Request Demo
Last update 08 May 2025
DIO2
Last update 08 May 2025
Basic Info
Synonyms 5DII, deiodinase-2, deiodinase, iodothyronine type II + [13] |
Introduction Responsible for the deiodination of T4 (3,5,3',5'-tetraiodothyronine) into T3 (3,5,3'-triiodothyronine). Essential for providing the brain with appropriate levels of T3 during the critical period of development. |
Related
100 Clinical Results associated with DIO2
Login to view more data
100 Translational Medicine associated with DIO2
Login to view more data
0 Patents (Medical) associated with DIO2
Login to view more data
1,299
Literatures (Medical) associated with DIO225 Apr 2025·Circulation Research
Local DIO2 Elevation Is an Adaption in Malformed Cerebrovasculature
Article
Author: Tang, Yushan ; Zhang, Yu ; Lv, Cheng ; Yu, Liang ; Hu, Pengyan ; Wang, Yibo ; Li, Ruofei ; Wang, Haiyue ; Gerdes, A. Martin
24 Mar 2025·Endocrinology
FVB But Not B6 Mice Carrying the Thr92Ala-Dio2 Polymorphism Have Impaired Thyroid Hormonogenesis and Goiter
Article
Author: Arvan, Peter ; Salas-Lucia, Federico ; Bianco, Antonio C ; Ribeiro, Miriam O ; McAninch, Elizabeth A ; Bocco, Barbara M L C ; Zhang, Xiaohan ; Fonseca, Tatiana L ; Batistuzzo, Alice
20 Mar 2025·Biological and Pharmaceutical Bulletin
Estradiol Regulates the Expression of Type 3 Deiodinase in a Chondrocyte Cell Line
Article
Author: Moriyama, Kenji ; Hayashi, Misa ; Hano, Hiromi ; Mitsutani, Mana ; Yamauchi, Ichiro ; Matsushita, Midori ; Tagami, Tetsuya ; Yokoyama, Mei
Analysis
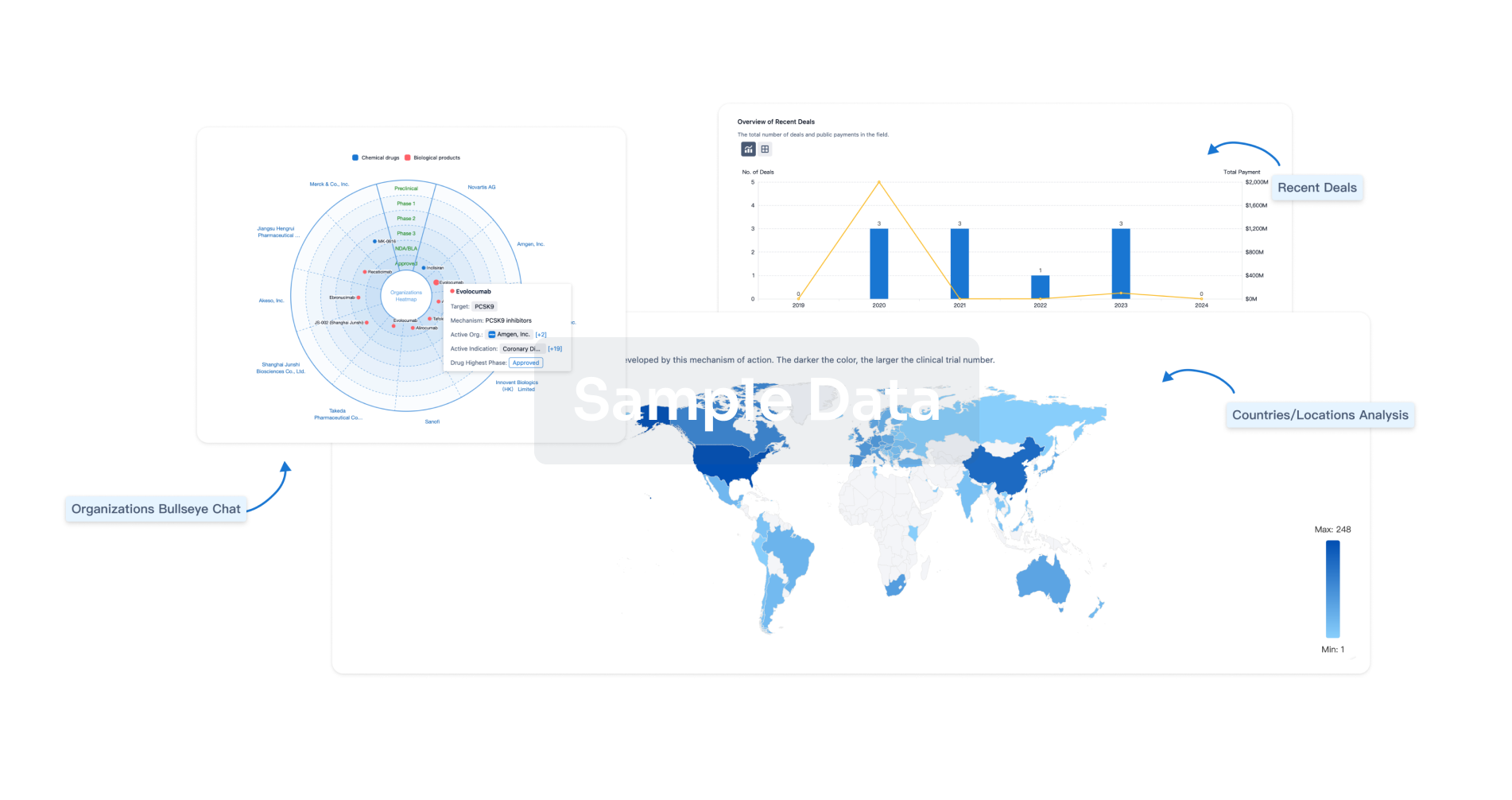
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free