Request Demo
Last update 08 May 2025
HighTide Therapeutics (Hong Kong) Ltd.
Private Company|2018|Hong Kong SAR, China
Private Company|2018|Hong Kong SAR, China
Last update 08 May 2025
Overview
Tags
Endocrinology and Metabolic Disease
Digestive System Disorders
Other Diseases
Small molecule drug
Chemical drugs
Synthetic peptide
Disease domain score
A glimpse into the focused therapeutic areas
No Data
Technology Platform
Most used technologies in drug development
No Data
Targets
Most frequently developed targets
No Data
| Disease Domain | Count |
|---|---|
| Endocrinology and Metabolic Disease | 5 |
| Nervous System Diseases | 1 |
| Top 5 Drug Type | Count |
|---|---|
| Small molecule drug | 4 |
| Chemical drugs | 2 |
| Synthetic peptide | 1 |
| Top 5 Target | Count |
|---|---|
| NGFB x TLR4 | 1 |
| AMPK x Lipid x NLRP3 | 1 |
Related
8
Drugs associated with HighTide Therapeutics (Hong Kong) Ltd.Target |
Mechanism AMPK agonists [+2] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhasePhase 3 |
First Approval Ctry. / Loc.- |
First Approval Date- |
Target |
Mechanism NGFB stimulants [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhasePhase 2 |
First Approval Ctry. / Loc.- |
First Approval Date- |
Target- |
Mechanism- |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhasePhase 1 |
First Approval Ctry. / Loc.- |
First Approval Date- |
13
Clinical Trials associated with HighTide Therapeutics (Hong Kong) Ltd.CTR20242631
一项在轻、中度肾功能损害受试者与匹配的肾功能正常对照受试者中评价HTD1801药代动力学的I期、开放标签、平行组、单次给药研究
[Translation] A Phase I, open-label, parallel-group, single-dose study evaluating the pharmacokinetics of HTD1801 in subjects with mild to moderate renal impairment and matched controls with normal renal function
首要目的:在轻度和中度肾功能损害受试者与匹配的肾功能正常对照受试者中确定HTD1801的单次给药PK特征。
次要目的:1、在轻度和中度肾功能损害受试者与匹配的肾功能正常对照受试者中评估HTD1801的安全性和耐受性;2、在轻度和中度肾功能损害受试者与匹配的肾功能正常对照受试者中评估HTD1801的血浆蛋白结合情况;3、评估基线肾功能与PK参数之间的关系。
[Translation]
Primary objective: To determine the single-dose PK characteristics of HTD1801 in subjects with mild and moderate renal impairment and matched control subjects with normal renal function.
Secondary objectives: 1. To evaluate the safety and tolerability of HTD1801 in subjects with mild and moderate renal impairment and matched control subjects with normal renal function; 2. To evaluate the plasma protein binding of HTD1801 in subjects with mild and moderate renal impairment and matched control subjects with normal renal function; 3. To evaluate the relationship between baseline renal function and PK parameters.
Start Date02 Sep 2024 |
Sponsor / Collaborator |
CTR20242600
[14C-B]HTD1801在健康受试者中的单中心、非随机、开放、单次给药的物质平衡研究
[Translation] [14C-B] A single-center, non-randomized, open-label, single-dose mass balance study of HTD1801 in healthy subjects
主要研究目的:
1) 定量分析男性健康受试者单次口服[14C-B]HTD1801后,排泄物(尿液和粪便)中的总放射性量,获得人体放射性的累积排泄率;
2) 鉴定男性健康受试者单次口服[14C-B]HTD1801后人体内的代谢产物,确定主要生物转化途径和主要代谢产物结构;
3) 考察男性健康受试者单次口服[14C-B]HTD1801后,全血和血浆中总放射性的分配情况以及血浆总放射性的药代动力学。
次要研究目的:
1) 采用已验证的液相色谱-串联质谱法(LC-MS/MS)定量分析血浆中的小檗碱及其主要代谢产物(如适用)的浓度,获得小檗碱及其主要代谢产物(如适用)的药动学参数;
2) 评价[14C-B]HTD1801单次给药后男性健康受试者的安全性。
[Translation]
Main study objectives:
1) To quantitatively analyze the total radioactivity in excreta (urine and feces) after a single oral administration of [14C-B]HTD1801 to healthy male subjects, and obtain the cumulative excretion rate of radioactivity in the human body;
2) To identify the metabolites in the human body after a single oral administration of [14C-B]HTD1801 to healthy male subjects, and determine the main biotransformation pathways and the structures of the main metabolites;
3) To investigate the distribution of total radioactivity in whole blood and plasma and the pharmacokinetics of total radioactivity in plasma after a single oral administration of [14C-B]HTD1801 to healthy male subjects.
Secondary study objectives:
1) To quantitatively analyze the concentration of berberine and its main metabolites (if applicable) in plasma using a validated liquid chromatography-tandem mass spectrometry (LC-MS/MS) method, and obtain the pharmacokinetic parameters of berberine and its main metabolites (if applicable);
2) To evaluate the safety of healthy male subjects after a single administration of [14C-B]HTD1801.
Start Date12 Aug 2024 |
Sponsor / Collaborator |
NCT06415773
A Phase 3, Multicenter, Randomized, Double-Blind, Active-Controlled (Dapagliflozin), Parallel Group Efficacy and Safety Study of HTD1801 in Patients with Type 2 Diabetes Mellitus Inadequately Controlled with Metformin Alone
The goal of this clinical study is to evaluate the efficacy and safety of berberine ursodeoxycholate (HTD1801) compared to dapagliflozin in patients with type 2 diabetes inadequately controlled with metformin alone.
Start Date04 Jun 2024 |
Sponsor / Collaborator |
100 Clinical Results associated with HighTide Therapeutics (Hong Kong) Ltd.
Login to view more data
0 Patents (Medical) associated with HighTide Therapeutics (Hong Kong) Ltd.
Login to view more data
5
Literatures (Medical) associated with HighTide Therapeutics (Hong Kong) Ltd.11 Feb 2021·Journal of Biomolecular Structure and Dynamics
A new analogue of islet neogenesis associated protein with higher structural and plasma stability
Article
Author: Maiztegui, Barbara ; Flores, Luis Emilio ; McCarthy, Andrés Norman ; Lynn, Soledad ; Diambra, Luis ; Liping, Liu ; Román, Carolina Lisi ; Ricardo Espinosa Silva, Yanis ; Ru, Bai ; Gagliardino, Juan José
01 Jan 2017·Journal of Diabetes ResearchQ3 · MEDICINE
Forkhead Protein FoxO1 Acts as a Repressor to Inhibit Cell Differentiation in Human Fetal Pancreatic Progenitor Cells
Q3 · MEDICINE
ArticleOA
Author: Jiang, Zongzhe ; Huang, Zhenhe ; Liu, Liping ; Zhang, Wenjian ; Yan, Hao ; Lou, Jinning ; Tian, Jingjing ; Ma, Xiaosong
JAMA Network Open
A Randomized Clinical Trial
Article
Author: Liu, Kui ; Li, Sheli ; Gan, Shenglian ; Ma, Jianhua ; Cheng, Zhifeng ; Ji, Linong ; Liu, Liping ; Wang, Kun ; Bai, Jie ; Xue, Xia ; Li, Shu ; Ma, Yujin ; Yuan, Guoyue ; Cai, Hanqing ; Liu, Dexue ; Yu, Meng ; Liu, Yu
13
News (Medical) associated with HighTide Therapeutics (Hong Kong) Ltd.05 Jun 2024
ROCKVILLE, MD and SHENZHEN, CHINA, HighTide Therapeutics, Inc. (Stock Code: 2511.HK), a clinical stage biopharmaceutical company specializing in the development of multi-targeted therapies for chronic liver and metabolic diseases, announced that it will make multiple presentations at the European Association for the Study of the Liver (EASL) Congress, taking place from June 5-8, 2024 in Milan, Italy. The presentations include post-hoc analyses of the Phase 2a clinical study of berberine ursodeoxcyholate (HTD1801), a gut-liver anti-inflammatory metabolic modulator, in patients with metabolic dysfunction-associated steatohepatitis (MASH) and comorbid type 2 diabetes mellitus (T2DM) (NCT03656744).
“These data provide additional insight on the potential benefits of HTD1801, a novel, multifunctional therapy being developed for the treatment of patients with MASH and T2DM. The ongoing multi-regional Phase 2b study (CENTRICITY, NCT05623189), now fully enrolled, evaluates the histologic benefit of HTD1801 in this same patient population. We look forward to the results of CENTRICITY which is on track to read out in the first half of 2025,” said Dr. Leigh MacConell, Chief Development Officer of HighTide.
“Efficacy of Berberine Ursodeoxycholate (HTD1801) Compared to Ongoing Use of GLP-1 Receptor Agonists in Patients with MASH and T2DM” (Abstract SAT-227, Poster Presented June 8)
About the Abstract: As GLP-1 Receptor Agonists (GLP-1RAs) are prominently used in patients with T2DM and gaining attention as a potential treatment for MASH, this post-hoc comparative efficacy analysis evaluated ongoing GLP-1RA use compared to newly initiated HTD1801 treatment. This analysis suggests that HTD1801 provides greater benefit across multiple cardiometabolic endpoints compared to ongoing GLP-1RA use. These findings are important as they suggest that patients with MASH and T2DM, on concomitant GLP-1RA treatment, could achieve additional benefit with HTD1801 in terms of further glucose and lipid lowering as well as weight loss.
“Berberine Ursodeoxycholate (HTD1801) Provides a Unique Therapeutic Approach for Patients with Metabolic Liver Disease and Severe Insulin Resistance” (Abstract SAT-225, Poster Presented June 8)
About the Abstract: Insulin resistance is a significant risk factor for T2DM, obesity and MASH. HTD1801 enhances the utilization of glucose and fats through activation of AMP-activated protein kinase (AMPK), thereby improving insulin sensitivity. As HTD1801 is under development as a treatment for patients with MASH and T2DM, the objective of this post-hoc analysis was to evaluate the effects of HTD1801 based on degree of insulin resistance. These data demonstrate that HTD1801 can alleviate the metabolic inhibitory effects caused by hyperinsulinemia, leading to even greater metabolic benefits in patients with MASH and more severe insulin resistance and therefore may offer a unique therapeutic approach for individuals with MASH and T2DM.
“Time Course of Onset, Incidence, and Prevalence of Gastrointestinal Adverse Events with HTD1801 (Berberine Ursodeoxycholate) in Patients with MASH and T2DM” (Abstract SAT-243, Poster Presented June 8)
About the Abstract: The most commonly occurring adverse events (AEs) in studies of HTD1801 across several indications have been mild to moderate gastrointestinal (GI) AEs, primarily diarrhea and nausea. The purpose of this post-hoc analysis was to characterize the time course and severity of GI AEs in patients with MASH and T2DM treated with HTD1801 for 18 weeks. Diarrhea and nausea, the most commonly occurring of GI AEs, followed a trend that was consistent with all reported GI AEs; they showed early onset (within the first 4 weeks), were mild or moderate in severity, and importantly, showed a decreasing incidence and prevalence over the course of treatment. These data demonstrate that with continued treatment with HTD1801, GI tolerability improves supporting its potential for long-term use for the treatment of chronic disease, such as MASH.
About HighTide Therapeutics
HighTide Therapeutics, Inc. (HKEX: 2511) is a globally integrated biopharmaceutical company focusing on the discovery and development of first-in-class multifunctional multi-targeted therapies with chronic liver and metabolic diseases with significant unmet medical needs. The company is developing multiple clinical assets, including therapy for metabolic dysfunction-associated steatohepatitis (MASH), type 2 diabetes (T2DM), severe hypertriglyceridemia (SHTG), primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC). Berberine ursodeoxycholate (HTD1801), the company’s lead drug candidate, received Fast Track designation from the U.S. FDA for both NASH and PSC, as well as Orphan Drug designation for PSC. In China, HTD1801 has been included in the National Major New Drug Innovation Program under the 13th Five-Year Plan for Major Technology Project.
Disclaimer
The information contained herein is based solely on events or data available as of the date of this document. Unless required by law, we are under no obligation to update or publicly revise any forward-looking statements or events beyond those anticipated, even if new information, future events, or other circumstances arise after the date of the forward-looking statement. Please review this document carefully and be aware that our actual future performance or results may significantly deviate from expectations. All statements in this document are made as of the publication date and may change considering future developments.
For more information, please visit
Contact: pr@hightidetx.com
Phase 2Orphan DrugFast Track
26 Sep 2023
Pliant Therapeutics is part of a small band of biotechs working to address the unmet need in primary sclerosing cholangitis.
Investors are swayed by Pliant Therapeutics’ data. The biotech posted early clinical evidence that its lead drug candidate reduces scarring and itching in a chronic liver disease, sending its share price up around 15%.
The phase 2a trial is comparing bexotegrast, an oral, dual-selective inhibitor of two integrins, to placebo in patients with primary sclerosing cholangitis (PSC) and suspected liver fibrosis. PSC, a condition with no FDA-approved therapies, causes scarring of bile ducts and cirrhosis. Through tissue specific inhibition of TGF-β, bexotegrast may block fibrosis, leading Pliant to identify it as a potential treatment for PSC.
In the phase 2a trial, participants received one of three doses of bexotegrast or placebo. While the study is primarily designed to assess safety, tolerability and pharmacokinetics, Pliant also looked at exploratory efficacy endpoints such as changes in the fibrosis, biochemistry and imaging of the liver. The exploratory endpoints revealed early signs that bexotegrast may improve outcomes.
After 12 weeks of dosing, the ELF score, a blood test of fibrosis markers, was significantly lower in the high, 160-mg dose cohort than in the placebo group and numerically lower in all the bexotegrast arms. Pliant linked the high dose to an 84% reduction relative to placebo. The reduction was underpinned by significant declines in all three markers that make up the ELF score.
Pliant also reported a significant drop in collagen synthesis and, at the high dose, in the score on an itch scale. Other liver biochemistry and imaging parameters favored bexotegrast, too, giving Pliant data with enough promise to send its share price up around 15% to $16.60 in premarket trading.
The data set is small—each arm featured around 20 patients—but the signs of efficacy and lack of safety red flags have encouraged Pliant and its investors. Attention now turns to the anticipated publication of 12-week data on a higher, 320-mg dose, which is scheduled for the first quarter of next year.
Pliant is part of a small band of biotechs working to address the unmet need in PSC, a disease that companies including Gilead Sciences have targeted in the past without delivering a FDA-approved treatment. The current crop of companies going after the liver condition includes Chemomab Therapeutics, Dr. Falk Pharma, Escient Pharmaceuticals, HighTide Therapeutics and Mirum Pharmaceuticals.
Phase 2Clinical Result
22 Mar 2023
89bio
said
its drug was better than placebo at lessening fibrosis without worsening nonalcoholic steatohepatitis, or NASH, in two of three dose groups.
The San Francisco biotech said it thinks the Phase IIb data pave the way for a potential Phase III, following in the footsteps of another biotech in its drug class, Akero Therapeutics. To fund a late-stage study, CEO Rohan Palekar told
Endpoints News
89bio “would need to raise additional capital,” with the company having about
$188 million
at the end of last year.
Both 89bio and Akero are making analogs of FGF21 — a hormone normally produced in the liver at low levels to manage energy and lipid metabolism and insulin sensitivity — in the hopes of treating the fatty liver disease. They’re attempting to wade into a disease that has tripped up biopharmas for years but might soon see the first two treatment approvals, with Intercept awaiting an
FDA decision in June
and Madrigal Pharmaceuticals
headed to the regulator next year
. Akero previously said it would
meet with the FDA
this month to discuss a late-stage trial after reading out a positive Phase IIb last September.
For 89bio’s
Enliven study
, 27% of patients receiving the investigational drug pegozafermin at 44mg every two weeks experienced a decrease of at least one stage of fibrosis with no worsening of NASH, the biotech said Wednesday, compared to 7% of those on placebo. For those who got 30mg every week, 26% of patients saw that improvement. Those pegozafermin groups came in at a p-value of 0.008, which the company said was “high statistical significance.” About 22% of the 15mg group saw that improvement, for a p-value of 0.1.
On the other primary endpoint, looking at NASH resolution without a worsening of liver fibrosis, 89bio said 26% of those on the 44mg dose every two weeks met that bar compared to 2% on placebo. The weekly 30mg group saw 23% meet that endpoint, and 37% did so in the weekly 15mg set of patients. P-values were 0.0005 for 44mg, 0.0009 for 30mg and less than 0.0001 for 15mg.
The potential Phase III dosing regimen hasn’t been determined yet, but Palekar said an every-two-week injection is more ideal for patients than a weekly one, especially given the chronic nature of NASH.
The data, with more to be submitted to a medical conference and journal, are likely to draw fine-combing from other NASH drug developers, physicians and investors as the analysis of two primary endpoints came from 192 of 219 patients dosed. The 27-patient difference came after the biotech changed from consulting one pathologist to having three independent pathologists score each liver biopsy slide, which CMO Hank Mansbach called a “much more precise approach” that resulted in those patients no longer meeting the histological inclusion criteria. “Insight from the landscape about how” NASH trials were being conducted led to the adjustment, he said in an interview.
“There is a large variability when a pathologist reads that slide, and in some ways, this has plagued some of the prior studies in NASH,” Palekar said in a separate interview.
The biotech homed in on the prospectively identified population of those with F2 and F3 stages of fibrosis, or liver scarring, which are the “population of interest for regulatory submission,” Mansbach said. Other NASH drug trials have looked at patients with additional stages of fibrosis, but they typically isolate data from the F2 and F3 group, he noted.
On the safety front, 89bio said five patients on pegozafermin versus none on placebo discontinued because of treatment-related adverse events. The biotech said the most frequently reported side effects were grade 1 or 2 diarrhea, nausea or increased appetite at mild to moderate levels. One drug-related serious adverse event occurred in which a patient experienced “uncomplicated pancreatitis associated with gallbladder sludge” after receiving one dose in the 44mg every-two-week group.
Liver fat levels dropped more for patients on 44mg every two weeks and 30mg weekly. 89bio reported 54% and 52% declines for those groups, respectively, versus 14% for the patients on placebo. Liver damage was also lower on the study drug than placebo.
Up next, 89bio plans to meet with regulators in the US and Europe to discuss a Phase III clinical trial, Palekar said. To fund that, the biotech will need more capital, he noted, as current funds are also being directed toward an upcoming Phase III that will test pegozafermin in patients with severe hypertriglyceridemia. The FDA approved the late-stage study after 89bio
presented data last year
on the condition, which can lead to cardiovascular disease.
As 89bio gears up for the next stage, patients and the field await an FDA decision on Intercept’s obeticholic acid. The agency will
convene its outside advisors
on May 19. Mansbach, the 89bio CMO, said a thumbs up from the experts and a subsequent approval for Intercept’s treatment candidate would be “very welcomed certainly by patients as well as by physicians” because it would be the first treatment approved for the indication.
Meanwhile, multiple other biotechs are in the mid-and-late stages of NASH drug development, with Inventiva
working on Phase III studies
of its drug lanifibranor and
HighTide Therapeutics reeling in $107 million
to help support a Phase IIb trial. Chemomab Therapeutics, when presenting Phase IIa results in January,
said it’d focus on other diseases
because of the cash required for running later-stage studies in NASH.
Phase 2Clinical ResultPhase 3Drug Approval
100 Deals associated with HighTide Therapeutics (Hong Kong) Ltd.
Login to view more data
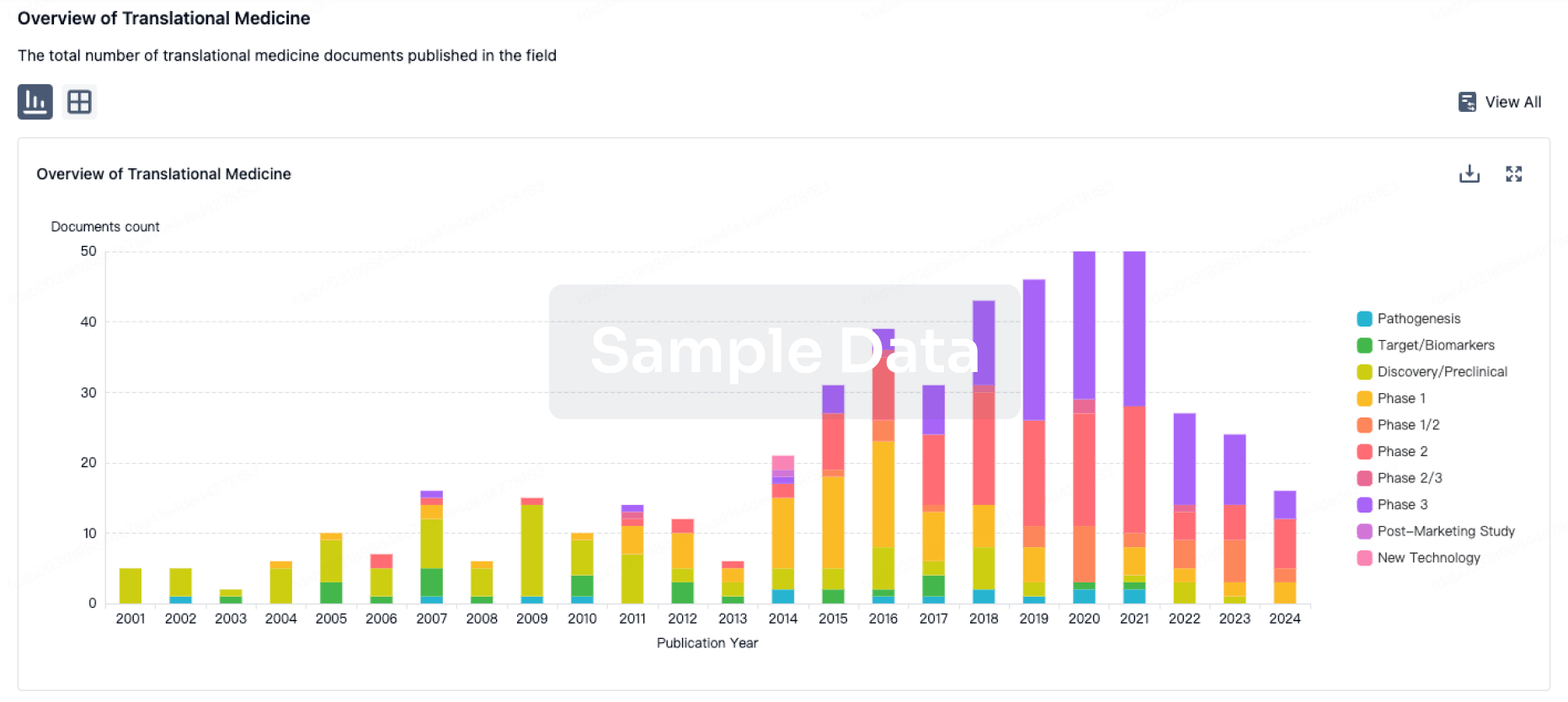
100 Translational Medicine associated with HighTide Therapeutics (Hong Kong) Ltd.
Login to view more data
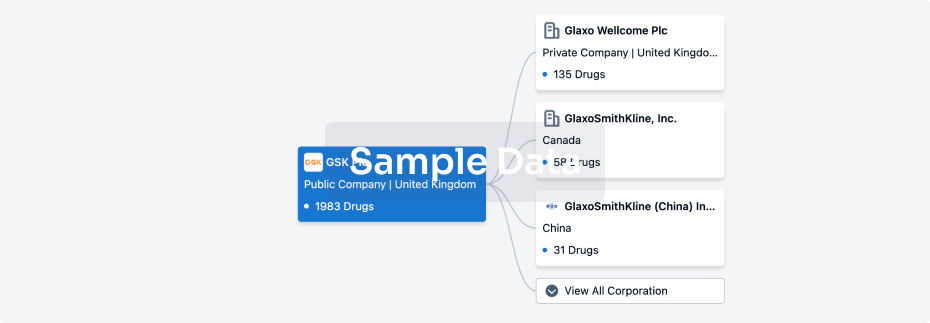
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 11 Dec 2025
The statistics for drugs in the Pipeline is the current organization and its subsidiaries are counted as organizations,Early Phase 1 is incorporated into Phase 1, Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3
Preclinical
4
1
Phase 1 Clinical
Phase 2 Clinical
1
1
Phase 3 Clinical
Other
1
Login to view more data
Current Projects
| Drug(Targets) | Indications | Global Highest Phase |
|---|---|---|
Berberine Ursodeoxycholate ( AMPK x Lipid x NLRP3 ) | Cholangitis, Sclerosing More | Phase 3 |
Rimtoregtide ( NGFB x TLR4 ) | Hepatitis, Alcoholic More | Phase 2 |
HTD-1804 | Obesity More | Phase 1 |
HTF1037 | Obesity More | Preclinical |
HTD-2802 | Inflammatory Bowel Diseases More | Preclinical |
Login to view more data
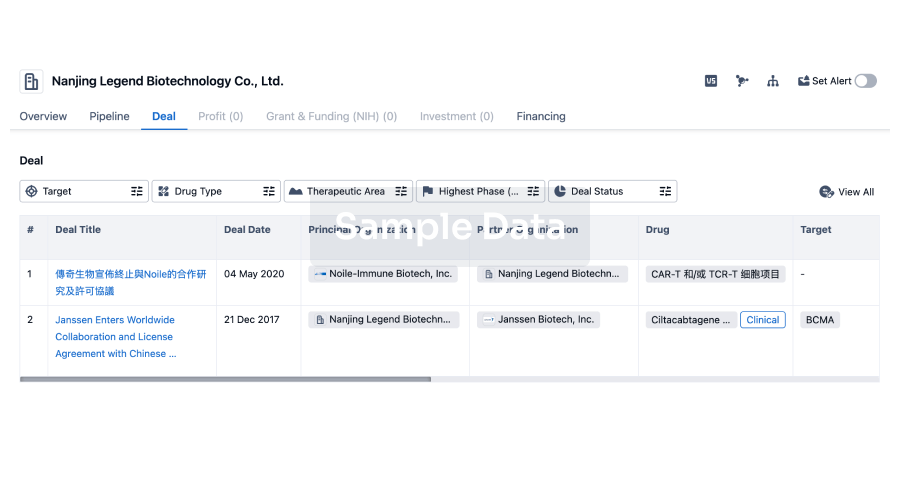
Deal
Boost your decision using our deal data.
login
or
Translational Medicine
Boost your research with our translational medicine data.
login
or
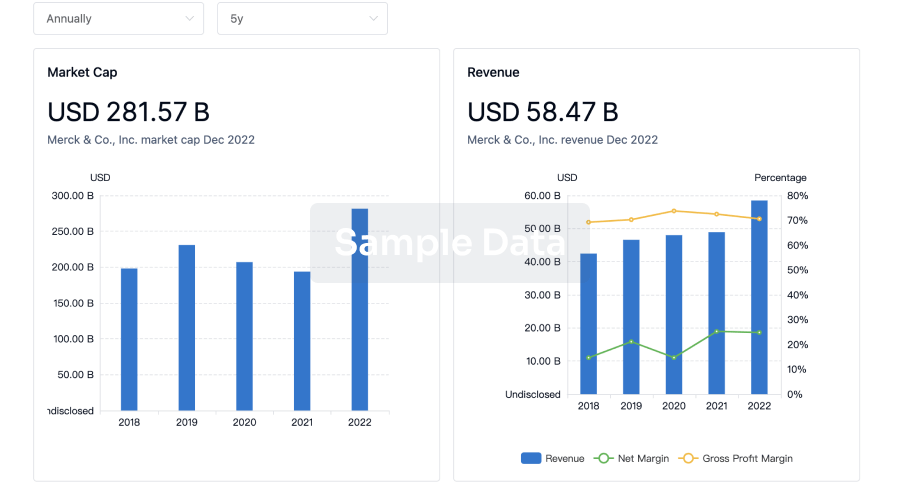
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
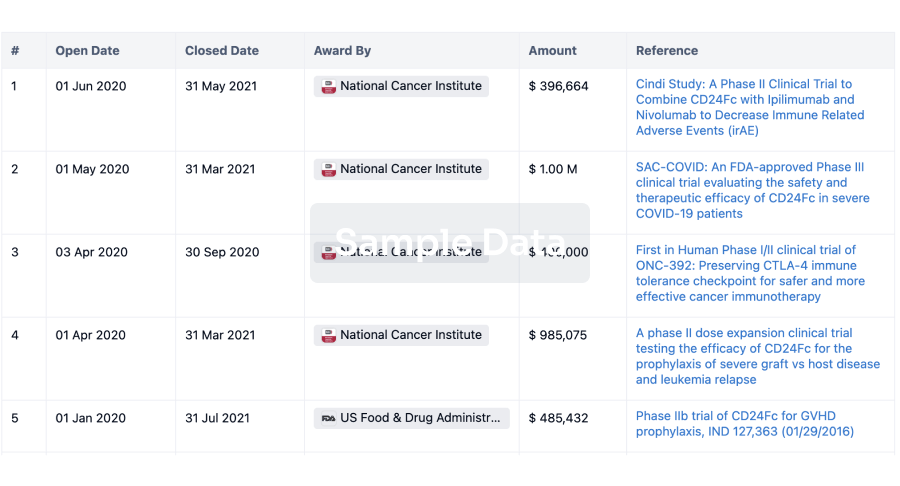
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
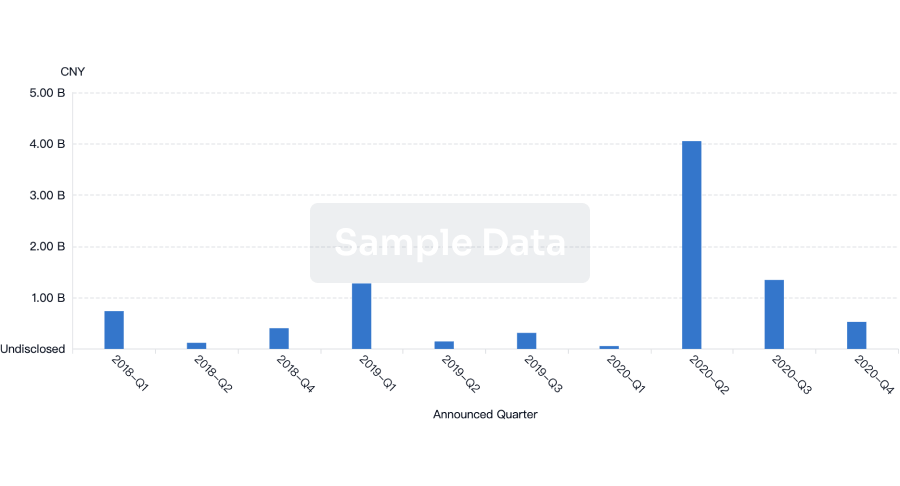
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
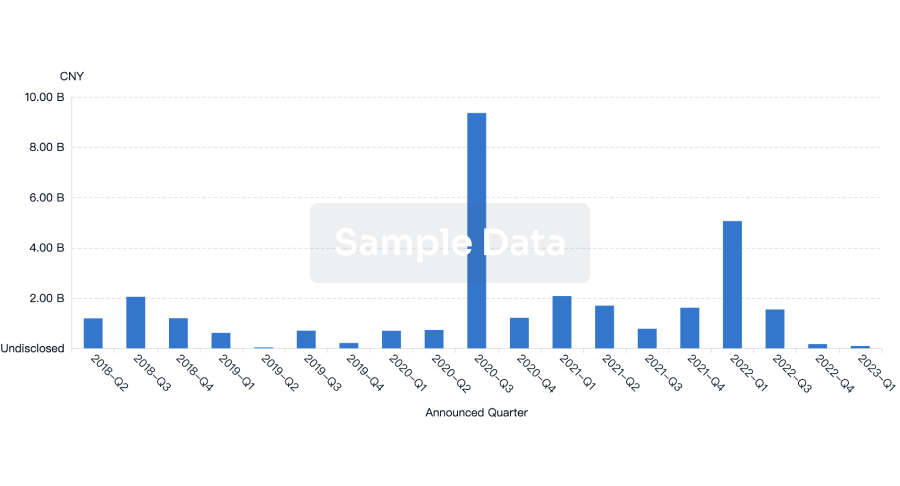
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

