because clinical trial subjects are small children with pools of stem cells that are rapidly divided into developing and creating new organs and laying down new pathways in the brain.
"So, it's absolutely essential that any drug we use doesn't target those developing cell populations."
In the lab, Gwynne observed how gaunt and sickly the mice treated with chemo and radiation were, as is typical in these studies. In stark contrast, the mice treated with the Bayer compound were "running around the cage happy and healthy." Those mice also outlived the mice receiving traditional treatments.
"This single agent DHODH inhibitor was as effective as current standard of care in this mouse model without the side effects of the mice becoming really, really sick and getting really, really skinny like they normally do," Gwynne said.
Due to the low-toxicity profile, Singh said a Phase I clinical trial is the next logical step. Bayer has yet to contact her, but a lot of interest has surfaced since the paper's publishing.
"I've been contacted by drug developers who are interested and they're asking me questions like, do you think this could translate to clinical trials?Our papers have reenergized interest around that compound."
BioSpace reached out to Bayer for comment but had not heard back at the time of this publication.
15 Nov 2022
Scientists hope new findings could translate to treatments for medulloblastoma that have fewer side effects than the ones in use today.
Medulloblastoma is a relatively treatable pediatric brain cancer, with survival rates of about 80% if it's treated before it spreads. But in addition to surgery, most cases require chemotherapy and radiation—treatments that can harm brain development and set the stage for complications later in life.
Now, it appears that blocking a key enzyme could offer a better path to treating medulloblastoma. In a study published Nov 10. in Cancer Cell, scientists at McMaster University in Ontario described how they used a Bayer compound to curtail the cancer's spread in mouse models of its most aggressive subtype.
“This potential treatment pathway will allow us to kill the weeds but save the flower of the developing brain,” William Gwynne, first author, said in a press release.
The enzyme at the heart of the study is dihydroorotate dehydrogenase, or DHODH. It’s a key part of the de novo pyrimidine synthesis pathway, a pathway that ultimately leads to the creation of DNA and RNA and is known to be hijacked by cancers in their effort to grow. DHODH inhibitors like Sanofi’s Arava and Aubagio are FDA approved for the treatment of rheumatoid arthritis and multiple sclerosis, respectively, while others are under investigation against a wide breadth of conditions, including viruses and several types of cancer.
The McMaster team’s findings add one more potential indication to the list. The scientists homed in on DHODH by screening the genomes and metabolic processes of MYC-amplified medulloblastoma, a particularly deadly subtype of the brain cancer. They found alterations in the de novo pyrimidine synthesis pathway, and genetic analyses in cells and mice showed that knocking out DHODH could hinder medulloblastoma growth.
The scientists then sought to find out whether an orally administered DHODH inhibitor could stop tumor growth in mice. They treated mouse models of MYC-amplified medulloblastoma with a compound called BAY2402234, which, until this past January was under investigation by Bayer for the treatment of acute myeloid leukemia and glioma. The researchers found that the compound was able to reduce tumor growth and improve survival times in the mice, increasing their life spans from about 28 days in controls to around 38 days in the ones that were treated with BAY2402234.
While the team didn’t assess whether the compound had an impact on the brain development of young mice, they did find that it wasn’t harmful to cultured neural stem cells. In contrast, radiation is well known to impact neural stem cells in both children and adults and is thought to be the reason for brain damage associated with its use. Chemotherapy has been shown to kill brain cells as well, a possible explanation for the phenomenom of “chemo brain” described by patients.
Given these results and the fact that BAY2402234 has already been proven safe in humans during clinical trials at the equivalent doses to the ones used in their study, the researchers called for further optimizing DHODH inhibitors preclinically in medulloblastoma both alone and in combination with other treatments. If they perform well, the drugs should be translated to clinical research, the researchers wrote in their paper.

Radiation TherapyDrug ApprovalClinical Result
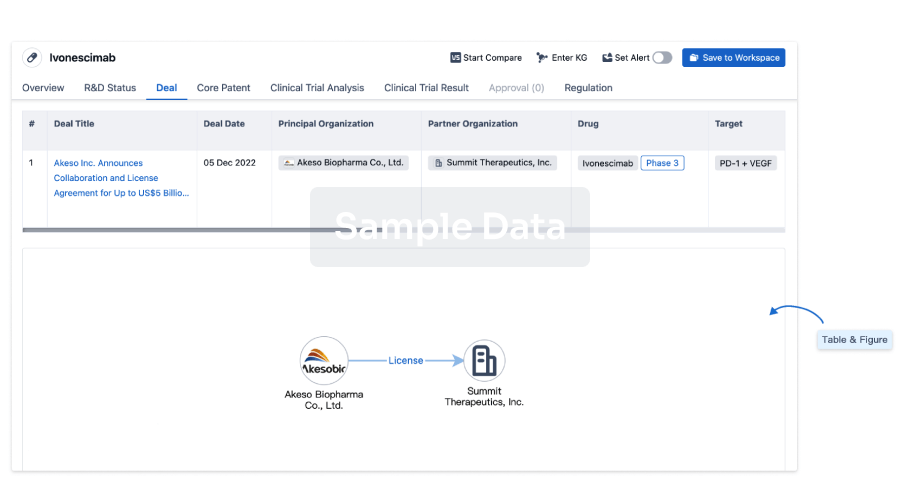
100 Deals associated with Orludodstat
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Recurrent Glioma | Phase 1 | - | 01 Dec 2021 | |
| Chronic Myelomonocytic Leukemia | Phase 1 | United States | 29 Mar 2018 | |
| Chronic Myelomonocytic Leukemia | Phase 1 | France | 29 Mar 2018 | |
| Myeloid Tumor | Phase 1 | United States | 29 Mar 2018 | |
| Myeloid Tumor | Phase 1 | France | 29 Mar 2018 | |
| Refractory acute myeloid leukemia | Phase 1 | United States | 29 Mar 2018 | |
| Refractory acute myeloid leukemia | Phase 1 | France | 29 Mar 2018 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
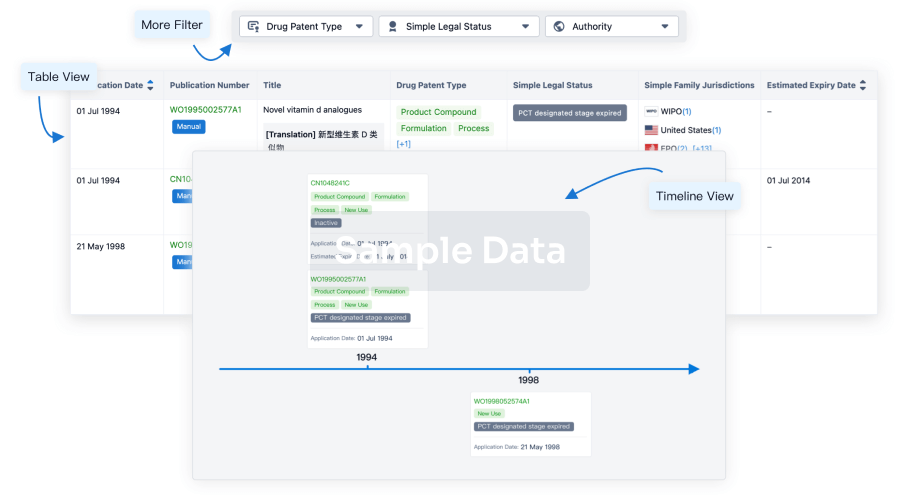
Core Patent
Boost your research with our Core Patent data.
login
or
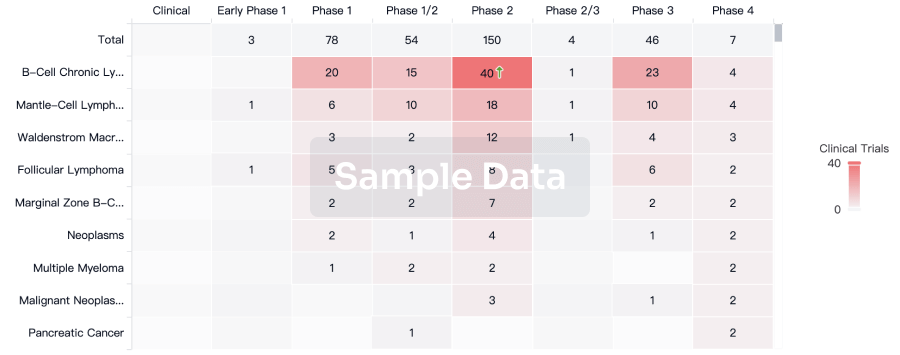
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
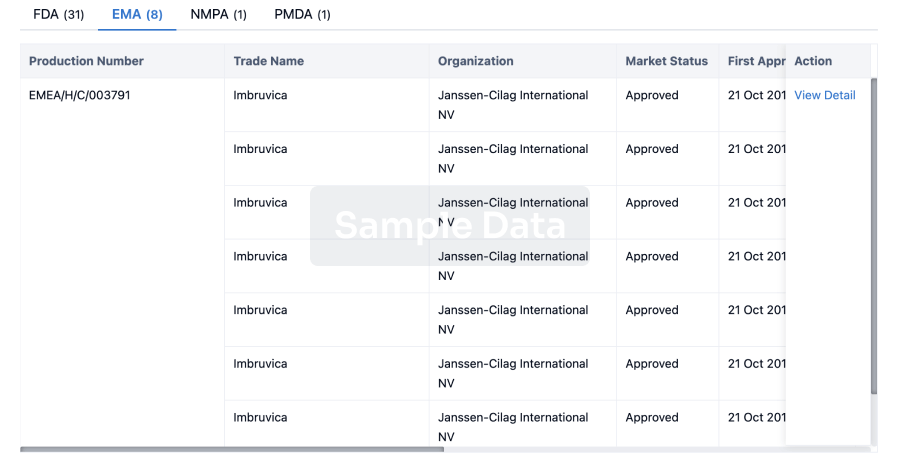
Approval
Accelerate your research with the latest regulatory approval information.
login
or
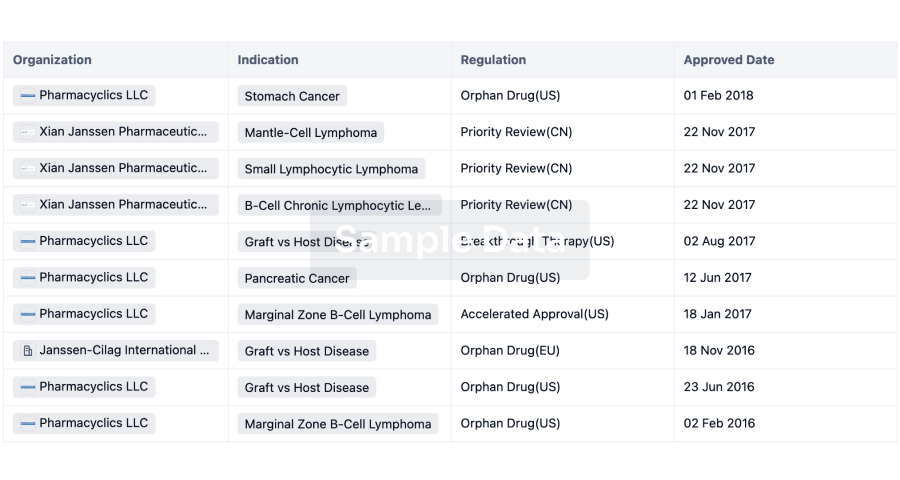
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


