Request Demo
Last update 08 May 2025

ImpriMed, Inc.
Last update 08 May 2025
Overview
Related
100 Clinical Results associated with ImpriMed, Inc.
Login to view more data
0 Patents (Medical) associated with ImpriMed, Inc.
Login to view more data
7
Literatures (Medical) associated with ImpriMed, Inc.11 Mar 2025·Cancer Research
Abstract B002: A study on the relationship between ex vivo drug sensitivity and clinical outcome of acute lymphoblastic leukemia
Author: Yi, Hyoju ; Lee, Seongjun ; Yoon, Jae-Ho ; Park, Sesun ; Park, Sung-Soo ; Lee, Seok ; Koo, Jamin ; Ham, Seunghyok ; Lim, Sungwon
05 Nov 2024·Blood
A Study on the Relationship between Ex Vivo Drug Sensitivity and Clinical Outcome of Acute Lymphoblastic Leukemia
Author: Yoon, Jae-Ho ; Lim, Sungwon ; Koo, Jamin ; Park, Sesun ; Park, Sung-Soo ; Ham, Seunghyeok ; Lee, Seok ; Lee, Seongjoon ; Yi, Hyoju
02 Nov 2023·Blood
Prognostic Utility of the Patient-Derived AML Cells' Ex Vivo Drug Sensitivity Results
Author: Lim, Sungwon ; Park, Sung-Soo ; Song, Edward ; Kim, Heeje ; Park, Silvia ; Lee, Gunjae ; Lee, Junyoung ; Lee, Seongjoon ; Ham, Seunghyeok ; Cho, Byoung Sik ; Koo, Jamin ; Choi, Gyucheol ; Kim, Kwan Hyun ; Park, Sesun
7
News (Medical) associated with ImpriMed, Inc.07 Apr 2025
Biotechnology and precision medicine company Caris Life Sciences announced it raised $168 million in growth capital funding.
Caris Life Sciences has now raised $1.86 billion in capital since 2018.
Braidwell LP led the round with participation from new investors Perceptive Advisors, Woodline and Ghisallo.
Millennium Management and First Light Asset Management also participated in the round.
WHAT IT DOES
Caris is involved in pathology and molecular profiling to diagnose and treat cancerous tissues.
It uses molecular science AI and machine learning algorithms to analyze cancer to help guide physicians in making treatment decisions.
The company will use the money to grow its precision medicine platform and scale its reach.
"This raise will help us bring our market-leading science and technologies to as many patients as possible and further our goal of revolutionizing precision medicine," David Halbert, chairman, founder and CEO of Caris, said in a statement.
"We plan to unlock the full potential of precision medicine by comprehensively interrogating cancer at the molecular level and enabling the delivery of transformative applications of molecular science."
MARKET SNAPSHOT
In 2023, ConcertAI announced it expanded its partnership with Caris Life Sciences. The two companies created a database to generate insights to advance precision medicine, clinical trial management and therapeutic development.
The partners developed a database that leverages both companies' clinical, molecular and multimodal data aimed at allowing academics and biopharma researchers to acquire insights for oncology-focused precision medicine, clinical trial management and therapeutic development.
Other companies involved in precision medicine for cancer include ImpriMed, which in 2024 expanded its services to include human oncology with the aim of providing drug-response predictions for routine blood cancers, such as newly diagnosed multiple myeloma and acute myeloid leukemia.
ImpriMed's human precision medicine services focus on complex blood cancers, using genomic analysis, machine learning and ex vivo drug sensitivity testing.
In 2023, Pfizer announced a multiyear strategic alliance with Tempus to use AI and machine learning to inform drug discovery and development in oncology.
Pfizer uses Tempus' library of de-identified data to increase therapeutic development in oncology. Additionally, it will use Tempus' AI-driven companion diagnostic tools and clinical trial-matching program to bolster therapeutic research and development.
Clinical Study
23 Sep 2024
ImpriMed, a precision medicine company, announced that it has expanded its services to include human oncology.
The aim is to provide drug-response predictions for routine blood cancers such as newly diagnosed multiple myeloma and acute myeloid leukemia.
ImpriMed's human precision medicine services will set their sights on complex blood cancers via a combination of genomic analysis, ex vivo drug sensitivity testing and machine learning.
Data from the company's new research for naive non-Hodgkin lymphoma treatment outcomes will be presented at the EHA-SfPM meeting in Copenhagen, Denmark, September 25-27.
"The expansion of ImpriMed’s precision medicine services from veterinary to human oncology is a pivotal milestone in our mission to transform cancer treatment," Dr. Sungwon Lim, ImpriMed chief executive officer, said in a statement.
"By empowering oncologists and researchers to leverage AI-driven technology to predict treatment outcomes, every patient can receive truly personalized therapy. With our expansion into contract research organization services, we look forward to supporting the development of novel cancer therapies and more personalized treatments, aiming to bring hope to many more patients in their cancer journeys."
THE LARGER TREND
In August, ImpriMed announced the publication of research on a novel cell-sizing method for feline lymphomas in Veterinary Sciences. Data from the research revealed that by improving the precision of cell-size evaluation, ImpriMed’s technique can possibly transform veterinary oncology and give more dependable prognostic insights and improve treatment planning and patient outcomes.
In May, the company launched ImpriMed Drug Response Predictions, an AI service that brings personalized anticancer drug response projections for canine patients with lymphoma or leukemia. DRP is an addendum to the company’s personalized prediction profile, which features an “immunoprofile” report that gives clonality and immunophenotype data.
23 Sep 2024
MOUNTAIN VIEW, Calif.--(
BUSINESS WIRE
)--
EHA-SfPM –
ImpriMed
, a leading functional precision medicine company focused on leveraging artificial intelligence to improve cancer treatment, today announced the expansion of its precision medicine services into human oncology. Building on its success in veterinary oncology, ImpriMed’s pioneering human oncology services will provide drug response predictions for common blood cancers, including newly diagnosed multiple myeloma and acute myeloid leukemia. The company’s transformative new research for naïve non-Hodgkin lymphoma treatment outcomes will be unveiled at the upcoming
EHA-SfPM Precision Medicine Meeting
in Copenhagen, Denmark, from September 25-27, 2024.
ImpriMed Human Oncology Services
Precision medicine enables personalized therapy solutions tailored to each patient’s unique genetic and biological profile, transforming clinical treatment approaches and improving patient outcomes. ImpriMed’s human precision medicine services will focus on complex blood cancers through an innovative combination of genomic analysis, ex vivo drug sensitivity testing, and/or machine learning. Initial services include:
Newly Diagnosed Multiple Myeloma (NDMM)
: ImpriMed’s NDMM software-as-a-medical device utilizes AI and patient data to predict treatment outcomes and the probability of early disease progression without the need for biological samples.
Acute Myeloid Leukemia (AML)
: ImpriMed’s technology evaluates drug sensitivity test results for 21 anticancer drugs, enabling predictions of the patient’s drug responses and survival outcomes to optimize individual treatment plans.
Non-Hodgkin Lymphoma (NHL)
: ImpriMed’s novel approach to tackling NHL runs ex vivo drug sensitivity tests to accurately predict treatment outcomes, facilitating more precise treatment protocols.
EHA-SfPM Precision Medicine Meeting Participation
At EHA-SfPM, ImpriMed CEO Dr. Sungwon Lim will kick off the company’s expansion into human cancer care with a poster presentation titled
"Predicting treatment-specific outcomes for naïve non-Hodgkin lymphoma using ex vivo drug sensitivity analyses."
This groundbreaking study outlines the potential of ex vivo drug sensitivity testing in predicting treatment outcomes and guiding therapeutic decisions for naïve NHL patients, potentially improving survival outcomes.
The presentation marks a significant advancement in ImpriMed’s successful application of machine learning model development for personalized drug response and prognosis predictions and ex vivo drug sensitivity analyses to human cancer care. The company also previously presented the prognostic utility of patient-derived AML cells’ ex vivo drug sensitivity results at the 2023 American Society of Hematology Annual Conference.
“The expansion of ImpriMed’s precision medicine services from veterinary to human oncology is a pivotal milestone in our mission to transform cancer treatment,” said Lim. “By empowering oncologists and researchers to leverage AI-driven technology to predict treatment outcomes, every patient can receive truly personalized therapy. With our expansion into contract research organization services, we look forward to supporting the development of novel cancer therapies and more personalized treatments, aiming to bring hope to many more patients in their cancer journeys.”
ImpriMed is also a proud sponsor of EHA-SfPM alongside other leading pharmaceutical companies. The event, co-organized by the European Hematology Association (EHA) and the Society for Functional Precision Medicine (SfPM), will bring together global experts to discuss the future of predictive diagnostics and drug development for both liquid and solid tumors, underscoring ImpriMed’s commitment to advancing precision medicine in hematological malignancy. The company also plans to broaden its contract research organization (CRO) services, offering pharmaceutical companies access to ImpriMed’s cutting-edge live-cell analysis platform to evaluate the efficacy of new drug compounds on their target patients’ live cancer cells.
Meet with ImpriMed at EHA-SfPM
To schedule an in-person meeting with ImpriMed at EHA-SfPM, interested parties can fill out a meeting request form
here
. For more information about ImpriMed's expansion into human oncology, participation at EHA-SfPM, and CRO services, please visit
www.imprimedicine.com/oncology
.
About ImpriMed
ImpriMed, founded in 2017 in Silicon Valley, is a leading precision medicine startup transforming cancer treatment with artificial intelligence. The company’s pioneering drug response prediction technology helps reduce costs, accelerate treatment, enhance efficacy, and improve the quality of life for patients. To date, the company’s technology has been deployed across more than 40 U.S. states, Canada, England, France, and South Korea, treating 7,500+ canine and feline blood cancer patients as of 2024. ImpriMed is now poised to extend its groundbreaking AI-driven approach to human healthcare, redefining the future of oncology treatment with personalized, effective solutions. For additional information, visit
www.imprimedicine.com
.
ASH
100 Deals associated with ImpriMed, Inc.
Login to view more data
100 Translational Medicine associated with ImpriMed, Inc.
Login to view more data
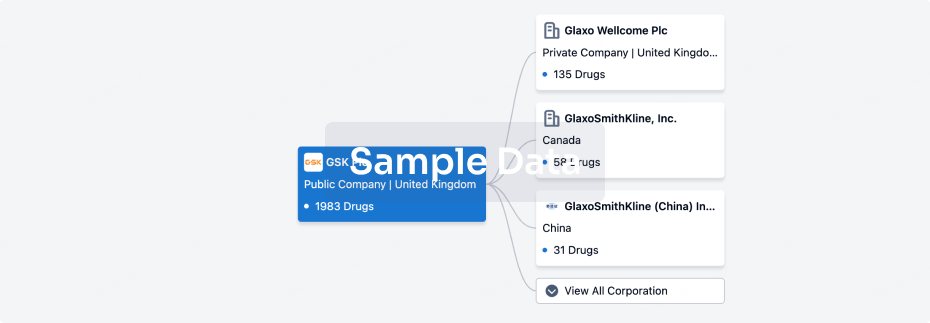
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 20 Aug 2025
No data posted
Login to keep update
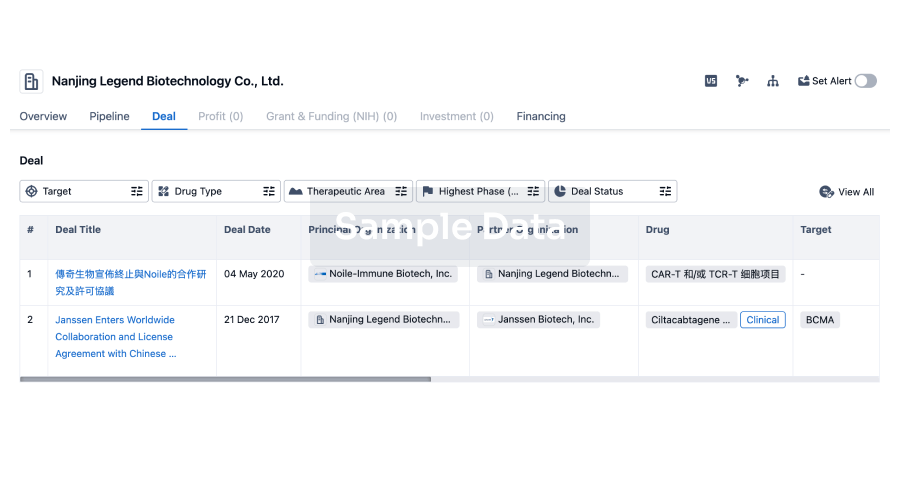
Deal
Boost your decision using our deal data.
login
or
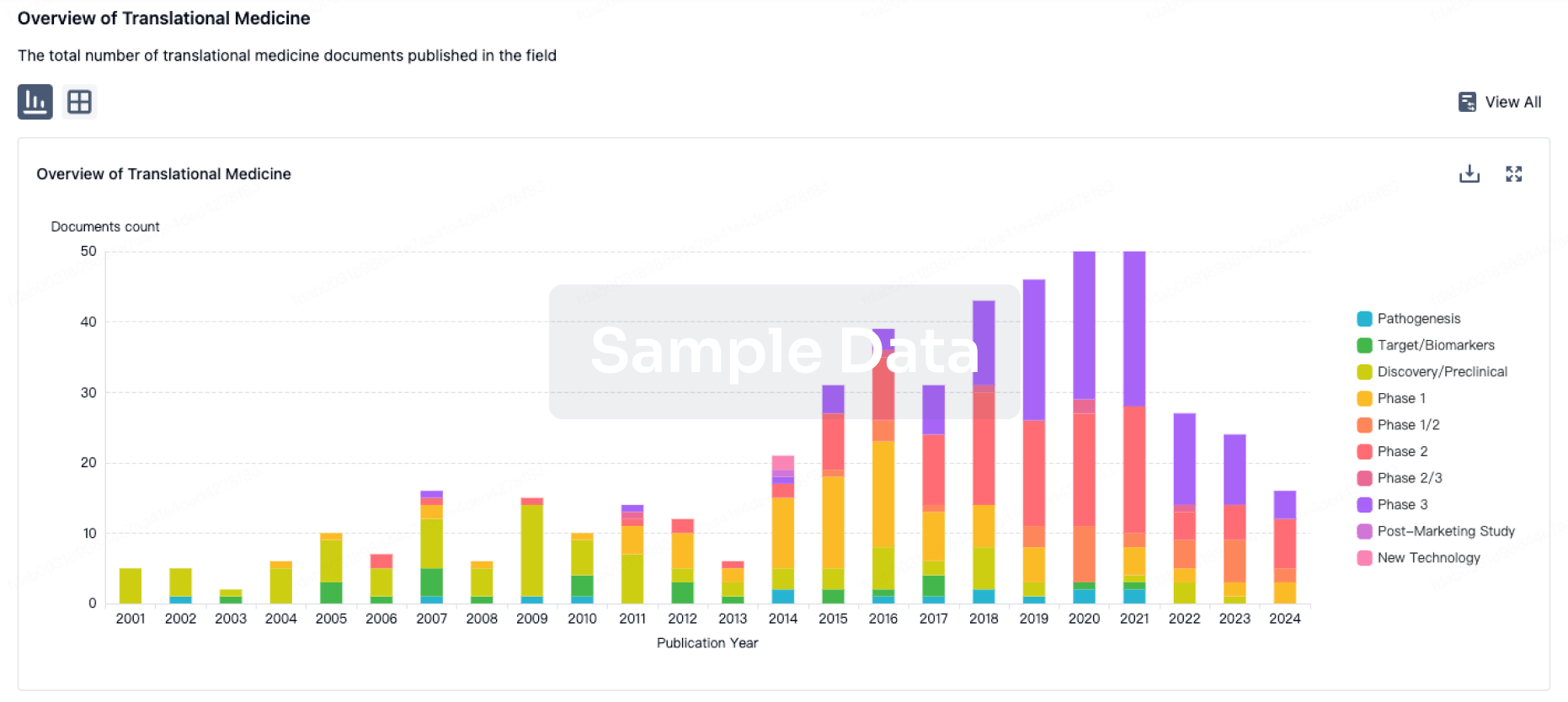
Translational Medicine
Boost your research with our translational medicine data.
login
or
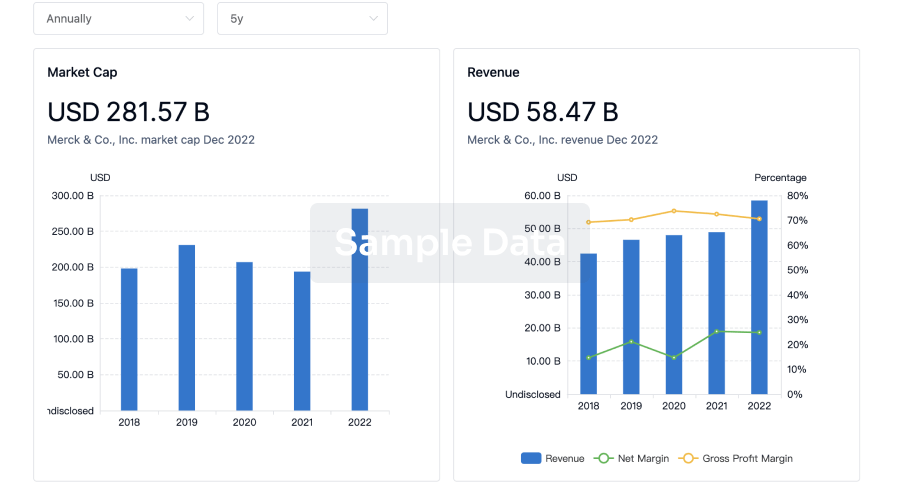
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
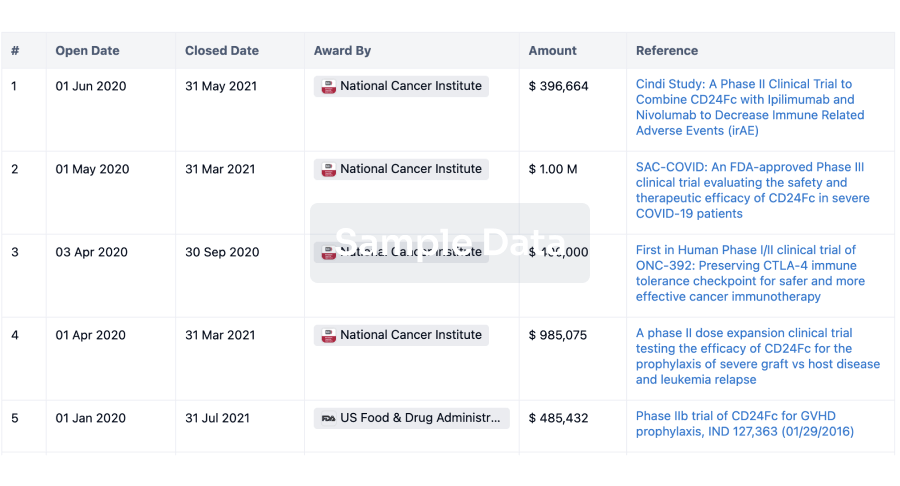
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
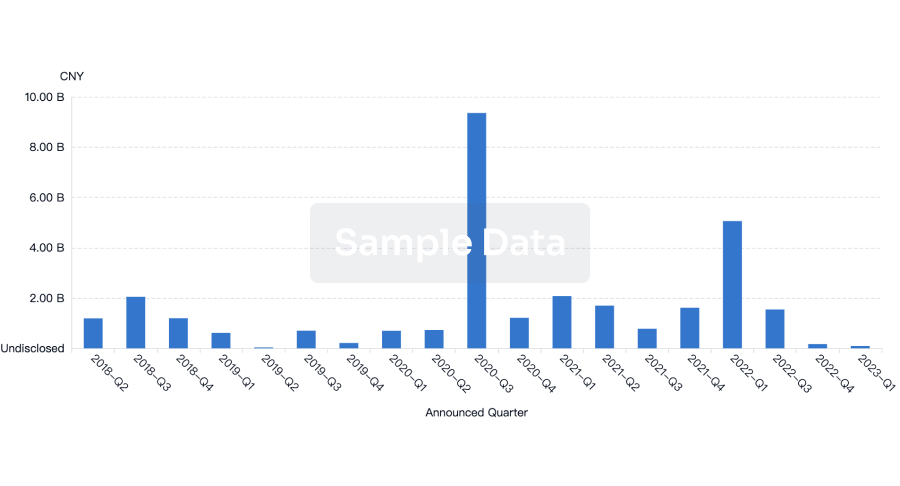
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
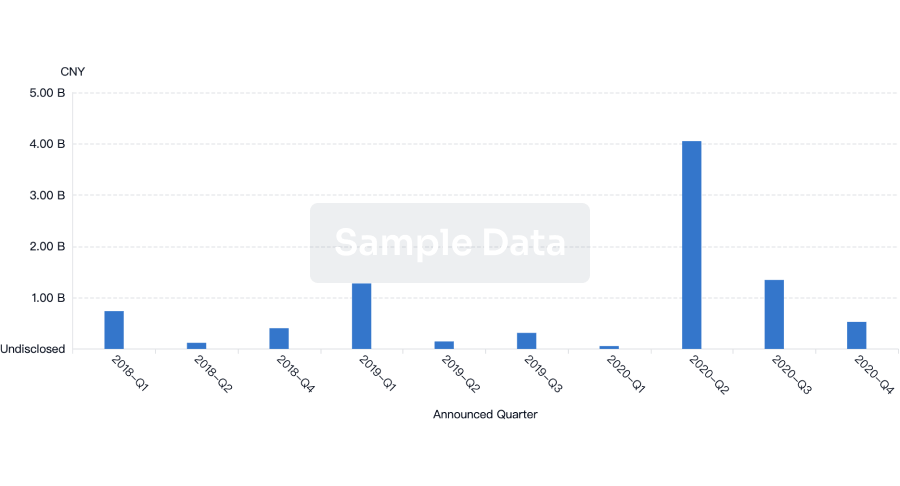
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free