Request Demo
Last update 08 May 2025

Droplet Biosciences, Inc.
Last update 08 May 2025
Overview
Related
100 Clinical Results associated with Droplet Biosciences, Inc.
Login to view more data
0 Patents (Medical) associated with Droplet Biosciences, Inc.
Login to view more data
4
Literatures (Medical) associated with Droplet Biosciences, Inc.21 Apr 2025·Cancer Research
Abstract 1946: Postoperative lymphatic exudate in HPV-negative head and neck cancer detects recurrence prior to adjuvant treatment decisions
Author: Whitfield, Damion ; Winckler, Wendy ; Chaudhuri, Aadel A. ; Pacula, Maciej ; Long, Megan ; Khalil, Lucien ; Lazare, Seka ; Earland, Noah ; Tellis, Ashley ; Francis, Marra ; Harmon, Adam ; Zevallos, Jose P. ; Benson, Adam ; Gu, Zhuosheng ; Ferris, Robert L.
13 Nov 2024·Clinical Cancer Research
Abstract B057: Base-error model (BEM) for improved detection of ctDNA in lymph samples of HPV-negative head and neck cancer patients
Author: Long, Megan ; Zevallos, Jose P. ; Lazare, Seka ; Francis, Marra S. ; Gu, Zhuosheng ; Chaudhuri, Aadel A. ; Winckler, Wendy ; Harmon, Adam ; Pacula, Maciej ; Earland, Noah
01 Apr 2024·Clinical Cancer Research
Sensitive MRD Detection from Lymphatic Fluid after Surgery in HPV-Associated Oropharyngeal Cancer
Article
Author: Hearn, Andrew I. ; Alahi, Irfan ; Chaudhuri, Aadel A. ; Gerndt, Sophie P. ; Chen, Andrew ; Harris, Peter K. ; Ramirez, Ricardo J. ; Zhang, Jin ; Chen, Kevin ; Zevallos, Jose P. ; Whitfield, Damion ; Szymanski, Jeffrey J. ; Inkman, Matthew ; Semenkovich, Nicholas P. ; Gu, Zhuosheng ; Ni, Gabris ; Earland, Noah ; Winckler, Wendy ; Wahle, Benjamin M. ; Xu, Zhongping
2
News (Medical) associated with Droplet Biosciences, Inc.03 Apr 2024
DEL MAR, Calif., April 03, 2024 (GLOBE NEWSWIRE) -- Genece Health, a molecular testing company focused on improving cancer detection for lung, breast, ovarian and other cancers, today announced that Marra Francis, MD, FACOG, has joined the company as its chief medical officer. Dr. Francis is a board-certified Obstetrician and Gynecologist with over 23 years of clinical practice and 18 years of commercial leadership roles across the diagnostics and biotech sectors. She is also currently a member of the MIT Catalyst Faculty. Most recently, Dr. Francis was an advisor to Droplet Biosciences and to Exai Bio, where she built their respective target product profiles ahead of Droplet’s first product launch and Exai’s clinical validation study. At Delphi, she led an early access program for their flagship commercial test. Dr. Francis’ past experience also includes serving as head of medical affairs for women's health of Sema4 (now GeneDx); as executive medical director of EverlyWell; and as chief medical officer of Aspira Women's Health. Earlier in her career, she served as both vice chair and chair of the Department of Obstetrics and Gynecology at Memorial Hermann Hospital of the Woodlands. Dr. Francis holds a medical degree from the University of Connecticut Health Center and a bachelor of arts degree in biology from Occidental College. Dr. Marra Francis named as Genece Health CMO “We are delighted to have Marra join our team at a very exciting time for Genece,” said Greg Gosch, CEO of Genece Heath. “Marra’s clinical expertise in women’s health and oncology will be pivotal in the advancement of our clinical studies and bringing our liquid biopsy and deep-learning AI technology to market. Our goal is to empower physicians with critical insights they need to make informed decisions and improve patient care. Marra will be instrumental in driving key milestones to ultimately help change the way cancer is detected.” About Genece HealthGenece leverages a proprietary liquid biopsy and deep-learning AI technology for early cancer detection. The Company was founded in 2022 through a strategic partnership with GC Genome, the genomics arm of GC Corporation, a leading life sciences company in South Korea. Genece focuses on the acute need for targeted screening and detection tools to support decision-making when a mass or lump is detected through imaging, empowering physicians to make informed decisions and improve care. The Company’s initial applications include high-mortality and women’s health cancers. For more information, visit genecehealth.com or follow Genece on LinkedIn. Investor Contact:investors@genecehealth.com A photo accompanying this announcement is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/7c648163-47e0-4823-b27d-e8426f22ed15
Executive Change
16 Mar 2023
With an $8 million seed investment led by The Engine, Droplet will develop a novel lymph liquid biopsy for earlier, more precise care following surgery.
CAMBRIDGE, Mass.--(BUSINESS WIRE)-- Droplet Biosciences today announced an $8 million seed investment to establish proof of concept for the company’s technology. While the lymphatic system’s critical role in metastasis has long been recognized, routine access to patient lymph has been elusive. Droplet’s foundational breakthrough is a non-invasive process to access lymph through the collection of surgical drain fluid after tumor resection. Rich in T-cells, proteins, and other biomarkers, this lymphatic fluid can offer insights into the body’s immune response to cancer earlier and with greater sensitivity than blood.
This press release features multimedia. View the full release here:
Droplet's Co-founder and CEO Theresa Tribble (L) and Wendy Winckler, PhD, Chief Scientific Officer (Photo: Business Wire)
The first application is detecting residual disease in head and neck cancer patients immediately after surgery. Earlier and more sensitive residual disease detection enables tailored patient-specific follow-up treatment to reduce cancer recurrence. The financing was led by The Engine, the venture firm spun out of MIT that invests in early-stage Tough Tech companies.
Droplet was founded in 2021 by CEO Theresa Tribble and Stan Lapidus, along with scientific co-founders Jose P. Zevallos, MD, MPH, Eugene N. Myers M.D. Chair of Otolaryngology at the University of Pittsburgh and UPMC, and Aadel Chaudhuri, MD, PhD, a leading liquid biopsy researcher and assistant professor of cancer biology, radiation oncology, genetics, computer science, and biomedical engineering at the Washington University in St. Louis. With backgrounds in diagnostics, surgery, oncology, and genomics, the founding team is combining its hands-on patient experience with breakthrough science to unlock the potential of an enriched biofluid.
“Droplet’s mission is to dramatically improve patient outcomes by leveraging the unique and vital features of lymphatic fluid,” said co-founder and CEO Theresa Tribble. “Lymph is a minimally explored scientific frontier that can transform the way we identify recurrence risk. Droplet technology will significantly improve on blood-based monitoring diagnostics by aiding clinicians at the most consequential treatment decision point. Additionally, we see massive potential for the lymphatic data coming out of our research to generate new approaches to patient selection and treatment response.”
Wendy Winckler, PhD, Droplet’s Chief Scientific Officer added, “The lymphatic system is the most common route of metastasis in over 90% of cancer cases. As the most proximal biofluid to a recently resected tumor, the lymph contained in surgical drain fluid offers critical information for assessing metastatic risk at the source of potential spread – before it can travel to other parts of the body. Because Droplet’s test takes place immediately after surgery, the results can aid clinicians in adjuvant treatment decisions, unlike blood-based liquid biopsies that can take weeks or even months to identify recurrence risk.”
“The founders identified a new, important frontier in medicine based on their deep understanding and research into the challenges of treating cancer,” said Ann DeWitt, General Partner at The Engine. “We are thrilled to support this team with an equally impressive track record of bringing transformative diagnostics to market.”
Fueled by increasing cancer rates, advances in sequencing technology, and demand for earlier, non-invasive monitoring across the patient journey, the liquid biopsy market is expected to accelerate significantly over the next decade, with annual growth rates ranging from 12% to 23%. Droplet’s diagnostic approach is differentiated from current products in the liquid biopsy market because it will deliver earlier and more sensitive results compared to existing blood-based assays.
About Droplet Biosciences
Founded in 2021, Cambridge, MA-based Droplet Biosciences harnesses the power of lymphatic fluid to provide earlier and more sensitive cancer diagnostics. For more information, visit .
About The Engine
The Engine, spun out of MIT, invests in early-stage companies solving the world’s biggest problems through a convergence of breakthrough science, engineering, and leadership. We accelerate the path to market for Tough Tech companies through the combination of capital, infrastructure, and network. The Engine is headquartered in Cambridge, MA. For more information, visit .
Diagnostic Reagents
100 Deals associated with Droplet Biosciences, Inc.
Login to view more data
100 Translational Medicine associated with Droplet Biosciences, Inc.
Login to view more data
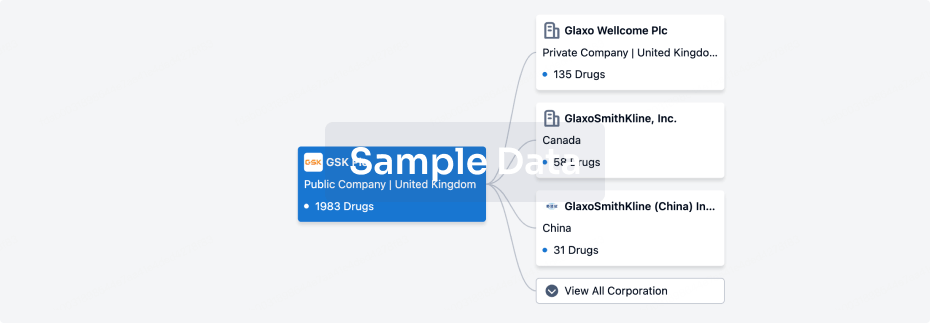
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 13 Sep 2025
No data posted
Login to keep update
Deal
Boost your decision using our deal data.
login
or

Translational Medicine
Boost your research with our translational medicine data.
login
or

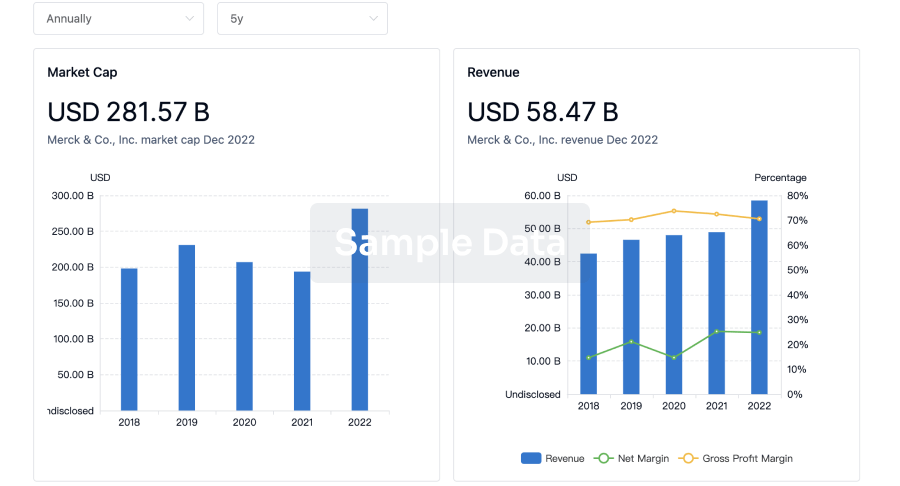
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
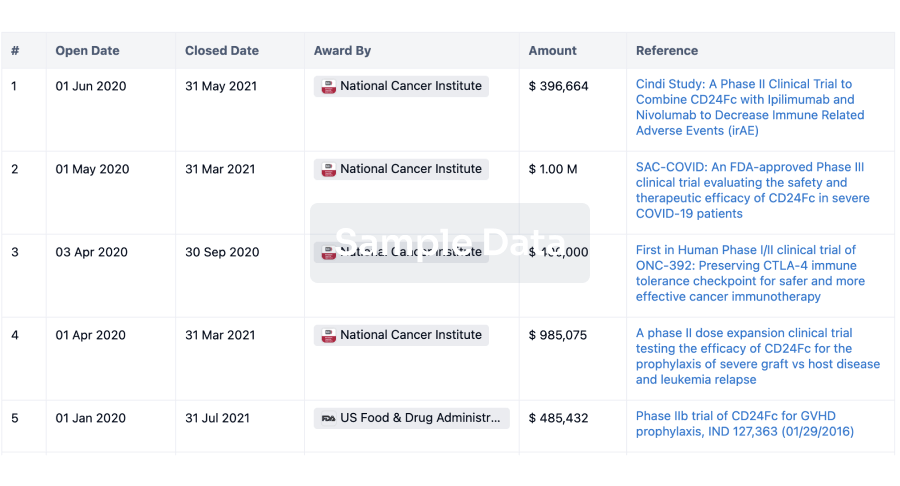
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
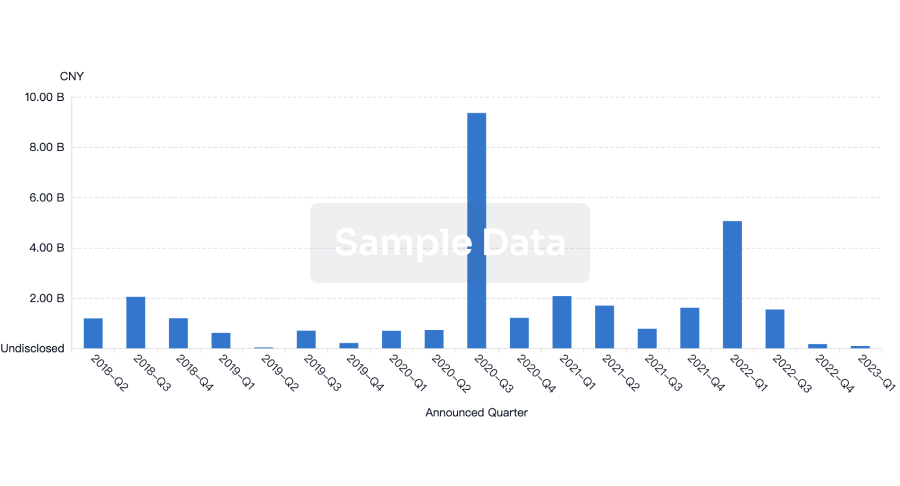
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free