Request Demo
Last update 08 May 2025

Mrc Mitochondrial Biology Unit
Last update 08 May 2025
Overview
Related
1
Clinical Trials associated with Mrc Mitochondrial Biology UnitNCT02469207
A Study Utilising Tissue From Deceased Organ Donors to Investigate Regenerative Cellular Therapies and Related Physiological and Developmental Processes
This study aims to use tissue from deceased organ donors to investigate organ physiology, developmental biology, as well as the development of future regenerative cellular therapies. It will investigate function and immune response to stem cells as well as their generation from adult cells and generation of induced pluripotent stem cells (iPSCs).
Start Date01 Jan 2016 |
Sponsor / Collaborator |
100 Clinical Results associated with Mrc Mitochondrial Biology Unit
Login to view more data
0 Patents (Medical) associated with Mrc Mitochondrial Biology Unit
Login to view more data
351
Literatures (Medical) associated with Mrc Mitochondrial Biology Unit01 Jan 2025·Acta Ophthalmologica
Impact of time to idebenone initiation on visual acuity in leber hereditary optic neuropathy: Post hoc analysis of the leros study
Author: Llòria, Xavier ; Silva, Magda Joana ; Yu‐Wai‐Man, Patrick ; Klopstock, Thomas ; Carelli, Valerio
01 Jan 2025·Acta Ophthalmologica
Changes in visual acuity categories in a historical population of patients with leber hereditary optic neuropathy from case record survey‐2 (CRS‐2)
Author: Lamperti, Costanza ; Krawczynski, Maciej ; Carelli, Valerio ; Leroy, Bart ; Yu‐Wai‐Man, Patrick ; Llòria, Xavier ; van Everdingen, Judith ; Klopstock, Thomas
01 Jan 2025·Acta Ophthalmologica
Visual acuity outcomes by causative mutation in the natural history of leber hereditary optic neuropathy: Analysis of historical data from Case Record Survey‐2 (CRS‐2)
Author: Klopstock, Thomas ; Yu‐Wai‐Man, Patrick ; Krawczynski, Maciej ; van Everdingen, Judith ; Llòria, Xavier ; Lamperti, Costanza ; Carelli, Valerio ; Leroy, Bart
1
News (Medical) associated with Mrc Mitochondrial Biology Unit08 Mar 2023
Scientists have made an important breakthrough in understanding what goes wrong in our bodies during the progression of inflammatory diseases and -- in doing so -- unearthed a potential new therapeutic target. The scientists have found that an enzyme called fumarate hydratase is repressed in macrophages, a frontline inflammatory cell type implicated in a range of diseases including lupus, arthritis, sepsis and COVID-19.
Scientists working in the School of Biochemistry and Immunology in the Trinity Biomedical Sciences Institute at Trinity College Dublin have made an important breakthrough in understanding what goes wrong in our bodies during the progression of inflammatory diseases and -- in doing so -- unearthed a potential new therapeutic target.
The scientists have found that an enzyme called Fumarate Hydratase is repressed in macrophages, a frontline inflammatory cell type implicated in a range of diseases including Lupus, Arthritis, Sepsis and COVID-19.
Professor Luke O'Neill, Professor of Biochemistry at Trinity is the lead author of the research article that has just been published in leading international journal, Nature. He said:
"No-one has made a link from Fumarate Hydratase to inflammatory macrophages before and we feel that this process might be targetable to treat debilitating diseases like Lupus, which is a nasty autoimmune disease that damages several parts of the body including the skin, kidneys and joints."
Joint first-author Christian Peace added:
"We have made an important link between Fumarate Hydratase and immune proteins called cytokines that mediate inflammatory diseases. We found that when Fumarate Hydratase is repressed, RNA is released from mitochondria which can bind to key proteins 'MDA5' and 'TLR7' and trigger the release of cytokines, thereby worsening inflammation. This process could potentially be targeted therapeutically."
Fumarate Hydratase was shown to be repressed in a model of sepsis, an often-fatal systemic inflammatory condition that can happen during bacterial and viral infections. Similarly, in blood samples from patients with Lupus, Fumarate Hydratase was dramatically decreased.
"Restoring Fumarate Hydratase in these diseases or targeting MDA5 or TLR7 therefore presents an exciting prospect for badly needed new anti-inflammatory therapies," said Prof O'Neill.
Excitingly, this newly published work is accompanied by another publication by a group led by Professor Christian Frezza, now at the University of Cologne, and Dr Julien Prudent at the MRC Mitochondrial Biology Unit (MBU), who have made similar findings in the context of kidney cancer.
"Because the system can go wrong in certain types of cancer, the scope of any potential therapeutic target could be widened beyond inflammation," added Prof O'Neill.
The Trinity study is a collaboration between eight universities including the MRC MBU, University of Cambridge where Dr Dylan Ryan is co-first author along with Dr Alex Hooftman, who is now based at the Swiss Federal Institute of Technology Lausanne. Cedars Sinai Medical Centre in Los Angeles is another key collaborator helping with the study of Lupus patients.
The study was supported with funding from the European Research Council, Medical Research Council and Science Foundation Ireland. Work in the Frezza lab is also supported by the ERC, further illustrating the importance of ERC funding for EU science.
100 Deals associated with Mrc Mitochondrial Biology Unit
Login to view more data
100 Translational Medicine associated with Mrc Mitochondrial Biology Unit
Login to view more data
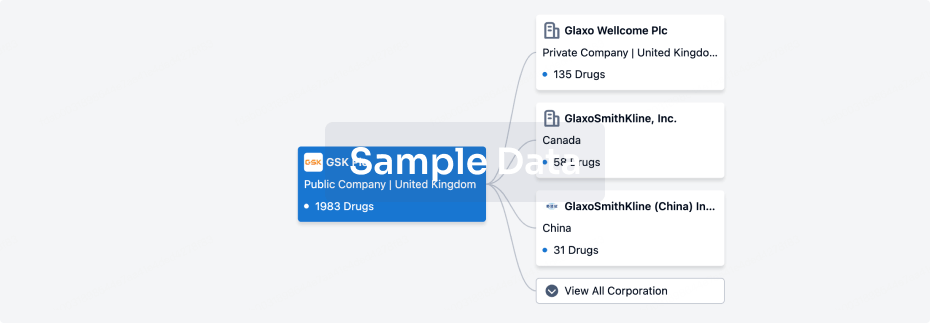
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 19 Oct 2025
No data posted
Login to keep update
Deal
Boost your decision using our deal data.
login
or

Translational Medicine
Boost your research with our translational medicine data.
login
or

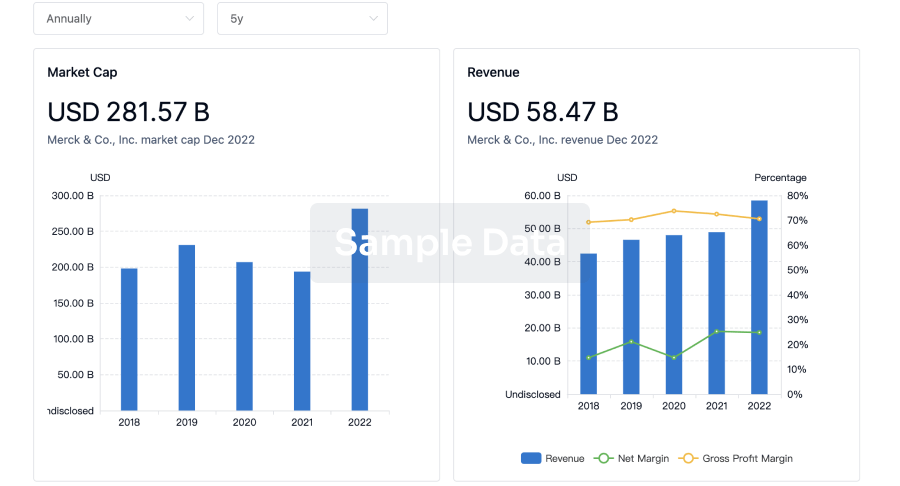
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
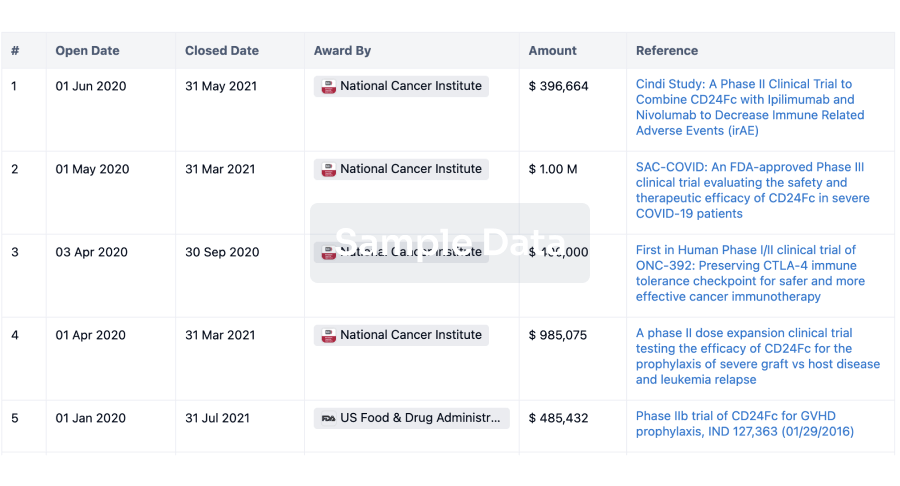
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
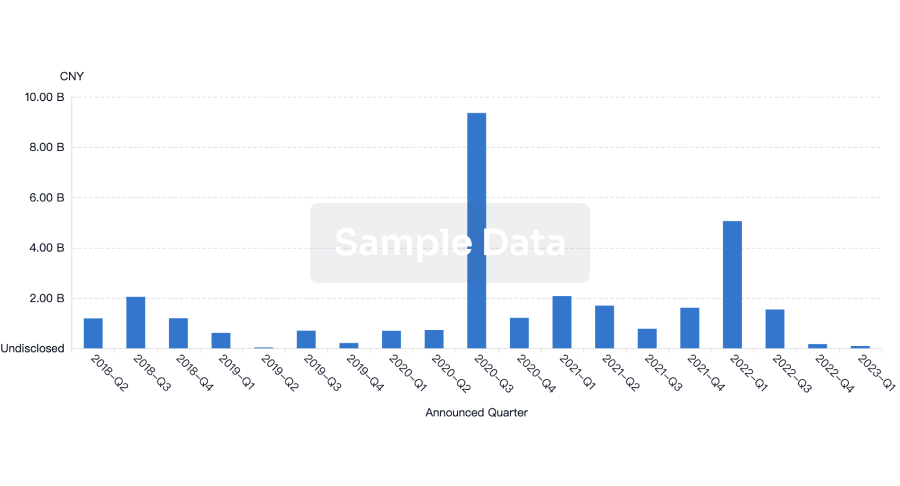
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
