Request Demo
Last update 08 May 2025
Qilu Pharmaceuticals Co. Ltd.
Private Company|2016|Shandong Sheng, China
Private Company|2016|Shandong Sheng, China
Last update 08 May 2025
Overview
Tags
Endocrinology and Metabolic Disease
Respiratory Diseases
Neoplasms
Antibody drug conjugate (ADC)
Disease domain score
A glimpse into the focused therapeutic areas
No Data
Technology Platform
Most used technologies in drug development
No Data
Targets
Most frequently developed targets
No Data
| Disease Domain | Count |
|---|---|
| Neoplasms | 1 |
| Endocrinology and Metabolic Disease | 1 |
| Top 5 Drug Type | Count |
|---|---|
| Antibody drug conjugate (ADC) | 1 |
| Top 5 Target | Count |
|---|---|
| CLDN6 x Top I | 1 |
Related
1
Drugs associated with Qilu Pharmaceuticals Co. Ltd.Target |
Mechanism CLDN6 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePhase 1 |
First Approval Ctry. / Loc.- |
First Approval Date- |
100 Clinical Results associated with Qilu Pharmaceuticals Co. Ltd.
Login to view more data
0 Patents (Medical) associated with Qilu Pharmaceuticals Co. Ltd.
Login to view more data
29
Literatures (Medical) associated with Qilu Pharmaceuticals Co. Ltd.21 Apr 2025·Cancer Research
Abstract 3495: QL535, A novel CD2-costimulating T cell engager targeting PSMA-positive prostate cancer matching CD28 trispecific antibody in cytotoxicity, minimizing cytokine release and T-cell exhaustion
Author: Ngo, Nathan ; Liu, Ke ; Chen, Shihao ; Zhao, Shuyong ; Kong, Jiantao ; Liu, Hao ; Wang, Yuxia ; Liu, Xiao ; Chen, Jane ; Zhu, Hejie ; Fang, Yan ; Ma, Ruixue ; Morrissette, Joshua ; Hu, Moyan ; Zhang, Xin ; Guo, Guangjie ; Cao, Jiaming ; Wang, Liwei ; Sun, Min ; Gu, Shenda
21 Apr 2025·Cancer Research
Abstract 1743: QLS1209, A highly potent and selective PKMYT1 inhibitor demonstrates activity in tumors with CCNE1Amp and/ or FBXW7LoF mutations
Author: Chen, Jianping ; Lei, Guangyue ; Hao, Junguo ; He, Changliang ; Qin, Hua ; Qian, Wenyuan ; Shi, Guqin ; Wang, Zheng ; Zheng, Qingmei ; Tao, Weikang ; Zhang, Yuxing ; Wang, Rongyan ; Sun, Weimei ; Sun, Daqing ; Cheng, Xinghua ; Fu, Jiasheng ; Chen, Ping ; Li, Ling ; Shao, Xinrui ; Yang, Dong
21 Apr 2025·Cancer Research
Abstract 2135: QLS4131, a proprietary T cell engager targeting both BCMA and GPRC5D for the treatment of multiple myeloma
Author: Qian, Hongliang ; Yang, Liuqing ; Luo, Juan ; Zhao, Shuyong ; Zhang, Ling ; Ying, Hua ; Tao, Weikang ; Liu, Ke
6
News (Medical) associated with Qilu Pharmaceuticals Co. Ltd.21 Jan 2025
First Berlin Equity Research on 01/21/2025 initiated coverage on Lisata Therapeutics, Inc. (ISIN: US1280583022/ Bloomberg: LSTA US). Analyst Christian Orquera placed a BUY rating on the stock, with a USD 15.00 price target. A summary of the report is available below. To view the full report, please Click Here
CERTEPETIDE – THE COMPANION OF CHOICE TO IMPROVE CANCER THERAPY
Abstract: Lisata Therapeutics Inc (Lisata), previously Caladrius Biosciences and renamed after the merger with Cend Therapeutics in 2022, is a US clinical-stage pharmaceutical company focused on the development of innovative therapies for the treatment of advanced solid tumours and other serious diseases. Its lead drug candidate, certepetide, is a peptide with a dual mode of action which (1) enhances penetration of co-administered anti-cancer drugs into solid tumours and (2) modifies the tumour microenvironment (TME) by reducing immunosuppressive cell populations, such as regulatory T cells (Tregs), and increasing cytotoxic T cells. This modulation has the potential to enhance the efficacy of chemo- and immunotherapies and concurrently inhibit the progression of metastasis, making certepetide an ideal combination with standard cancer therapy. The drug candidate is in clinical development in seven trials for a number of indications: (1) 1st and 2nd line metastatic pancreatic ductal adenocarcinoma (mPDAC), (2) locally advanced non-resectable PDAC, (3) 1st and 2nd line cholangiocarcinoma, (4) 1st line glioblastoma multiforme and (5) pancreatic, colon and appendiceal cancer. In addition, Lisata has licensed the exclusive rights for certepetide in Greater China to Qilu Pharmaceuticals under a lucrative agreement with potential milestone payments of up to USD221m. Qilu conducted a phase 1b/2a study and is now carrying out a phase 2 study in the lead 1st line mPDAC indication. Lisata's own ongoing two-cohort ASCEND phase 2b study in 1st line mPDAC is expected to report results from the first cohort in January 2025 and from the second cohort by Q2/Q3 2025. We see 2025 as an exciting year for Lisata as we also expect results on the other ongoing trials of certepetide, which will likely act as a catalyst for the share price. Our sum-of-the-parts valuation model yields a price target of USD15.00. We initiate coverage of Lisata with a Buy recommendation.
Phase 2ImmunotherapyLicense out/in
04 Mar 2024
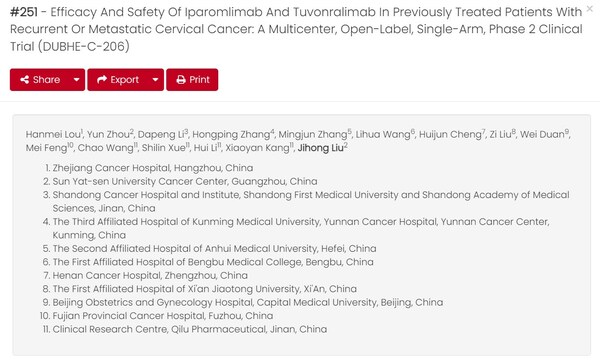
JINAN, China, March 4, 2024 /PRNewswire/ -- The European Society of Gynecological Oncology (ESGO) 2024 Conference has recently made selected abstracts available online. The abstract (abstract # 251) that details results from the Phase II clinical trial (DUBHE-C-206) evaluating the efficacy and safety of Qilu Pharmaceuticals' iparomlimab and tuvonralimab (QL1706) in cervical cancer was selected for oral presentation on 8 March, local time.
Access the abstract here: !
Continue Reading
image
This study was led by Professor Jihong Liu from the Sun Yat-sen University Cancer Center and Professor Hanmei Lou from the Zhejiang Cancer Hospital. This was a multi-center, single-arm, phase II study which recruited patients with recurrent or metastatic cervical cancer unresponsive to first-line platinum-based chemotherapy (with or without bevacizumab) and without prior immunotherapy. Participants received QL1706 at a dose of 5.0 mg/kg once every three weeks (Q3W). The study involved 38 medical centers across China and enrolled 148 patients, with a median follow-up of 11.0 months at the data cut-off. The primary endpoint, the objective response rate (ORR), as assessed by an Independent Evaluation Committee (IRC), was 33.8%, meeting the prespecified criteria. The disease control rate (DCR) was 64.9% and median progression-free survival (PFS) was 5.4 months. Overall survival (OS) was not reached. Treatment-related adverse events (TRAEs) occurred in 104 (70.3%) subjects, with 36 (24.3%) experiencing grade ≥3 TRAEs. Anemia (4.1%) was the most common TRAE. Treatment discontinuation due to TRAEs occurred in three patients (2.0%). TRAE leading to death didn't occur.
The trial indicates that QL1706 is an effective and safe therapy for patients with recurrent or metastatic cervical cancer whose disease progressed after first-line standard of care. In August 2023, the China NMPA, Center for Drug Evaluation (CDE) accepted the new drug application for QL1706, making it the first MabPair product targeting PD-1 and CTLA-4 worldwide and a potential new treatment option for patients with cervical cancer.
Photo -
Logo -
Phase 2Clinical ResultIND
02 Aug 2023
FDA sign outside its office in Maryland
iStock,
JHVEPhoto
Following reports of destroyed and discarded data, the U.S. regulator issued a warning letter to India’s Intas Pharmaceuticals regarding violations of current good manufacturing practice.
Pictured: FDA sign at its headquarters in Washington DC/iStock,
JHVEPhoto
The FDA on Friday issued a
warning letter
to India-based generics manufacturer
Intas Pharmaceuticals
citing several quality control issues at its Sanand plant, including “significant violations” of current good manufacturing practice as well as destroyed and discarded data.
The letter revealed that in November 2022 an Intas analyst was seen pouring acetic acid into a trash bin that was containing current good manufacturing practice (CGMP) records. A quality control officer had also witnessed the same analyst destroy data sheets including balance printouts and titration curves. The employee reported these incidents to company management but Intas did not launch an investigation until a week later, according to the FDA’s letter.
Another Intas analyst, after weighing out amitriptyline hydrochloride tablets multiple times, told FDA investigators that he did not report all of the results. In other instances, the analyst said, he would throw away balance printouts.
FDA investigators also found plastic bags full of discarded CGMP documents across the manufacturing facilities, suggesting that Intas had gotten rid of Environmental Monitoring Systems engineering checklists, several analytical test reports, titration curves and balance weight slips for drug products.
Intas had been made aware of these infractions, among several others, in a 36-page document issued last December 2022. The FDA detailed these issues again in Friday’s warning letter, adding that while Intas had previously promised to work with consultants to evaluate its data governance protocols, its efforts had so far still not met the FDA’s requirements.
“Your response is inadequate in that it did not fully evaluate the scope of this deficiency and the impact to product quality,” the FDA said in the warning letter. “You did not adequately address the major failure of laboratory, operations, and quality assurance management to conduct proper oversight over documentation and prevent data integrity lapses.”
As of June 1, Intas is on the FDA’s
Import Alert
list, which allows the regulator’s field staff to detain products from the company even without physical examination, given repeated evidence of its CGMP violations. The alert covers several cancer drugs, including carboplatin and cisplatin, which are currently in critical short supply in the U.S.
In an
interview
with
BioSpace
last month, Erin Fox of the American Society of Health-System Pharmacists said that Intas had been responsible for approximately half of the supply of these two drugs, and that the closure of its Gujarat facility could have contributed greatly to the current shortage crisis.
Currently, the FDA has resorted to importing these drugs from other manufacturers in other countries,
announcing
in May that it would source cisplatin from Chinese drugmaker Qilu Pharmaceuticals. This is only a temporary fix, however, as
strong legislative incentives
are needed to produce these medicines domestically.
Last week, House Republicans
released a draft bill
designed specifically to address the drug shortage and prevent a similar crisis from happening in the future. One of the draft’s provisions is to launch a pilot program to accelerate the licensing of domestic manufacturing facilities.
Tristan Manalac is an independent science writer based in metro Manila, Philippines. He can be reached at
tristan@tristanmanalac.com
or
tristan.manalac@biospace.com
.
100 Deals associated with Qilu Pharmaceuticals Co. Ltd.
Login to view more data
100 Translational Medicine associated with Qilu Pharmaceuticals Co. Ltd.
Login to view more data
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 20 Oct 2025
The statistics for drugs in the Pipeline is the current organization and its subsidiaries are counted as organizations,Early Phase 1 is incorporated into Phase 1, Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3
Preclinical
1
Login to view more data
Current Projects
| Drug(Targets) | Indications | Global Highest Phase |
|---|---|---|
QLS5132 ( CLDN6 x Top I ) | Testicular Neoplasms More | Preclinical |
Login to view more data
Deal
Boost your decision using our deal data.
login
or

Translational Medicine
Boost your research with our translational medicine data.
login
or

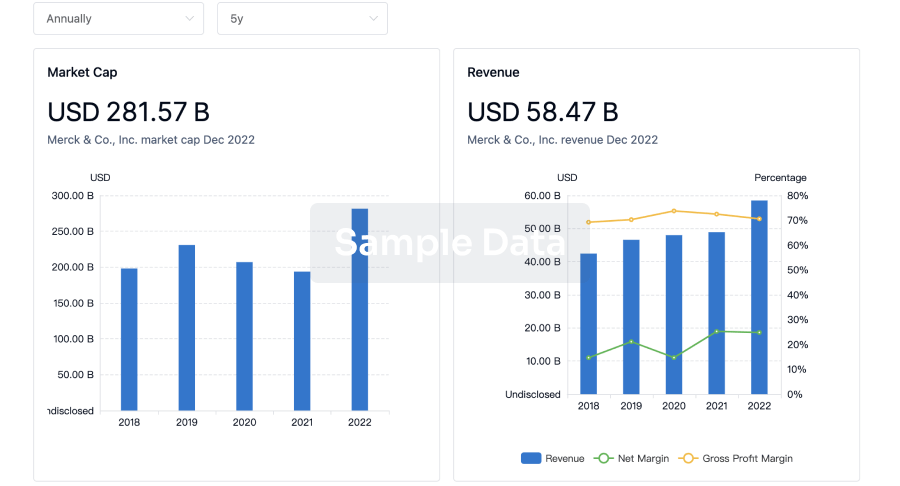
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
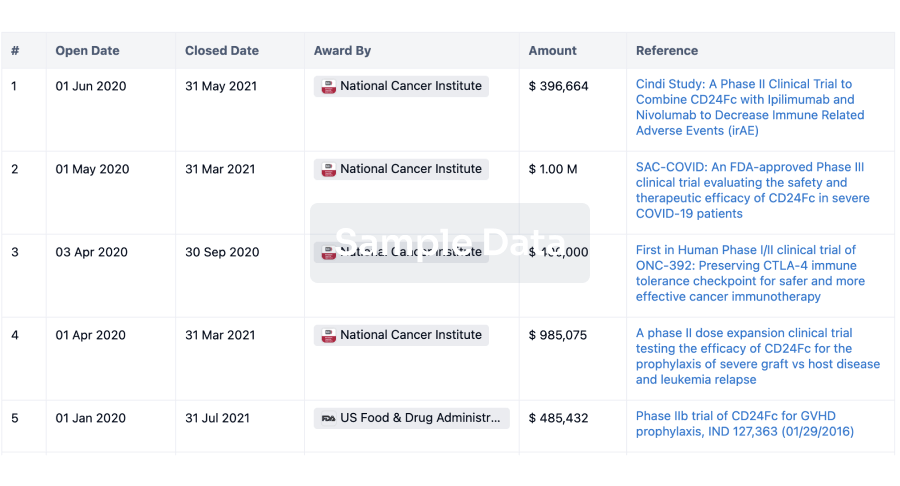
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
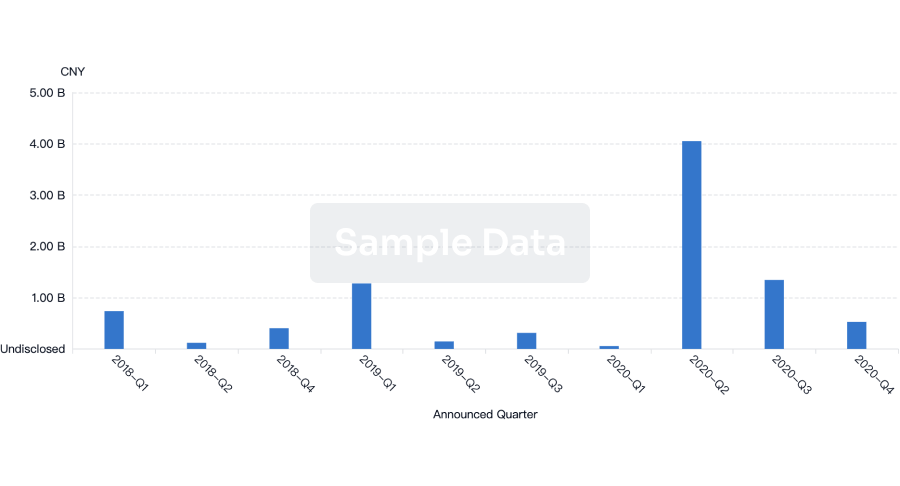
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
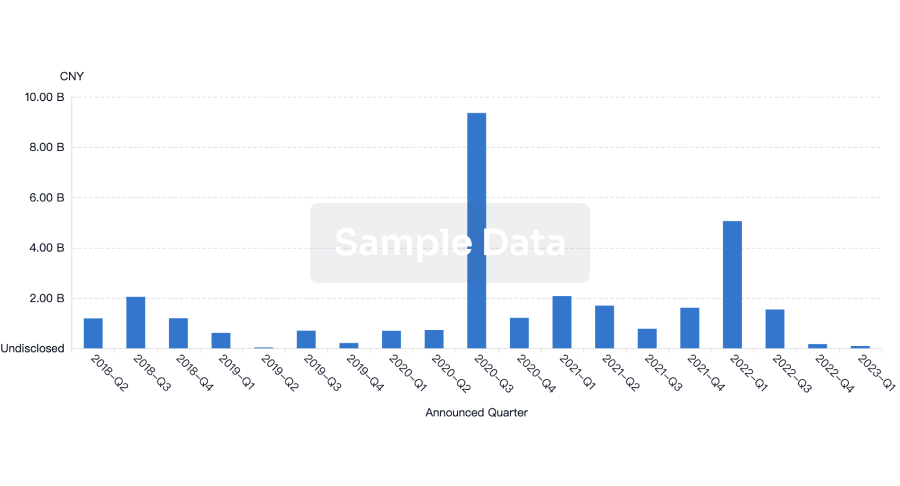
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
