Request Demo
Last update 28 Sep 2024
Amiloride sensitive sodium channel
Last update 28 Sep 2024
Basic Info
Related Targets |
Related
2
Drugs associated with Amiloride sensitive sodium channelMechanism Amiloride sensitive sodium channel inhibitors |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePhase 2 |
First Approval Ctry. / Loc.- |
First Approval Date- |
Mechanism Amiloride sensitive sodium channel inhibitors |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date- |
5
Clinical Trials associated with Amiloride sensitive sodium channelNCT06478706
A Randomised, Double-Blind, Placebo Controlled, Two-Part Study to Evaluate the Efficacy, Safety, Tolerability and Pharmacokinetics of a Repeat Dose of Inhaled ETD001 in People With Cystic Fibrosis
This study is the first to give ETD001 to people with CF. The study will be run in two parts. Part A will assess if ETD001 is safe to give to people with CF, and Part B will assess if ETD001 improves lung function. The study drug is taken twice a day, in Part A it is taken for 7 days and in Part B for 28 days. In Part B there will be a separate period where dummy medicine is given for 28 days so the treatments can be compared.
In Part A participants will receive 13 doses of either ETD001 or placebo, 8 people will take part. Participants will take up to 56 days to finish the study and make 5 outpatient visits.
In Part B participants will receive 55 doses of ETD001 and 55 doses of placebo, 32 people will take part. Participants will take up to 140 days to finish the study and will make 8 outpatient visits.
Study assessments include physical examinations, vital signs, heart traces, blood/urine samples, breathing tests and health questionnaires.
In Part A participants will receive 13 doses of either ETD001 or placebo, 8 people will take part. Participants will take up to 56 days to finish the study and make 5 outpatient visits.
In Part B participants will receive 55 doses of ETD001 and 55 doses of placebo, 32 people will take part. Participants will take up to 140 days to finish the study and will make 8 outpatient visits.
Study assessments include physical examinations, vital signs, heart traces, blood/urine samples, breathing tests and health questionnaires.
Start Date26 Jun 2024 |
Sponsor / Collaborator |
CTIS2023-504092-25-00
A Randomised, Double-Blind, Placebo Controlled, Two-Part Study to Evaluate the Efficacy, Safety, Tolerability and Pharmacokinetics of a Repeat Dose of Inhaled ETD001 in People with Cystic Fibrosis - ET-ENAC-03
Start Date26 Jun 2024 |
Sponsor / Collaborator |
NCT04926701
A First in Human Randomised, Double Blind, Placebo-controlled, Two-part Study to Evaluate the Safety, Tolerability and Pharmacokinetics of Single and Multiple Ascending Doses (SAD and MAD) of Inhaled ETD001 in Healthy Male and Female Subjects
This is a first in human study of ETD001 a new drug being developed for the treatment of cystic fibrosis. The study is a randomised, placebo-controlled, double-blind interventional study to assess the safety, tolerability and pharmacokinetics of single and multiple ascending doses of inhaled ETD001in healthy male and female subjects.
Start Date11 Jun 2021 |
Sponsor / Collaborator |
100 Clinical Results associated with Amiloride sensitive sodium channel
Login to view more data
100 Translational Medicine associated with Amiloride sensitive sodium channel
Login to view more data
0 Patents (Medical) associated with Amiloride sensitive sodium channel
Login to view more data
112
Literatures (Medical) associated with Amiloride sensitive sodium channel01 Nov 2023·Journal of the European Academy of Dermatology and Venereology : JEADV
Detection of a knockdown mutation in the voltage-sensitive sodium channel associated with permethrin tolerance in Sarcoptes scabiei var. hominis mites.
Article
Author: Walochnik, J ; Weber, P B ; Urban, N ; Purkhauser, K ; Handisurya, A ; Riebenbauer, K ; Stamm, T
BACKGROUND:
Increasing evidence has sparked a debate on the loss of sensitivity of scabies mites to conventional permethrin therapy. Mutations in the voltage-sensitive sodium channels (VSSC) were associated with knockdown resistance (kdr) in many arthropods, but have never been identified in Sarcoptes scabiei variatio (var.) hominis mites.
OBJECTIVES:
To identify factors contributing to therapy failure.
METHODS:
Sixty-seven mites were collected from 64 scabies-infested patients in Vienna, Austria, of whom 85.9% were refractory to prior permethrin-based treatments, and genotyped for the presence of nucleotide polymorphisms in Domain II of the VSSC, known to be associated with kdr. Information regarding previous antiscabietic therapies, decontamination procedures and possible re-infestations by contacts as well as the response to re-imposed therapies were obtained.
RESULTS:
Sequence alignment comparisons revealed previously unidentified mutations in the coding region of Domain II of the VSSC. A novel A1663T transversion was detected in 97.0% of the mites, resulting in a non-synonymous substitution from methionine to leucine, M918L, a mutation known to confer kdr in other arthropods. In addition, a synonymous G1659A transition was identified in one mite, which otherwise showed a nucleotide sequence identical to the wild-type reference. No major inconsistencies were observed within the previous therapeutic and decontamination procedures, which could have accounted for the observed non-responsiveness to permethrin-based therapies. Subsequent cure of infestation was achieved in 65.6% of the participants, predominantly by combination therapies with topical permethrin and systemic ivermectin. However, in 14.6% of the cured cases, permethrin monotherapy sufficed for eradication of scabies, albeit in some cases prolonged exposure was necessary.
CONCLUSIONS:
The kdr-associated M918L mutation in the VSSC gene has now emerged in S. scabiei var. hominis mites. Hence, loss of sensitivity to permethrin due to kdr-type resistance may be more prevalent than anticipated and may be decisive for the therapy responsiveness of scabies-infested patients.
01 Sep 2021·The Journal of dermatologyQ3 · MEDICINE
Efficacy and safety of a dimethicone lotion in patients with pyrethroid‐resistant head lice in an epidemic area, Okinawa, Japan
Q3 · MEDICINE
Article
Author: Miyagi, Takuya ; Okamoto, Yuka ; Yamaguchi, Sayaka ; Kawada, Hitoshi ; Takahashi, Kenzo ; Okubo, Yuko ; Yasumura, Ryo
Abstract:
Pyrethroid insecticides are the only pesticides approved for the treatment of head lice (pediculosis capitis) infestations in Japan. However, in Okinawa Prefecture, 96% of head lice are resistant to pyrethroids. Here, we conducted a clinical trial to assess the safety and efficacy of a dimethicone preparation against head lice infestations in Okinawa Prefecture. Dimethicone‐containing lotion was applied over the entire scalp three times over a 7‐day period. Lice bodies (nymphs/adults) and eggs (nits) were counted before (day 0) and after treatment (day 8); a subset of eggs was collected to estimate viability based on hatch rate. Efficacy was evaluated based on improvement (reduction) in head lice counts post‐treatment with respect to baseline. Safety was evaluated based on subjects’ scalp condition and adverse event incidence. Utility was a composite end‐point combining efficacy and safety. In total, 35 subjects were enrolled. Efficacy and safety were evaluated in 23 and 35 subjects, respectively. No side‐effects of note were reported during the treatment period. The dimethicone lotion resulted in a utility rating of “marginally useful” or higher in over 80% of the study population, signifying the formulation to be both safe and effective. The dimethicone lotion was also a potent ovicide; 99.4% of eggs collected after treatment failed to hatch when incubated. Eradication of head lice remained successful for at least 4 weeks after the final topical dimethicone application in 25 of the 28 subjects reached by telephone survey. Lice bodies and eggs were genotyped to analyze the prevalence of three knockdown resistance (kdr)‐type mutations within the voltage‐sensitive sodium channel known to confer pyrethroid resistance. One or more kdr mutations were confirmed in 30 of the 32 subjects from whom specimens were collected (93.8%). Dimethicone was confirmed to be both safe and effective in treating pyrethroid‐resistant head lice.
01 Mar 2020·Pesticide biochemistry and physiology
Regional and seasonal detection of resistance mutation frequencies in field populations of Anopheles Hyrcanus Group and Culex pipiens complex in Korea
Article
Author: Klein, Terry A ; Kim, Ju Hyeon ; Lee, Si Hyeock ; Kim, Heung-Chul ; Choi, Kwang Shik ; Lee, Do Eun ; Kim, Young Ho ; Chong, Sung-Tae
Pyrethroid (PYR) and organophosphate (OP) insecticides have been extensively used for mosquito control for several decades in South Korea, and has resulted in the rapid development of resistance in the field. In this study, quantitative sequencing (QS) protocols were developed for the frequency prediction of insecticide resistance alleles [e.g., the L1014F/C mutation on the voltage sensitive sodium channel as a PYR resistance allele and the G119S mutation on the acetylcholinesterase 1 as OP resistance alleles] in four regional populations of Anopheles Hyrcanus Group and Culex pipiens complex. Both of the L1014F/C and G119S mutations were observed in all examined regional populations of An. Hyrcanus Group, suggesting a wide distribution of both PYR and OP resistance. In contrast, populations of the Cx. pipiens complex were determined to possess almost no G119S mutation, but relatively higher frequencies of the L1014F mutation, showing differential resistance patterns between different mosquito groups. The mutation frequencies were also monitored throughout a mosquito season (May-October) at one collection site to determine the seasonal changes of resistance mutation frequency in mosquito populations. Dramatic decreases of both L1014F/C and G119S mutation frequencies were observed in the An. Hyrcanus Group toward the fall, with no mutations observed in the early spring, suggesting a connection between the fitness costs of overwintering and insecticide resistance. However, no apparent trends were detectable in the Cx. pipiens complex populations due to low or zero mutation frequencies.
Analysis
Perform a panoramic analysis of this field.
login
or
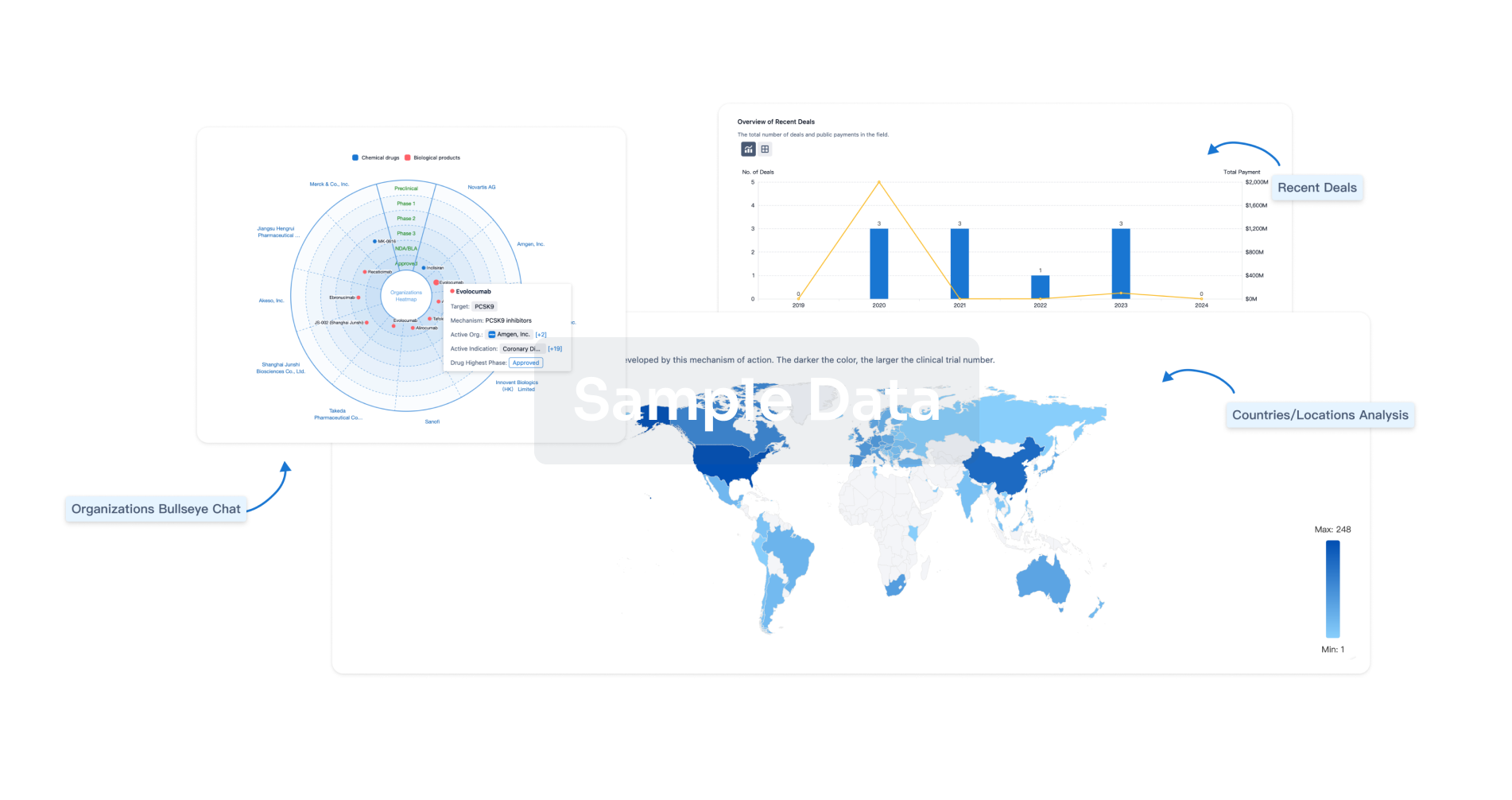
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


