Request Demo
Last update 29 Aug 2025

University of Massachusetts Dartmouth
Last update 29 Aug 2025
Overview
Related
100 Clinical Results associated with University of Massachusetts Dartmouth
Login to view more data
0 Patents (Medical) associated with University of Massachusetts Dartmouth
Login to view more data
4,933
Literatures (Medical) associated with University of Massachusetts Dartmouth01 Nov 2025·BONE
Effect of type 1 and type 2 diabetes on human femoral trabecular bone composition, microarchitecture, and mechanical behavior
Article
Author: Karim, Lamya ; Yu, Marc Gregory ; Bouxsein, Mary L ; Behzad, Ramina ; Wu, I-Hsien ; Johannesdottir, Fjola ; Yu, Elaine W ; Emerzian, Shannon R ; King, George L ; Unal, Mustafa ; Brooks, Daniel J ; Gauthier, John ; Jangolla, Surya ; Hanlon, Jackson ; Shah, Hetal S
Both type 1 diabetes (T1D) and type 2 diabetes (T2D) increase hip fracture risk beyond what bone mineral density (BMD) explains, potentially due to changes in bone material from advanced glycation end-products (AGEs) and altered matrix composition. However, there are limited data regarding the impact of diabetes on human trabecular bone composition and mechanical behavior. We assessed trabecular bone material behavior using cadaveric femoral specimens from older adults with long-duration T1D (≥50 years; n = 24), T2D (n = 21), and non-diabetic controls (n = 21). Femoral head trabecular bone was evaluated via micro-computed tomography, mechanical testing (uniaxial compression), total fluorescent AGEs quantification, and Raman spectroscopy (matrix composition). BMD and microarchitecture measures did not differ between groups (p > 0.535). Compared to controls, T1D trabecular bone had higher AGE content (+42 %, p = 0.016), lower mineral-to-matrix ratio (-12 %, p = 0.048), trend toward lower crystallinity (-4 %, p = 0.054), and greater proline hydroxylation (+5 %, p = 0.007), but showed no differences in mechanical behavior (p ≥ 0.415). T2D trabecular bone also had elevated AGE (+60 %, p < 0.001) and altered matrix composition. Unlike T1D, T2D bone demonstrated improved ductility and post-yield energy dissipation versus control, with greater ultimate strain (+36 %, p = 0.008), post-yield strain (+62 %, p = 0.075), and toughness to ultimate force (+38 %, p = 0.044). This study reveals distinct effects of T1D and T2D on trabecular bone matrix composition, although these effects did not coincide with reduced mechanical properties under uniaxial compression loading.
01 Sep 2025·NURSING OUTLOOK
Impact of minority stress and resilience on post-traumatic stress disorder symptom severity among a sample of transgender, nonbinary, and gender-expansive individuals
Article
Author: Hernandez, Stephen ; Parshall, Mark ; Deutsch, Madeline B ; Jackson, Kristopher ; Tomlinson, Starr ; Hung, Erick K ; Ruyak, Sharon
BACKGROUND:
Transgender, nonbinary, and gender-expansive (TNGE) individuals experience disproportionately high levels of discrimination and violence. These chronic stressors can disrupt stress responses and increase vulnerability to negative mental health outcomes.
PURPOSE:
The purpose of this research was to explore the impact of gender minority stress and resilience on post-traumatic stress disorder (PTSD) symptom severity among TNGE individuals receiving outpatient medical or psychiatric care.
METHODS:
Individuals (N = 103) receiving gender-affirming healthcare services at one of two university-affiliated practice settings completed an anonymous survey measuring PTSD symptom severity and gender minority stress and resilience.
RESULTS:
One-third of participants met provisional criteria for PTSD. No significant differences in PTSD symptoms were found based on assigned sex at birth, current gender identity, marital status, sexual orientation, or race/ethnicity. Distal stressor subscales accounted for approximately 40% of variance in PTSD symptom severity in a hierarchical regression model. Proximal stressors and resilience subscales accounted for an additional 7% and 3% of variance, respectively.
DISCUSSION:
TNGE individuals' experiences of gender minority stress, especially distal stressors, may constitute risk factors for PTSD. Interventions to foster community engagement may offer valuable mental health benefits for TNGE persons.
01 Sep 2025·Nursing Education Perspectives
Nursing Preceptor Development Using a Mobile Application
Article
Author: Ross, Jennifer Gunberg ; Dunker, Kimberly ; Duprey, Melissa ; Parson, Tracy
Abstract:
Mobile technologies can be used to engage learners in a dynamic way. Many nursing preceptors are not adequately prepared for clinical teaching. The purpose of this project was to implement mobile learning technology for clinical preceptor development. Preceptors working one-on-one with senior nursing students in their final clinical practicum course received weekly information through the Remind© application, including reminders, supplemental resources, course updates, and encouragement to engage preceptors in developing competency in the clinical educator role. Preceptors’ reaction to the continuing education offering was positive. Research is needed to evaluate the effects of mobile technology on preceptors’ competence.
2
News (Medical) associated with University of Massachusetts Dartmouth15 May 2025
Duchemin brings global MedTech leadership experience to accelerate Fotona's next phase of growth
DALLAS , May 15, 2025 /PRNewswire/ -- Fotona
Ⓡ, a global leader in high-performing laser systems and energy-based devices for aesthetic, dental and gynecological applications, today announces the appointment of Jeff Duchemin as Group President and CEO.
Continue Reading
Jeff Duchemin, CEO Fotona
Duchemin brings decades of leadership experience in the global medical technology sector, having held senior roles in both U.S. and international markets. Most recently, he served in executive roles in the Interventional Surgery and Integrated Diagnostic Solutions business at Becton Dickinson along with being the former President and CEO of Harvard Biosciences. His expertise in driving revenue growth—both organically and through strategic acquisitions—will play a critical role in advancing Fotona's innovation and expanding its presence globally. Duchemin holds an M.B.A from Southern New Hampshire University and a B.S. in Accounting from the University of Massachusetts Dartmouth.
"Jeff is a visionary leader with a strong track record of driving global success in the life sciences and medical device industries," said Jay Katzen, Executive Chairman, Fotona. "We are excited to have him join Fotona, which has industry leading experts and solutions, to lead Fotona through its next chapter of innovation and market leadership."
"Innovation is at the heart of Fotona," said Duchemin. "I'm passionate about accelerating growth by enhancing our current solutions and introducing breakthrough technologies. Fotona has a solid foundation, exceptional talent, and world-class products. It's an honor to lead the company at such a pivotal time in its journey."
Last year, Fotona proudly marked 60 years of innovation in laser technology. Throughout its history, the company has been at the forefront of industry advancements, including the groundbreaking integration of dual laser wavelengths (Er:YAG and Nd:YAG) within a single system. Most recently, Fotona launched the Dynamis® Max, its next-generation aesthetic platform offering expanded versatility, improved usability, and enhanced treatment efficiency—supporting more than 100 advanced treatment applications.
For more information, visit Fotona.com.
About Fotona
Fotona is a world-leading medical laser company recognized for its innovative, award-winning laser systems for applications in aesthetics & dermatology, dentistry, surgery and gynecology. The company has one of the most highly educated workforces in the industry, with an exceptionally high number of PhDs specializing in laser and medical technology innovation. In addition to its direct presence in the US, China, Japan and the EU, Fotona's global distribution network spans across more than 70 countries, ensuring comprehensive support and service for Fotona laser users, including clinical training.
SOURCE Fotona
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
Executive Change
22 Jun 2021
June 22, 2021 13:00 UTC
Engineering and Technology Veteran to Lead Company’s Product Vision and Support Growing Demand for Insulin Dosing Software and Inpatient Glycemic Management
WALTHAM, Mass.--(BUSINESS WIRE)-- Glytec LLC, the only provider of cloud-based insulin management software across the continuum of care, today announced the appointment of Nausheen Moulana as Chief Technology Officer. In this role, Moulana will be responsible for the company’s product and technology vision, strategy and execution.
A highly accomplished technologist in the healthcare, enterprise technology and scientific computing sectors, Moulana brings over 25 years of engineering and operations experience to Glytec. She possesses a deep understanding of developing complex software products and driving process improvement to maximize customer value.
Moulana comes to Glytec from Kyruus, the leader in provider search and scheduling solutions for health systems, where she served as Vice President of Engineering & Operations and led multiple teams tasked with delivering multi-channel patient access solutions. She also previously held leadership positions at Attivio (since acquired by ServiceNow) and MathWorks.
“Thousands of hospitals across the country still rely on dated paper protocols to titrate insulin and manage inpatient blood glucose levels. The opportunity for advanced software to simplify these processes and improve patient safety and care is massive,” said Moulana. “I’m honored to join the growing team at Glytec to address this challenge and further revolutionize the way providers care for patients that require insulin in the hospital setting.”
In April 2021, Glytec closed a $21 million funding round to put significant resources behind accelerating research and product development and scaling into hospitals across the United States. In her new role, Moulana will lead the teams responsible for creating the innovations that continue to strengthen Glytec’s position as the industry leader in insulin management and patient safety. The Product Development teams will focus on enhancements in provider workflows, EHR integrations, mobile apps at scale and support for other diabetes technology across the continuum of care.
“This has been a record year for Glytec and adding a proven technology leader like Nausheen to the Executive team only builds upon that momentum,” said Ed Furlong, President and Chief Executive Officer, Glytec. “The past year has illuminated the importance of properly managing glycemic issues, especially in the hospital setting. Nausheen will help us meet the growing demand for eGlycemic Management System, enabling Glytec to remain the industry leader for inpatient glycemic management.”
Moulana holds a Master of Science in Electrical Engineering from the University of Massachusetts Dartmouth and a Master of Business Administration from Babson College. Known for her mentorship approach to leadership and advocacy for diversity, equity and inclusion, Moulana is also a startup advisor, speaker and host for several technical and talent events.
To learn more about Glytec, visit: .
About Glytec
Glytec is the insulin management software company for healthcare providers focused on improving the quality and cost of care. Its FDA-cleared titration software and proprietary algorithms power the only solution capable of delivering personalized diabetes treatment recommendations across the continuum of care, from hospital to home. With ongoing support from its team of doctors, nurses and technologists headquartered outside of Boston, Glytec improves outcomes and controls costs for the large population of patients requiring insulin treatment – including those with and without a diagnosis of diabetes. For more information, follow Glytec on Twitter (@Glytec) and LinkedIn, or visit .
MAR-0000344 Rev. 1.0
100 Deals associated with University of Massachusetts Dartmouth
Login to view more data
100 Translational Medicine associated with University of Massachusetts Dartmouth
Login to view more data
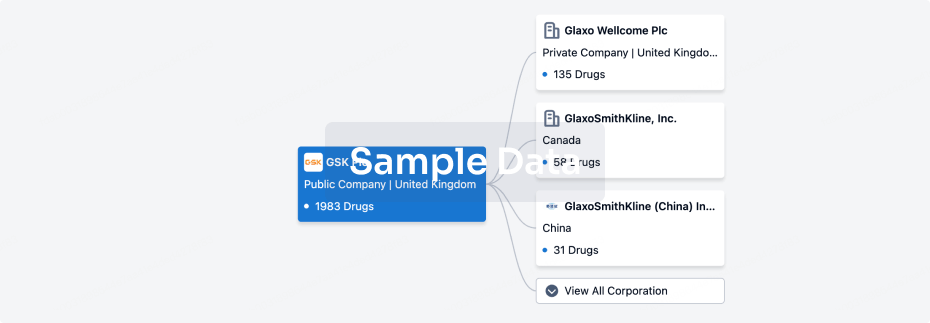
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 01 Sep 2025
No data posted
Login to keep update
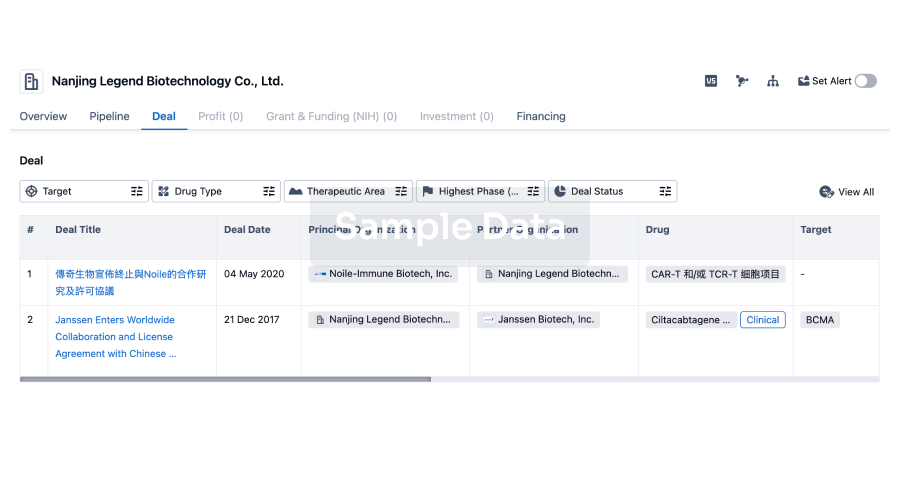
Deal
Boost your decision using our deal data.
login
or
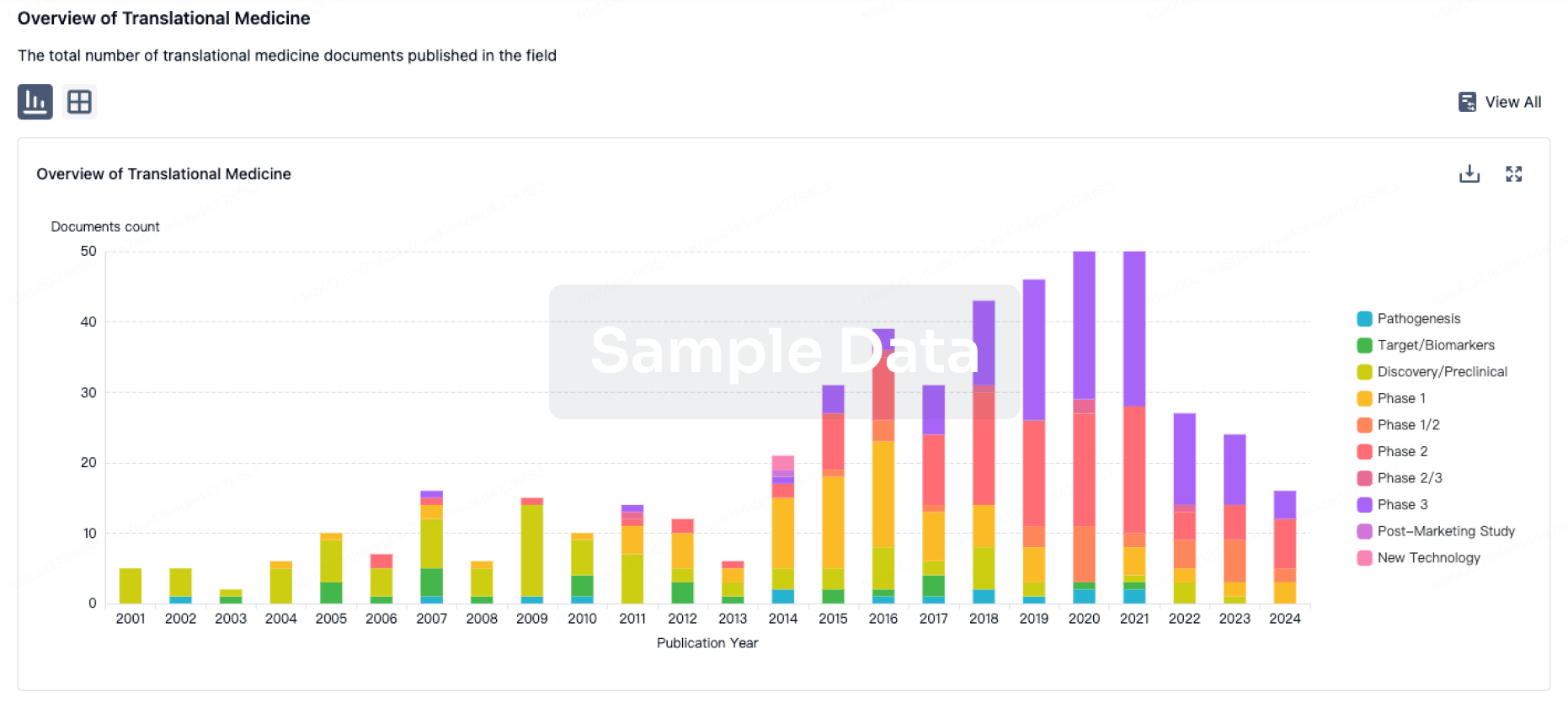
Translational Medicine
Boost your research with our translational medicine data.
login
or
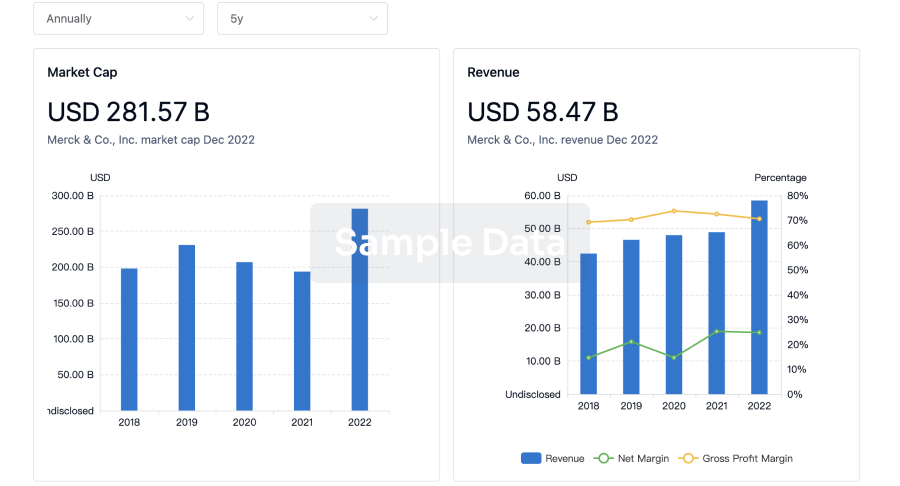
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
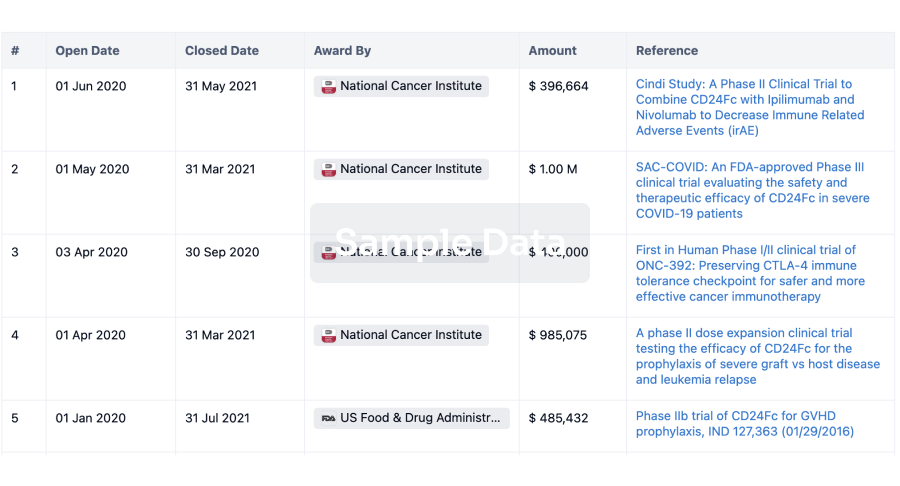
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
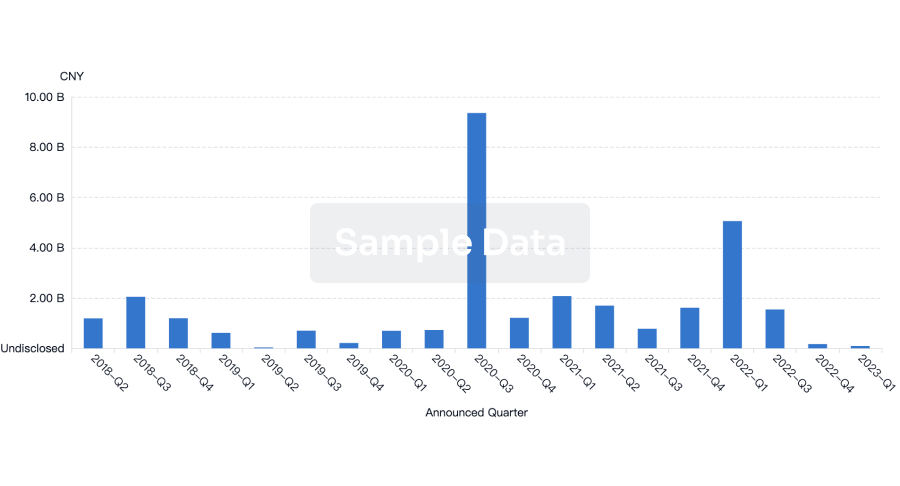
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
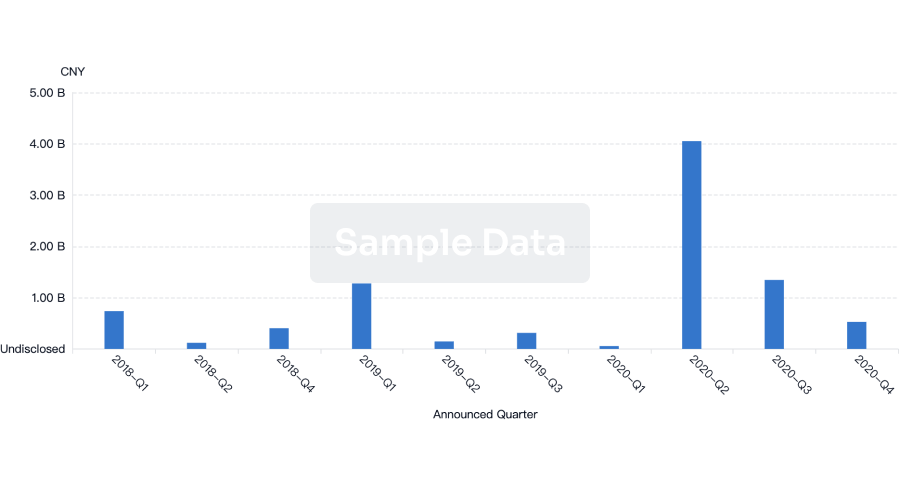
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free