Request Demo
Last update 08 May 2025
GOT1
Last update 08 May 2025
Basic Info
Synonyms Aspartate aminotransferase, cytoplasmic, AST1, cAspAT + [7] |
Introduction Biosynthesis of L-glutamate from L-aspartate or L-cysteine (PubMed:21900944). Important regulator of levels of glutamate, the major excitatory neurotransmitter of the vertebrate central nervous system. Acts as a scavenger of glutamate in brain neuroprotection. The aspartate aminotransferase activity is involved in hepatic glucose synthesis during development and in adipocyte glyceroneogenesis. Using L-cysteine as substrate, regulates levels of mercaptopyruvate, an important source of hydrogen sulfide. Mercaptopyruvate is converted into H(2)S via the action of 3-mercaptopyruvate sulfurtransferase (3MST). Hydrogen sulfide is an important synaptic modulator and neuroprotectant in the brain. In addition, catalyzes (2S)-2-aminobutanoate, a by-product in the cysteine biosynthesis pathway (PubMed:27827456). |
Related
1
Drugs associated with GOT1Target |
Mechanism ALP modulators [+2] |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with GOT1
Login to view more data
100 Translational Medicine associated with GOT1
Login to view more data
0 Patents (Medical) associated with GOT1
Login to view more data
13,016
Literatures (Medical) associated with GOT131 Dec 2025·Annals of Medicine
Aspartate aminotransferase-to-platelet ratio index as a novel predictor of early mortality in heat stroke patients: a multi-centre retrospective study
Article
Author: Cao, Yuan ; Kang, Hong-Jun ; Wang, Sheng-Yuan ; Jiao, Jie ; Wang, Min ; Wu, Yi-Qi ; Song, Bin ; Yang, Meng-Meng ; Liu, Fu-Jing ; Li, Yun ; Wang, Lu
01 Dec 2025·Molecular Biology Reports
Atypical pathogen community-acquired pneumonia: an analysis of clinical characteristics, drug treatment, and prognosis in the related patients
Review
Author: Yu, Ying ; Li, Minghui
01 Dec 2025·European Journal of Trauma and Emergency Surgery
The role of serum vaspin level in the early diagnosis of mesenteric ischemia induced in experimental animal model
Article
Author: Çakir, Remzi Can ; Doğan, Uğur ; Aydemir, Erhan ; Ellidağ, Hamit Yaşar ; Yildiz, Turan Can ; Etli, Özlem ; Çelik, Ömer ; Eyvaz, Kemal
13
News (Medical) associated with GOT111 Apr 2025
First Global Phase 3 Trial Showing Substantial Survival Advantage Over Chemotherapy, for Patients With Progression On or After Platinum-Based Chemotherapy
THOUSAND OAKS, Calif., April 11, 2025 /PRNewswire/ -- Amgen (NASDAQ:AMGN) today announced that the global Phase 3 DeLLphi-304 clinical trial evaluating IMDELLTRA® (tarlatamab-dlle) as a treatment for patients with small cell lung cancer (SCLC) who progressed on or after a single line of platinum-based chemotherapy met its primary endpoint at a planned interim analysis. IMDELLTRA demonstrated statistically significant and clinically meaningful improvement in overall survival (OS) compared to local standard-of-care (SOC) chemotherapy.
"Small cell lung cancer is one of the most aggressive malignancies, with a high unmet need for more effective therapies.1 The topline results from DeLLphi-304 demonstrate overwhelming clinical benefit for people living with this devastating disease and affirm IMDELLTRA as standard of care," said Jay Bradner, M.D., executive vice president, Research and Development, at Amgen. "We look forward to sharing these results with the scientific community and health authorities as we continue our efforts to bring IMDELLTRA to patients worldwide."
The safety profile for IMDELLTRA was consistent with its known profile. Detailed data from DeLLphi-304 will be presented at an upcoming medical congress.
DeLLphi-304 is a global Phase 3 randomized controlled open-label clinical trial evaluating the efficacy and safety of IMDELLTRA as a treatment for patients with SCLC who progressed on or after a single line of platinum-based chemotherapy.2 Patients were randomized to receive either IMDELLTRA or local SOC chemotherapy (topotecan in all countries except Japan; lurbinectedin in the U.S., Canada, Australia, Singapore, Korea; and amrubicin in Japan).2,3 The primary outcome measure of the trial is OS.2
About IMDELLTRA® (tarlatamab-dlle)
IMDELLTRA is a first-in-class immunotherapy engineered by Amgen researchers that binds to both DLL3 on tumor cells and CD3 on T cells, activating T cells to kill DLL3-expressing SCLC cells. This results in the formation of a cytolytic synapse with lysis of the cancer cell.4,5 DLL3 is a protein that is expressed on the surface of SCLC cells in ~85-96% of patients with SCLC, but is minimally expressed on healthy cells, making it an exciting target.6,7
IMDELLTRA® (tarlatamab-dlle) U.S. Indication
IMDELLTRA® (tarlatamab-dlle) is indicated for the treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC) with disease progression on or after platinum-based chemotherapy.
This indication is approved under accelerated approval based on overall response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
About Small Cell Lung Cancer (SCLC)
SCLC is one of the most aggressive and devastating solid tumor malignancies, with a 5-10% five-year relative survival rate across all stages combined.1 SCLC comprises about 15% of the more than 2.4 million patients diagnosed with lung cancer worldwide each year.8-10 Despite initial high response rates to first-line platinum-based chemotherapy, most patients quickly relapse within months and require subsequent treatment options.9
About Tarlatamab Clinical Trials
Amgen's robust tarlatamab development program includes the DeLLphi clinical trials, which evaluate tarlatamab as both a monotherapy and in combination regimens in earlier lines of SCLC.
Tarlatamab is being investigated in multiple studies including DeLLphi-303, a Phase 1b study investigating tarlatamab in combination with standard of care therapies in first-line ES-SCLC; DeLLphi-304, a randomized Phase 3 trial comparing tarlatamab monotherapy with standard of care chemotherapy in second-line treatment of SCLC; DeLLphi-305, a randomized Phase 3 trial comparing tarlatamab in combination with durvalumab versus durvalumab alone as first-line maintenance treatment in ES-SCLC; DeLLphi-306, a randomized placebo-controlled Phase 3 trial of tarlatamab following concurrent chemoradiotherapy in limited-stage SCLC; DeLLphi-308, a Phase 1b study evaluating subcutaneous tarlatamab in second line or later ES-SCLC; and DeLLphi-309, a Phase 2 study evaluating alternative intravenous dosing regimens with tarlatamab in second-line ES-SCLC.11
For more information, please visit .
About Amgen
Amgen discovers, develops, manufactures and delivers innovative medicines to help millions of patients in their fight against some of the world's toughest diseases. More than 40 years ago, Amgen helped to establish the biotechnology industry and remains on the cutting-edge of innovation, using technology and human genetic data to push beyond what's known today. Amgen is advancing a broad and deep pipeline that builds on its existing portfolio of medicines to treat cancer, heart disease, osteoporosis, inflammatory diseases and rare diseases.
In 2024, Amgen was named one of the "World's Most Innovative Companies" by Fast Company and one of "America's Best Large Employers" by Forbes, among other external recognitions. Amgen is one of the 30 companies that comprise the Dow Jones Industrial Average®, and it is also part of the Nasdaq-100 Index®, which includes the largest and most innovative non-financial companies listed on the Nasdaq Stock Market based on market capitalization.
For more information, visit Amgen.com and follow Amgen on X, LinkedIn, Instagram, YouTube and Threads.
IMDELLTRA® (tarlatamab-dlle) Important Safety Information
WARNING: CYTOKINE RELEASE SYNDROME AND NEUROLOGIC TOXICITY including IMMUNE EFFECTOR CELL-ASSOCIATED NEUROTOXICITY SYNDROME
Cytokine release syndrome (CRS), including serious or life-threatening reactions, can occur in patients receiving IMDELLTRA®. Initiate treatment with IMDELLTRA® using the step-up dosing schedule to reduce the incidence and severity of CRS. Withhold IMDELLTRA® until CRS resolves or permanently discontinue based on severity.
Neurologic toxicity, including immune effector cell-associated neurotoxicity syndrome (ICANS), including serious or life-threatening reactions, can occur in patients receiving IMDELLTRA®. Monitor patients for signs and symptoms of neurologic toxicity, including ICANS, during treatment and treat promptly. Withhold IMDELLTRA® until ICANS resolves or permanently discontinue based on severity.
WARNINGS AND PRECAUTIONS
Cytokine Release Syndrome (CRS): IMDELLTRA® can cause CRS including serious or life-threatening reactions. In the pooled safety population, CRS occurred in 55% of patients who received IMDELLTRA®, including 34% Grade 1, 19% Grade 2, 1.1% Grade 3 and 0.5% Grade 4. Recurrent CRS occurred in 24% of patients, including 18% Grade 1 and 6% Grade 2.
Most events (43%) of CRS occurred after the first dose, with 29% of patients experiencing any grade CRS after the second dose and 9% of patients experiencing CRS following the third dose or later. Following the Day 1, Day 8, and Day 15 infusions, 16%, 4.3% and 2.1% of patients experienced ≥ Grade 2 CRS, respectively. The median time to onset of all grade CRS from most recent dose of IMDELLTRA® was 13.5 hours (range: 1 to 268 hours). The median time to onset of ≥ Grade 2 CRS from most recent dose of IMDELLTRA® was 14.6 hours (range: 2 to 566 hours).
Clinical signs and symptoms of CRS included pyrexia, hypotension, fatigue, tachycardia, headache, hypoxia, nausea, and vomiting. Potentially life-threatening complications of CRS may include cardiac dysfunction, acute respiratory distress syndrome, neurologic toxicity, renal and/or hepatic failure, and disseminated intravascular coagulation (DIC).
Administer IMDELLTRA® following the recommended step-up dosing and administer concomitant medications before and after Cycle 1 IMDELLTRA® infusions as described in Table 3 of the Prescribing Information (PI) to reduce the risk of CRS. Administer IMDELLTRA® in an appropriate health care facility equipped to monitor and manage CRS. Ensure patients are well hydrated prior to administration of IMDELLTRA®.
Closely monitor patients for signs and symptoms of CRS during treatment with IMDELLTRA®. At the first sign of CRS, immediately discontinue IMDELLTRA® infusion, evaluate the patient for hospitalization and institute supportive care based on severity. Withhold or permanently discontinue IMDELLTRA® based on severity. Counsel patients to seek medical attention should signs or symptoms of CRS occur.
Neurologic Toxicity, Including ICANS: IMDELLTRA® can cause serious or life-threatening neurologic toxicity, including ICANS. In the pooled safety population, neurologic toxicity, including ICANS, occurred in 47% of patients who received IMDELLTRA®, including 10% Grade 3. The most frequent neurologic toxicities were headache (14%), peripheral neuropathy (7%), dizziness (7%), insomnia (6%), muscular weakness (3.7%), delirium (2.1%), syncope (1.6%), and neurotoxicity (1.1%).
ICANS occurred in 9% of IMDELLTRA®-treated patients. Recurrent ICANS occurred in 1.6% of patients. Most patients experienced ICANS following Cycle 2 Day 1 (24%). Following Day 1, Day 8, and Day 15 infusions, 0.5%, 0.5% and 3.7% of patients experienced ≥ Grade 2 ICANS, respectively. The median time to onset of ICANS from the first dose of IMDELLTRATM was 29.5 days (range: 1 to 154 days). ICANS can occur several weeks following administration of IMDELLTRATM. The median time to resolution of ICANS was 33 days (range: 1 to 93 days).
The onset of ICANS can be concurrent with CRS, following resolution of CRS, or in the absence of CRS. Clinical signs and symptoms of ICANS may include but are not limited to confusional state, depressed level of consciousness, disorientation, somnolence, lethargy, and bradyphrenia.
Patients receiving IMDELLTRA® are at risk of neurologic adverse reactions and ICANS resulting in depressed level of consciousness. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, in the event of any neurologic symptoms until they resolve.
Closely monitor patients for signs and symptoms of neurologic toxicity and ICANS during treatment. At the first sign of ICANS, immediately evaluate the patient and provide supportive therapy based on severity. Withhold IMDELLTRA® or permanently discontinue based on severity.
Cytopenias: IMDELLTRA® can cause cytopenias including neutropenia, thrombocytopenia, and anemia. In the pooled safety population, decreased neutrophils occurred in 12% including 6% Grade 3 or 4 of IMDELLTRA®-treated patients. The median time to onset for Grade 3 or 4 neutropenia was 29.5 days (range: 2 to 213). Decreased platelets occurred in 33% including 3.2% Grade 3 or 4. The median time to onset for Grade 3 or 4 decreased platelets was 50 days (range: 3 to 420). Decreased hemoglobin occurred in 58% including 5% Grade 3 or 4. Febrile neutropenia occurred in 0.5% of patients treated with IMDELLTRA®.
Monitor patients for signs and symptoms of cytopenias. Perform complete blood counts prior to treatment with IMDELLTRA®, before each dose, and as clinically indicated. Based on the severity of cytopenias, temporarily withhold, or permanently discontinue IMDELLTRA®.
Infections: IMDELLTRA® can cause serious infections, including life-threatening and fatal infections. In the pooled safety population, infections, including opportunistic infections, occurred in 41% of patients who received IMDELLTRA®. Grade 3 or 4 infections occurred in 13% of patients. The most frequent infections were COVID-19 (9%, majority during the COVID-19 pandemic), urinary tract infection (10%), pneumonia (9%), respiratory tract infection (3.2%), and candida infection (3.2%).
Monitor patients for signs and symptoms of infection prior to and during treatment with IMDELLTRA® and treat as clinically indicated. Withhold or permanently discontinue IMDELLTRA® based on severity.
Hepatotoxicity: IMDELLTRA® can cause hepatotoxicity. In the pooled safety population, elevated ALT occurred in 42%, with Grade 3 or 4 ALT elevation occurring in 2.1%. Elevated AST occurred in 44% of patients, with Grade 3 or 4 AST elevation occurring in 3.2%. Elevated bilirubin occurred in 15% of patients; Grade 3 or 4 total bilirubin elevations occurred in 1.6% of patients. Liver enzyme elevation can occur with or without concurrent CRS. Monitor liver enzymes and bilirubin prior to treatment with IMDELLTRA®, before each dose, and as clinically indicated. Withhold IMDELLTRA® or permanently discontinue based on severity.
Hypersensitivity: IMDELLTRA® can cause severe hypersensitivity reactions. Clinical signs and symptoms of hypersensitivity may include, but are not limited to, rash and bronchospasm. Monitor patients for signs and symptoms of hypersensitivity during treatment with IMDELLTRA® and manage as clinically indicated. Withhold or consider permanent discontinuation of IMDELLTRA® based on severity.
Embryo-Fetal Toxicity: Based on its mechanism of action, IMDELLTRA® may cause fetal harm when administered to a pregnant woman. Advise patients of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with IMDELLTRA® and for 2 months after the last dose.
ADVERSE REACTIONS
The most common (> 20%) adverse reactions were CRS (55%), fatigue (51%), pyrexia (36%), dysgeusia (36%), decreased appetite (34%), musculoskeletal pain (30%), constipation (30%), anemia (27%) and nausea (22%). The most common (≥ 2%) Grade 3 or 4 laboratory abnormalities were decreased lymphocytes (57%), decreased sodium (16%), increased uric acid (10%), decreased total neutrophils (6%), decreased hemoglobin (5%), increased activated partial thromboplastin time (5%), decreased potassium (5%), increased aspartate aminotransferase (3.2%), decreased white blood cells (3.8%), decreased platelets (3.2%), and increased alanine aminotransferase (2.1%).
Serious adverse reactions occurred in 58% of patients. Serious adverse reactions in > 3% of patients included CRS (24%), pneumonia (6%), pyrexia (3.7%), and hyponatremia (3.6%). Fatal adverse reactions occurred in 2.7% of patients including pneumonia (0.5%), aspiration (0.5%), pulmonary embolism (0.5%), respiratory acidosis (0.5%), and respiratory failure (0.5%).
DOSAGE AND ADMINISTRATION: Important Dosing Information
Administer IMDELLTRA® as an intravenous infusion over one hour.
Administer IMDELLTRA® according to the step-up dosing schedule in the IMDELLTRA® PI (Table 1) to reduce the incidence and severity of CRS.
For Cycle 1, administer recommended concomitant medications before and after Cycle 1 IMDELLTRA® infusions to reduce the risk of CRS reactions as described in the PI (Table 3).
IMDELLTRA® should only be administered by a qualified healthcare professional with appropriate medical support to manage severe reactions such as CRS and neurologic toxicity including ICANS.
Due to the risk of CRS and neurologic toxicity, including ICANS, monitor patients from the start of the IMDELLTRA® infusion for 22 to 24 hours on Cycle 1 Day 1 and Cycle 1 Day 8 in an appropriate healthcare setting.
Recommend that patients remain within 1 hour of an appropriate healthcare setting for a total of 48 hours from start of the infusion with IMDELLTRA® following Cycle 1 Day 1 and Cycle 1 Day 8 doses, accompanied by a caregiver.
Prior to administration of IMDELLTRA® evaluate complete blood count, liver enzymes, and bilirubin before each dose, and as clinically indicated.
Ensure patients are well hydrated prior to administration of IMDELLTRA®.
Please see IMDELLTRA®
full Prescribing Information
, including BOXED WARNINGS.
Amgen Forward-Looking Statements
This news release contains forward-looking statements that are based on the current expectations and beliefs of Amgen. All statements, other than statements of historical fact, are statements that could be deemed forward-looking statements, including any statements on the outcome, benefits and synergies of collaborations, or potential collaborations, with any other company (including BeiGene, Ltd. or Kyowa Kirin Co., Ltd.), the performance of Otezla® (apremilast) , our acquisitions of ChemoCentryx, Inc., or Horizon Therapeutics plc (including the prospective performance and outlook of Horizon's business, performance and opportunities, and any potential strategic benefits, synergies or opportunities expected as a result of such acquisition), as well as estimates of revenues, operating margins, capital expenditures, cash, other financial metrics, expected legal, arbitration, political, regulatory or clinical results or practices, customer and prescriber patterns or practices, reimbursement activities and outcomes, effects of pandemics or other widespread health problems on our business, outcomes, progress, and other such estimates and results. Forward-looking statements involve significant risks and uncertainties, including those discussed below and more fully described in the Securities and Exchange Commission reports filed by Amgen, including our most recent annual report on Form 10-K and any subsequent periodic reports on Form 10-Q and current reports on Form 8-K. Unless otherwise noted, Amgen is providing this information as of the date of this news release and does not undertake any obligation to update any forward-looking statements contained in this document as a result of new information, future events or otherwise.
No forward-looking statement can be guaranteed and actual results may differ materially from those we project. Discovery or identification of new product candidates or development of new indications for existing products cannot be guaranteed and movement from concept to product is uncertain; consequently, there can be no guarantee that any particular product candidate or development of a new indication for an existing product will be successful and become a commercial product. Further, preclinical results do not guarantee safe and effective performance of product candidates in humans. The complexity of the human body cannot be perfectly, or sometimes, even adequately modeled by computer or cell culture systems or animal models. The length of time that it takes for us to complete clinical trials and obtain regulatory approval for product marketing has in the past varied and we expect similar variability in the future. Even when clinical trials are successful, regulatory authorities may question the sufficiency for approval of the trial endpoints we have selected. We develop product candidates internally and through licensing collaborations, partnerships and joint ventures. Product candidates that are derived from relationships may be subject to disputes between the parties or may prove to be not as effective or as safe as we may have believed at the time of entering into such relationship. Also, we or others could identify safety, side effects or manufacturing problems with our products, including our devices, after they are on the market.
Our results may be affected by our ability to successfully market both new and existing products domestically and internationally, clinical and regulatory developments involving current and future products, sales growth of recently launched products, competition from other products including biosimilars, difficulties or delays in manufacturing our products and global economic conditions, including those resulting from geopolitical relations or government actions. In addition, sales of our products are affected by pricing pressure, political and public scrutiny and reimbursement policies imposed by third-party payers, including governments, private insurance plans and managed care providers and may be affected by regulatory, clinical and guideline developments and domestic and international trends toward managed care and healthcare cost containment. Furthermore, our research, testing, pricing, marketing and other operations are subject to extensive regulation by domestic and foreign government regulatory authorities. Our business may be impacted by government investigations, litigation and product liability claims. In addition, our business may be impacted by the adoption of new tax legislation or exposure to additional tax liabilities. Further, while we routinely obtain patents for our products and technology, the protection offered by our patents and patent applications may be challenged, invalidated or circumvented by our competitors, or we may fail to prevail in present and future intellectual property litigation. We perform a substantial amount of our commercial manufacturing activities at a few key facilities, including in Puerto Rico, and also depend on third parties for a portion of our manufacturing activities, and limits on supply may constrain sales of certain of our current products and product candidate development. An outbreak of disease or similar public health threat and the public and governmental effort to mitigate against the spread of such disease, could have a significant adverse effect on the supply of materials for our manufacturing activities, the distribution of our products, the commercialization of our product candidates, and our clinical trial operations, and any such events may have a material adverse effect on our product development, product sales, business and results of operations. We rely on collaborations with third parties for the development of some of our product candidates and for the commercialization and sales of some of our commercial products. In addition, we compete with other companies with respect to many of our marketed products as well as for the discovery and development of new products. Further, some raw materials, medical devices and component parts for our products are supplied by sole third-party suppliers. Certain of our distributors, customers and payers have substantial purchasing leverage in their dealings with us. The discovery of significant problems with a product similar to one of our products that implicate an entire class of products could have a material adverse effect on sales of the affected products and on our business and results of operations. Our efforts to collaborate with or acquire other companies, products or technology, and to integrate the operations of companies or to support the products or technology we have acquired, may not be successful. There can be no guarantee that we will be able to realize any of the strategic benefits, synergies or opportunities arising from the Horizon acquisition, and such benefits, synergies or opportunities may take longer to realize than expected. We may not be able to successfully integrate Horizon, and such integration may take longer, be more difficult or cost more than expected. A breakdown, cyberattack or information security breach of our information technology systems could compromise the confidentiality, integrity and availability of our systems and our data. Our stock price is volatile and may be affected by a number of events. Our business and operations may be negatively affected by the failure, or perceived failure, of achieving our sustainability objectives. The effects of global climate change and related natural disasters could negatively affect our business and operations. Global economic conditions may magnify certain risks that affect our business. Our business performance could affect or limit the ability of our Board of Directors to declare a dividend or our ability to pay a dividend or repurchase our common stock. We may not be able to access the capital and credit markets on terms that are favorable to us, or at all.
The scientific information discussed in this news release related to our product candidates is preliminary and investigative. Such product candidates are not approved by the U.S. Food and Drug Administration, and no conclusions can or should be drawn regarding the safety or effectiveness of the product candidates. Further, any scientific information discussed in this news release relating to new indications for our products is preliminary and investigative and is not part of the labeling approved by the U.S. Food and Drug Administration for the products. The products are not approved for the investigational use(s) discussed in this news release, and no conclusions can or should be drawn regarding the safety or effectiveness of the products for these uses.
CONTACT: Amgen, Thousand Oaks
Elissa Snook, 609-251-1407 (media)
Justin Claeys, 805-313-9775 (investors)
REFERENCES:
PDQ® Adult Treatment Editorial Board. PDQ Small Cell Lung Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated June 27, 2024. Available at: . Accessed March 25, 2025.
DeLLphi-304 Clinical Trial Listing. Available at: . Accessed March 24, 2025.
Paz-Ares, et al. JCO. 41, TPS8611-TPS8611(2023). DOI:10.1200/JCO.2023.41.16_suppl.TPS8611
Giffin MJ, Cooke K, Lobenhofer EK, et al. AMG 757, a Half-Life Extended, DLL3-Targeted Bispecific T-Cell Engager, Shows High Potency and Sensitivity in Preclinical Models of Small-Cell Lung Cancer. Clin Cancer Res. 2021;27:1526-1537.
Baeuerle PA, Kufer P, Bargou R. BiTE: Teaching antibodies to engage T-cells for cancer therapy. Curr Opin Mol Ther. 2009;11:22-30.
Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for Patients with Previously Treated Small-Cell Lung Cancer. N Engl J Med. 2023;389:2063-2075.
Rojo F, Corassa M, Mavroudis D, et al. International real-world study of DLL3 expression in patients with small cell lung cancer. Lung Cancer. 2020;147:237-243.
World Health Organization. Lung. 2022. Available at: . Accessed on March 24, 2025.
Oronsky B, Abrouk N, Caroen S, et al. A 2022 Update on Extensive Stage Small-Cell Lung Cancer (SCLC). J Cancer. 2022;13:2945-2953.
Sabari JK, Lok BH, Laird JH, et al. Unravelling the biology of SCLC: implications for therapy. Nat Rev Clin Oncol. 2017;14:549-561.
Clinical Trials. Tarlatamab Clinical Trial Listings. . Accessed March 25, 2025.
SOURCE Amgen
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
Phase 3Clinical ResultPhase 2ImmunotherapyAccelerated Approval
27 Mar 2025
March 27, 2025 12:01 pm ET
Subcutaneous pembrolizumab administered every six weeks with a median injection time of two minutes, in combination with chemotherapy, shows consistent results across reported efficacy and safety endpoints compared to IV KEYTRUDA in combination with chemotherapy
A time and motion descriptive analysis shows nearly 50% reductions in patient chair and treatment room time, and in total active healthcare professional time related to treatment tasks, for subcutaneous pembrolizumab compared to IV KEYTRUDA
Applications for subcutaneous pembrolizumab are under review in the U.S. and Europe
RAHWAY, N.J.--(BUSINESS WIRE)--
Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced the first data presentation from the pivotal 3475A-D77 Phase 3 trial, evaluating the subcutaneous administration of pembrolizumab, together with berahyaluronidase alfa (MK-3475A; from now on referred to as “subcutaneous pembrolizumab”). Berahyaluronidase alfa is a variant of human hyaluronidase developed and manufactured by Alteogen Inc. These results are being presented today at the European Lung Cancer Congress (ELCC) 2025 (Abstract #8MO) and published simultaneously in
Annals of Oncology.
The study met its primary endpoints, demonstrating noninferior pharmacokinetics (PK) for subcutaneous pembrolizumab administered with chemotherapy with a median injection time of two minutes, versus intravenous (IV) KEYTRUDA
®
(pembrolizumab) administered with chemotherapy for the first-line treatment of adult patients with metastatic non-small cell lung cancer (NSCLC). The secondary endpoints of objective response rate (ORR), progression-free survival (PFS) and duration of response (DOR) and safety were consistent for subcutaneous pembrolizumab with chemotherapy compared to IV KEYTRUDA with chemotherapy. Median overall survival (OS) was not reached in either arm.
Based on these data, the U.S. Food and Drug Administration (FDA) has accepted for review a Biologics License Application (BLA) seeking approval of subcutaneous pembrolizumab across all previously approved solid tumor indications for KEYTRUDA. The FDA has set a Prescription Drug User Fee Act (PDUFA), or target action, date of Sept. 23, 2025. Additionally, the European Medicines Agency (EMA) has validated an extension application to introduce a new pharmaceutical form and new route of administration for KEYTRUDA.
In addition, results of a prospective, observational time and motion descriptive analysis conducted alongside study 3475A-D77 show that, compared to IV KEYTRUDA, subcutaneous pembrolizumab reduced time for patients spent in-chair and in the treatment room by 49.7% and 47.4%, respectively, and reduced the total active time spent by healthcare professionals (HCPs) on treatment preparation, administration process and patient monitoring by 45.7%. These results are being presented as a poster at ELCC (Poster #33P). Pharmacokinetic, efficacy, safety and time and motion results are described further below.
“These study findings demonstrate subcutaneous pembrolizumab reduces time demands for both the patient and the healthcare provider, all while providing a consistent efficacy and safety profile with IV pembrolizumab,” said Dr. Enriqueta Felip, head of Thoracic Tumors Group, Vall d’Hebron Institute of Oncology. “As a physician, I am thrilled to see these data for subcutaneous pembrolizumab, which, if approved, have the potential to give patients valuable time back in their treatment day with results that are consistent with IV pembrolizumab.”
In the 3475A-D77 trial, subcutaneous pembrolizumab, administered every six weeks with a median injection time of two minutes (4.8 mL) along with chemotherapy, demonstrated noninferiority of area under the curve (AUC) exposure of pembrolizumab during the first dosing cycle (geometric mean ratio of 1.14 [96% CI, 1.06-1.22]; p<0.0001) and model-based trough concentration (Ctrough) of pembrolizumab measured at steady state (geometric mean ratio of 1.67 [94% CI, 1.52-1.84]; p<0.0001), compared to IV KEYTRUDA administered every six weeks with chemotherapy.
“KEYTRUDA has helped transform the treatment of certain cancers, and we continue to pursue innovations that build on this breakthrough medicine to give patients and those who treat them better experiences,” said Dr. Marjorie Green, senior vice president and head of oncology, global clinical development, Merck Research Laboratories. “If approved, we are excited about the potential of subcutaneous pembrolizumab to become a new meaningful treatment option that may increase access and save time needed for administration compared to IV KEYTRUDA. We look forward to working with global regulatory authorities to bring the first subcutaneous checkpoint inhibitor that can be administered in approximately two minutes to patients and providers.”
In the prospective, observational time and motion study, patient time in chair during treatment with pembrolizumab was reduced by 49.7% (weighted means [WM]: 59.0 versus 117.2 minutes) for subcutaneous pembrolizumab with chemotherapy compared to IV KEYTRUDA with chemotherapy. Patients receiving subcutaneous pembrolizumab versus IV KEYTRUDA spent 47.4% less time in the treatment room (WM: 66.7 versus 126.9 minutes). Time associated with chemotherapy administration was removed from chair and treatment room duration. Results also show that subcutaneous pembrolizumab with chemotherapy reduced total active HCP time by 45.7% (WM: 14.0 versus 25.8 minutes;), including 44.6% less time on subcutaneous pembrolizumab preparation (WM: 5.1 versus 9.2 minutes) and 46.7% less time on subcutaneous pembrolizumab administration process and patient monitoring (WM: 8.9 versus 16.7 minutes) compared to IV KEYTRUDA with chemotherapy. The differences as measured by a linear mixed model were statistically significant (p<0.0001) for active HCP and patient time endpoints.
In addition to the 3475A-D77 trial, Merck’s subcutaneous pembrolizumab clinical development program includes the 3475A-F84 Phase 3 trial evaluating subcutaneous pembrolizumab administered alone compared to IV KEYTRUDA alone for the first-line treatment of patients with metastatic NSCLC whose tumors have high PD-L1 expression (tumor proportion score [TPS] ≥50%), as well as the 3475A-F65 Phase 2 trial evaluating subcutaneous pembrolizumab administered alone in relapsed or refractory classical Hodgkin lymphoma and relapsed or refractory primary mediastinal large B-cell lymphoma. Merck is also conducting a patient preference Phase 2 study, 3475A-F11, evaluating participant-reported preference for subcutaneous pembrolizumab compared to IV KEYTRUDA.
Study design and additional data from 3475A-D77
Study 3475A-D77 is a randomized, open-label Phase 3 trial (ClinicalTrials.gov,
NCT05722015
) evaluating the subcutaneous administration of pembrolizumab together with berahyaluronidase alfa administered every six weeks with chemotherapy compared to IV KEYTRUDA administered every six weeks in combination with chemotherapy for the first-line treatment of adult patients with metastatic NSCLC, regardless of PD-L1 TPS expression. The study is designed to assess the dual primary PK endpoints of the AUC of pembrolizumab exposure during the first dosing cycle and the Ctrough of pembrolizumab measured at steady state. Secondary endpoints include additional PK parameters as well as efficacy (ORR, DOR, PFS and OS) and safety. The trial enrolled 377 patients who were randomized (2:1) to receive either subcutaneous pembrolizumab administered with chemotherapy or IV KEYTRUDA in combination with chemotherapy.
Secondary efficacy endpoints of the study, which were descriptive, showed:
An ORR of 45.4% (95% CI, 39.1-51.8) for subcutaneous pembrolizumab with chemotherapy versus 42.1% (95% CI, 33.3-51.2) for IV KEYTRUDA with chemotherapy (ORR ratio of 1.08 [95% CI, 0.85-1.37])
Median DOR of 9.1 months (95% CI, 6.9-not reached [NR]) for subcutaneous pembrolizumab with chemotherapy versus 8.0 months (95% CI, 7.4-NR) for IV KEYTRUDA with chemotherapy
Median PFS for subcutaneous pembrolizumab with chemotherapy of 8.1 months (95% CI, 6.3-8.3) versus 7.8 months (95% CI, 6.2-9.7) for IV KEYTRUDA with chemotherapy (HR=1.05 [95% CI, 0.78-1.43])
Median OS was not reached in either arm (HR=0.81 [95% CI, 0.53-1.22])
Among patients who received subcutaneous pembrolizumab with chemotherapy (n=251), Grade ≥3 adverse events (AEs) occurred in 47% of patients versus 47.6% of patients who received IV KEYTRUDA with chemotherapy (n=126). The incidence of local injection site reactions for subcutaneous pembrolizumab with chemotherapy was 2.4%, all of which were low grade. Treatment-related adverse events (TRAEs) led to discontinuation of subcutaneous pembrolizumab in 8.4% of patients in the subcutaneous pembrolizumab with chemotherapy arm and in 8.7% of patients in the IV KEYTRUDA with chemotherapy arm. Additionally, TRAEs led to discontinuation of chemotherapy in 15.1% of patients in the subcutaneous pembrolizumab with chemotherapy arm and 11.9% of patients in the IV KEYTRUDA with chemotherapy arm. Treatment-related deaths occurred in 3.6% of patients who received subcutaneous pembrolizumab with chemotherapy and 2.4% of patients who received IV KEYTRUDA with chemotherapy.
Study design from time and motion study
The global observational time and motion study enrolled 17 sites across eight countries in Europe (4), South America (3) and Asia (1) from the 3475A-D77 trial. Primary endpoints were patient time in chair during treatment, patient time in treatment room and total active HCP time for tasks related to subcutaneous pembrolizumab preparation, administration process and patient monitoring. Time was measured by trained observers using a stopwatch, and time associated with chemotherapy administration was removed from patient in-chair and treatment room duration. Descriptive statistics were calculated including WM to account for unequal sample sizes across countries in each group. Statistical differences between subcutaneous and IV arms were explored via a linear mixed model.
About KEYTRUDA
®
(pembrolizumab) injection for intravenous use, 100 mg
KEYTRUDA is an anti-programmed death receptor-1 (PD-1) therapy that works by increasing the ability of the body’s immune system to help detect and fight tumor cells. KEYTRUDA is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD- L1 and PD-L2, thereby activating T lymphocytes which may affect both tumor cells and healthy cells.
Merck has the industry’s largest immuno-oncology clinical research program. There are currently more than 1,600 trials studying KEYTRUDA across a wide variety of cancers and treatment settings. The KEYTRUDA clinical program seeks to understand the role of KEYTRUDA across cancers and the factors that may predict a patient's likelihood of benefitting from treatment with KEYTRUDA, including exploring several different biomarkers.
Selected KEYTRUDA
®
(pembrolizumab) Indications in the U.S.
Non-Small Cell Lung Cancer
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of patients with metastatic nonsquamous non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic tumor aberrations.
KEYTRUDA, in combination with carboplatin and either paclitaxel or paclitaxel protein-bound, is indicated for the first-line treatment of patients with metastatic squamous NSCLC.
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with NSCLC expressing PD-L1 [Tumor Proportion Score (TPS) ≥1%] as determined by an FDA-approved test, with no EGFR or ALK genomic tumor aberrations, and is:
Stage III where patients are not candidates for surgical resection or definitive chemoradiation, or
metastatic.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with metastatic NSCLC whose tumors express PD-L1 (TPS ≥1%) as determined by an FDA-approved test, with disease progression on or after platinum-containing chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving KEYTRUDA.
KEYTRUDA is indicated for the treatment of patients with resectable (tumors ≥4 cm or node positive) NSCLC in combination with platinum-containing chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
KEYTRUDA, as a single agent, is indicated as adjuvant treatment following resection and platinum-based chemotherapy for adult patients with Stage IB (T2a ≥4 cm), II, or IIIA NSCLC.
Selected Important Safety Information for KEYTRUDA
Severe and Fatal Immune-Mediated Adverse Reactions
KEYTRUDA is a monoclonal antibody that belongs to a class of drugs that bind to either the programmed death receptor-1 (PD-1) or the programmed death ligand 1 (PD-L1), blocking the PD-1/PD-L1 pathway, thereby removing inhibition of the immune response, potentially breaking peripheral tolerance and inducing immune-mediated adverse reactions. Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue, can affect more than one body system simultaneously, and can occur at any time after starting treatment or after discontinuation of treatment. Important immune-mediated adverse reactions listed here may not include all possible severe and fatal immune-mediated adverse reactions.
Monitor patients closely for symptoms and signs that may be clinical manifestations of underlying immune-mediated adverse reactions. Early identification and management are essential to ensure safe use of anti–PD-1/PD-L1 treatments. Evaluate liver enzymes, creatinine, and thyroid function at baseline and periodically during treatment. For patients with TNBC treated with KEYTRUDA in the neoadjuvant setting, monitor blood cortisol at baseline, prior to surgery, and as clinically indicated. In cases of suspected immune-mediated adverse reactions, initiate appropriate workup to exclude alternative etiologies, including infection. Institute medical management promptly, including specialty consultation as appropriate.
Withhold or permanently discontinue KEYTRUDA depending on severity of the immune-mediated adverse reaction. In general, if KEYTRUDA requires interruption or discontinuation, administer systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or equivalent) until improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider administration of other systemic immunosuppressants in patients whose adverse reactions are not controlled with corticosteroid therapy.
Immune-Mediated Pneumonitis
KEYTRUDA can cause immune-mediated pneumonitis. The incidence is higher in patients who have received prior thoracic radiation. Immune-mediated pneumonitis occurred in 3.4% (94/2799) of patients receiving KEYTRUDA, including fatal (0.1%), Grade 4 (0.3%), Grade 3 (0.9%), and Grade 2 (1.3%) reactions. Systemic corticosteroids were required in 67% (63/94) of patients. Pneumonitis led to permanent discontinuation of KEYTRUDA in 1.3% (36) and withholding in 0.9% (26) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 23% had recurrence. Pneumonitis resolved in 59% of the 94 patients.
Pneumonitis occurred in 8% (31/389) of adult patients with cHL receiving KEYTRUDA as a single agent, including Grades 3-4 in 2.3% of patients. Patients received high-dose corticosteroids for a median duration of 10 days (range: 2 days to 53 months). Pneumonitis rates were similar in patients with and without prior thoracic radiation. Pneumonitis led to discontinuation of KEYTRUDA in 5.4% (21) of patients. Of the patients who developed pneumonitis, 42% interrupted KEYTRUDA, 68% discontinued KEYTRUDA, and 77% had resolution.
Pneumonitis occurred in 7% (41/580) of adult patients with resected NSCLC who received KEYTRUDA as a single agent for adjuvant treatment of NSCLC, including fatal (0.2%), Grade 4 (0.3%), and Grade 3 (1%) adverse reactions. Patients received high-dose corticosteroids for a median duration of 10 days (range: 1 day to 2.3 months). Pneumonitis led to discontinuation of KEYTRUDA in 26 (4.5%) of patients. Of the patients who developed pneumonitis, 54% interrupted KEYTRUDA, 63% discontinued KEYTRUDA, and 71% had resolution.
Immune-Mediated Colitis
KEYTRUDA can cause immune-mediated colitis, which may present with diarrhea. Cytomegalovirus infection/reactivation has been reported in patients with corticosteroid-refractory immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup to exclude alternative etiologies. Immune-mediated colitis occurred in 1.7% (48/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (1.1%), and Grade 2 (0.4%) reactions. Systemic corticosteroids were required in 69% (33/48); additional immunosuppressant therapy was required in 4.2% of patients. Colitis led to permanent discontinuation of KEYTRUDA in 0.5% (15) and withholding in 0.5% (13) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 23% had recurrence. Colitis resolved in 85% of the 48 patients.
Hepatotoxicity and Immune-Mediated Hepatitis
KEYTRUDA as a Single Agent
KEYTRUDA can cause immune-mediated hepatitis. Immune-mediated hepatitis occurred in 0.7% (19/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.4%), and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 68% (13/19) of patients; additional immunosuppressant therapy was required in 11% of patients. Hepatitis led to permanent discontinuation of KEYTRUDA in 0.2% (6) and withholding in 0.3% (9) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, none had recurrence. Hepatitis resolved in 79% of the 19 patients.
KEYTRUDA With Axitinib
KEYTRUDA in combination with axitinib can cause hepatic toxicity. Monitor liver enzymes before initiation of and periodically throughout treatment. Consider monitoring more frequently as compared to when the drugs are administered as single agents. For elevated liver enzymes, interrupt KEYTRUDA and axitinib, and consider administering corticosteroids as needed. With the combination of KEYTRUDA and axitinib, Grades 3 and 4 increased alanine aminotransferase (ALT) (20%) and increased aspartate aminotransferase (AST) (13%) were seen at a higher frequency compared to KEYTRUDA alone. Fifty-nine percent of the patients with increased ALT received systemic corticosteroids. In patients with ALT ≥3 times upper limit of normal (ULN) (Grades 2-4, n=116), ALT resolved to Grades 0-1 in 94%. Among the 92 patients who were rechallenged with either KEYTRUDA (n=3) or axitinib (n=34) administered as a single agent or with both (n=55), recurrence of ALT ≥3 times ULN was observed in 1 patient receiving KEYTRUDA, 16 patients receiving axitinib, and 24 patients receiving both. All patients with a recurrence of ALT ≥3 ULN subsequently recovered from the event.
Immune-Mediated Endocrinopathies
Adrenal Insufficiency
KEYTRUDA can cause primary or secondary adrenal insufficiency. For Grade 2 or higher, initiate symptomatic treatment, including hormone replacement as clinically indicated. Withhold KEYTRUDA depending on severity. Adrenal insufficiency occurred in 0.8% (22/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.3%), and Grade 2 (0.3%) reactions. Systemic corticosteroids were required in 77% (17/22) of patients; of these, the majority remained on systemic corticosteroids. Adrenal insufficiency led to permanent discontinuation of KEYTRUDA in <0.1% (1) and withholding in 0.3% (8) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Hypophysitis
KEYTRUDA can cause immune-mediated hypophysitis. Hypophysitis can present with acute symptoms associated with mass effect such as headache, photophobia, or visual field defects. Hypophysitis can cause hypopituitarism. Initiate hormone replacement as indicated. Withhold or permanently discontinue KEYTRUDA depending on severity. Hypophysitis occurred in 0.6% (17/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.3%), and Grade 2 (0.2%) reactions. Systemic corticosteroids were required in 94% (16/17) of patients; of these, the majority remained on systemic corticosteroids. Hypophysitis led to permanent discontinuation of KEYTRUDA in 0.1% (4) and withholding in 0.3% (7) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Thyroid Disorders
KEYTRUDA can cause immune-mediated thyroid disorders. Thyroiditis can present with or without endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate hormone replacement for hypothyroidism or institute medical management of hyperthyroidism as clinically indicated. Withhold or permanently discontinue KEYTRUDA depending on severity. Thyroiditis occurred in 0.6% (16/2799) of patients receiving KEYTRUDA, including Grade 2 (0.3%). None discontinued, but KEYTRUDA was withheld in <0.1% (1) of patients.
Hyperthyroidism occurred in 3.4% (96/2799) of patients receiving KEYTRUDA, including Grade 3 (0.1%) and Grade 2 (0.8%). It led to permanent discontinuation of KEYTRUDA in <0.1% (2) and withholding in 0.3% (7) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement. Hypothyroidism occurred in 8% (237/2799) of patients receiving KEYTRUDA, including Grade 3 (0.1%) and Grade 2 (6.2%). It led to permanent discontinuation of KEYTRUDA in <0.1% (1) and withholding in 0.5% (14) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement. The majority of patients with hypothyroidism required long-term thyroid hormone replacement. The incidence of new or worsening hypothyroidism was higher in 1185 patients with HNSCC, occurring in 16% of patients receiving KEYTRUDA as a single agent or in combination with platinum and FU, including Grade 3 (0.3%) hypothyroidism. The incidence of new or worsening hypothyroidism was higher in 389 adult patients with cHL (17%) receiving KEYTRUDA as a single agent, including Grade 1 (6.2%) and Grade 2 (10.8%) hypothyroidism. The incidence of new or worsening hyperthyroidism was higher in 580 patients with resected NSCLC, occurring in 11% of patients receiving KEYTRUDA as a single agent as adjuvant treatment, including Grade 3 (0.2%) hyperthyroidism. The incidence of new or worsening hypothyroidism was higher in 580 patients with resected NSCLC, occurring in 22% of patients receiving KEYTRUDA as a single agent as adjuvant treatment (KEYNOTE-091), including Grade 3 (0.3%) hypothyroidism.
Type 1 Diabetes Mellitus (DM), Which Can Present With Diabetic Ketoacidosis
Monitor patients for hyperglycemia or other signs and symptoms of diabetes. Initiate treatment with insulin as clinically indicated. Withhold KEYTRUDA depending on severity. Type 1 DM occurred in 0.2% (6/2799) of patients receiving KEYTRUDA. It led to permanent discontinuation in <0.1% (1) and withholding of KEYTRUDA in <0.1% (1) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Immune-Mediated Nephritis With Renal Dysfunction
KEYTRUDA can cause immune-mediated nephritis. Immune-mediated nephritis occurred in 0.3% (9/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.1%), and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 89% (8/9) of patients. Nephritis led to permanent discontinuation of KEYTRUDA in 0.1% (3) and withholding in 0.1% (3) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, none had recurrence. Nephritis resolved in 56% of the 9 patients.
Immune-Mediated Dermatologic Adverse Reactions
KEYTRUDA can cause immune-mediated rash or dermatitis. Exfoliative dermatitis, including Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms, and toxic epidermal necrolysis, has occurred with anti– PD-1/PD-L1 treatments. Topical emollients and/or topical corticosteroids may be adequate to treat mild to moderate nonexfoliative rashes. Withhold or permanently discontinue KEYTRUDA depending on severity. Immune-mediated dermatologic adverse reactions occurred in 1.4% (38/2799) of patients receiving KEYTRUDA, including Grade 3 (1%) and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 40% (15/38) of patients. These reactions led to permanent discontinuation in 0.1% (2) and withholding of KEYTRUDA in 0.6% (16) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 6% had recurrence. The reactions resolved in 79% of the 38 patients.
Other Immune-Mediated Adverse Reactions
The following clinically significant immune-mediated adverse reactions occurred at an incidence of <1% (unless otherwise noted) in patients who received KEYTRUDA or were reported with the use of other anti–PD-1/PD-L1 treatments. Severe or fatal cases have been reported for some of these adverse reactions. Cardiac/Vascular: Myocarditis, pericarditis, vasculitis; Nervous System: Meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis (including exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune neuropathy; Ocular: Uveitis, iritis and other ocular inflammatory toxicities can occur. Some cases can be associated with retinal detachment. Various grades of visual impairment, including blindness, can occur. If uveitis occurs in combination with other immune-mediated adverse reactions, consider a Vogt-Koyanagi-Harada-like syndrome, as this may require treatment with systemic steroids to reduce the risk of permanent vision loss; Gastrointestinal: Pancreatitis, to include increases in serum amylase and lipase levels, gastritis, duodenitis; Musculoskeletal and Connective Tissue: Myositis/polymyositis, rhabdomyolysis (and associated sequelae, including renal failure), arthritis (1.5%), polymyalgia rheumatica; Endocrine: Hypoparathyroidism; Hematologic/Immune: Hemolytic anemia, aplastic anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid organ transplant rejection, other transplant (including corneal graft) rejection.
Infusion-Related Reactions
KEYTRUDA can cause severe or life-threatening infusion-related reactions, including hypersensitivity and anaphylaxis, which have been reported in 0.2% of 2799 patients receiving KEYTRUDA. Monitor for signs and symptoms of infusion-related reactions. Interrupt or slow the rate of infusion for Grade 1 or Grade 2 reactions. For Grade 3 or Grade 4 reactions, stop infusion and permanently discontinue KEYTRUDA.
Complications of Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)
Fatal and other serious complications can occur in patients who receive allogeneic HSCT before or after anti–PD-1/PD-L1 treatments. Transplant-related complications include hyperacute graft-versus-host disease (GVHD), acute and chronic GVHD, hepatic veno-occlusive disease after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause). These complications may occur despite intervening therapy between anti–PD-1/PD-L1 treatments and allogeneic HSCT. Follow patients closely for evidence of these complications and intervene promptly. Consider the benefit vs risks of using anti–PD-1/PD-L1 treatments prior to or after an allogeneic HSCT.
Increased Mortality in Patients With Multiple Myeloma
In trials in patients with multiple myeloma, the addition of KEYTRUDA to a thalidomide analogue plus dexamethasone resulted in increased mortality. Treatment of these patients with an anti–PD-1/PD-L1 treatment in this combination is not recommended outside of controlled trials.
Embryofetal Toxicity
Based on its mechanism of action, KEYTRUDA can cause fetal harm when administered to a pregnant woman. Advise women of this potential risk. In females of reproductive potential, verify pregnancy status prior to initiating KEYTRUDA and advise them to use effective contraception during treatment and for 4 months after the last dose.
Adverse Reactions
In KEYNOTE-006, KEYTRUDA was discontinued due to adverse reactions in 9% of 555 patients with advanced melanoma; adverse reactions leading to permanent discontinuation in more than one patient were colitis (1.4%), autoimmune hepatitis (0.7%), allergic reaction (0.4%), polyneuropathy (0.4%), and cardiac failure (0.4%). The most common adverse reactions (≥20%) with KEYTRUDA were fatigue (28%), diarrhea (26%), rash (24%), and nausea (21%).
In KEYNOTE-054, when KEYTRUDA was administered as a single agent to patients with stage III melanoma, KEYTRUDA was permanently discontinued due to adverse reactions in 14% of 509 patients; the most common (≥1%) were pneumonitis (1.4%), colitis (1.2%), and diarrhea (1%). Serious adverse reactions occurred in 25% of patients receiving KEYTRUDA. The most common adverse reaction (≥20%) with KEYTRUDA was diarrhea (28%). In KEYNOTE-716, when KEYTRUDA was administered as a single agent to patients with stage IIB or IIC melanoma, adverse reactions occurring in patients with stage IIB or IIC melanoma were similar to those occurring in 1011 patients with stage III melanoma from KEYNOTE-054.
In KEYNOTE-189, when KEYTRUDA was administered with pemetrexed and platinum chemotherapy in metastatic nonsquamous NSCLC, KEYTRUDA was discontinued due to adverse reactions in 20% of 405 patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA were pneumonitis (3%) and acute kidney injury (2%). The most common adverse reactions (≥20%) with KEYTRUDA were nausea (56%), fatigue (56%), constipation (35%), diarrhea (31%), decreased appetite (28%), rash (25%), vomiting (24%), cough (21%), dyspnea (21%), and pyrexia (20%).
In KEYNOTE-407, when KEYTRUDA was administered with carboplatin and either paclitaxel or paclitaxel protein-bound in metastatic squamous NSCLC, KEYTRUDA was discontinued due to adverse reactions in 15% of 101 patients. The most frequent serious adverse reactions reported in at least 2% of patients were febrile neutropenia, pneumonia, and urinary tract infection. Adverse reactions observed in KEYNOTE-407 were similar to those observed in KEYNOTE-189 with the exception that increased incidences of alopecia (47% vs 36%) and peripheral neuropathy (31% vs 25%) were observed in the KEYTRUDA and chemotherapy arm compared to the placebo and chemotherapy arm in KEYNOTE-407.
In KEYNOTE-042, KEYTRUDA was discontinued due to adverse reactions in 19% of 636 patients with advanced NSCLC; the most common were pneumonitis (3%), death due to unknown cause (1.6%), and pneumonia (1.4%). The most frequent serious adverse reactions reported in at least 2% of patients were pneumonia (7%), pneumonitis (3.9%), pulmonary embolism (2.4%), and pleural effusion (2.2%). The most common adverse reaction (≥20%) was fatigue (25%).
In KEYNOTE-010, KEYTRUDA monotherapy was discontinued due to adverse reactions in 8% of 682 patients with metastatic NSCLC; the most common was pneumonitis (1.8%). The most common adverse reactions (≥20%) were decreased appetite (25%), fatigue (25%), dyspnea (23%), and nausea (20%).
In KEYNOTE-671, adverse reactions occurring in patients with resectable NSCLC receiving KEYTRUDA in combination with platinum-containing chemotherapy, given as neoadjuvant treatment and continued as single-agent adjuvant treatment, were generally similar to those occurring in patients in other clinical trials across tumor types receiving KEYTRUDA in combination with chemotherapy.
The most common adverse reactions (reported in ≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were fatigue/asthenia, nausea, constipation, diarrhea, decreased appetite, rash, vomiting, cough, dyspnea, pyrexia, alopecia, peripheral neuropathy, mucosal inflammation, stomatitis, headache, weight loss, abdominal pain, arthralgia, myalgia, insomnia, palmar-plantar erythrodysesthesia, urinary tract infection, and hypothyroidism.
In the neoadjuvant phase of KEYNOTE-671, when KEYTRUDA was administered in combination with platinum-containing chemotherapy as neoadjuvant treatment, serious adverse reactions occurred in 34% of 396 patients. The most frequent (≥2%) serious adverse reactions were pneumonia (4.8%), venous thromboembolism (3.3%), and anemia (2%). Fatal adverse reactions occurred in 1.3% of patients, including death due to unknown cause (0.8%), sepsis (0.3%), and immune-mediated lung disease (0.3%). Permanent discontinuation of any study drug due to an adverse reaction occurred in 18% of patients who received KEYTRUDA in combination with platinum-containing chemotherapy; the most frequent adverse reactions (≥1%) that led to permanent discontinuation of any study drug were acute kidney injury (1.8%), interstitial lung disease (1.8%), anemia (1.5%), neutropenia (1.5%), and pneumonia (1.3%).
Of the KEYTRUDA-treated patients who received neoadjuvant treatment, 6% of 396 patients did not receive surgery due to adverse reactions. The most frequent (≥1%) adverse reaction that led to cancellation of surgery in the KEYTRUDA arm was interstitial lung disease (1%).
In the adjuvant phase of KEYNOTE-671, when KEYTRUDA was administered as a single agent as adjuvant treatment, serious adverse reactions occurred in 14% of 290 patients. The most frequent serious adverse reaction was pneumonia (3.4%). One fatal adverse reaction of pulmonary hemorrhage occurred. Permanent discontinuation of KEYTRUDA due to an adverse reaction occurred in 12% of patients who received KEYTRUDA as a single agent, given as adjuvant treatment; the most frequent adverse reactions (≥1%) that led to permanent discontinuation of KEYTRUDA were diarrhea (1.7%), interstitial lung disease (1.4%), increased aspartate aminotransferase (1%), and musculoskeletal pain (1%).
Adverse reactions observed in KEYNOTE-091 were generally similar to those occurring in other patients with NSCLC receiving KEYTRUDA as a single agent, with the exception of hypothyroidism (22%), hyperthyroidism (11%), and pneumonitis (7%). Two fatal adverse reactions of myocarditis occurred.
In KEYNOTE-048, KEYTRUDA monotherapy was discontinued due to adverse events in 12% of 300 patients with HNSCC; the most common adverse reactions leading to permanent discontinuation were sepsis (1.7%) and pneumonia (1.3%). The most common adverse reactions (≥20%) were fatigue (33%), constipation (20%), and rash (20%).
In KEYNOTE-048, when KEYTRUDA was administered in combination with platinum (cisplatin or carboplatin) and FU chemotherapy, KEYTRUDA was discontinued due to adverse reactions in 16% of 276 patients with HNSCC. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA were pneumonia (2.5%), pneumonitis (1.8%), and septic shock (1.4%). The most common adverse reactions (≥20%) were nausea (51%), fatigue (49%), constipation (37%), vomiting (32%), mucosal inflammation (31%), diarrhea (29%), decreased appetite (29%), stomatitis (26%), and cough (22%).
In KEYNOTE-012, KEYTRUDA was discontinued due to adverse reactions in 17% of 192 patients with HNSCC. Serious adverse reactions occurred in 45% of patients. The most frequent serious adverse reactions reported in at least 2% of patients were pneumonia, dyspnea, confusional state, vomiting, pleural effusion, and respiratory failure. The most common adverse reactions (≥20%) were fatigue, decreased appetite, and dyspnea. Adverse reactions occurring in patients with HNSCC were generally similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy, with the exception of increased incidences of facial edema and new or worsening hypothyroidism.
In KEYNOTE-204, KEYTRUDA was discontinued due to adverse reactions in 14% of 148 patients with cHL. Serious adverse reactions occurred in 30% of patients receiving KEYTRUDA; those ≥1% were pneumonitis, pneumonia, pyrexia, myocarditis, acute kidney injury, febrile neutropenia, and sepsis. Three patients died from causes other than disease progression: 2 from complications after allogeneic HSCT and 1 from unknown cause. The most common adverse reactions (≥20%) were upper respiratory tract infection (41%), musculoskeletal pain (32%), diarrhea (22%), and pyrexia, fatigue, rash, and cough (20% each).
In KEYNOTE-087, KEYTRUDA was discontinued due to adverse reactions in 5% of 210 patients with cHL. Serious adverse reactions occurred in 16% of patients; those ≥1% were pneumonia, pneumonitis, pyrexia, dyspnea, GVHD, and herpes zoster. Two patients died from causes other than disease progression: 1 from GVHD after subsequent allogeneic HSCT and 1 from septic shock. The most common adverse reactions (≥20%) were fatigue (26%), pyrexia (24%), cough (24%), musculoskeletal pain (21%), diarrhea (20%), and rash (20%).
In KEYNOTE-170, KEYTRUDA was discontinued due to adverse reactions in 8% of 53 patients with PMBCL. Serious adverse reactions occurred in 26% of patients and included arrhythmia (4%), cardiac tamponade (2%), myocardial infarction (2%), pericardial effusion (2%), and pericarditis (2%). Six (11%) patients died within 30 days of start of treatment. The most common adverse reactions (≥20%) were musculoskeletal pain (30%), upper respiratory tract infection and pyrexia (28% each), cough (26%), fatigue (23%), and dyspnea (21%).
In KEYNOTE-A39, when KEYTRUDA was administered in combination with enfortumab vedotin to patients with locally advanced or metastatic urothelial cancer (n=440), fatal adverse reactions occurred in 3.9% of patients, including acute respiratory failure (0.7%), pneumonia (0.5%), and pneumonitis/ILD (0.2%). Serious adverse reactions occurred in 50% of patients receiving KEYTRUDA in combination with enfortumab vedotin; the serious adverse reactions in ≥2% of patients were rash (6%), acute kidney injury (5%), pneumonitis/ILD (4.5%), urinary tract infection (3.6%), diarrhea (3.2%), pneumonia (2.3%), pyrexia (2%), and hyperglycemia (2%). Permanent discontinuation of KEYTRUDA occurred in 27% of patients. The most common adverse reactions (≥2%) resulting in permanent discontinuation of KEYTRUDA were pneumonitis/ILD (4.8%) and rash (3.4%). The most common adverse reactions (≥20%) occurring in patients treated with KEYTRUDA in combination with enfortumab vedotin were rash (68%), peripheral neuropathy (67%), fatigue (51%), pruritus (41%), diarrhea (38%), alopecia (35%), weight loss (33%), decreased appetite (33%), nausea (26%), constipation (26%), dry eye (24%), dysgeusia (21%), and urinary tract infection (21%).
In KEYNOTE-052, KEYTRUDA was discontinued due to adverse reactions in 11% of 370 patients with locally advanced or metastatic urothelial carcinoma. Serious adverse reactions occurred in 42% of patients; those ≥2% were urinary tract infection, hematuria, acute kidney injury, pneumonia, and urosepsis. The most common adverse reactions (≥20%) were fatigue (38%), musculoskeletal pain (24%), decreased appetite (22%), constipation (21%), rash (21%), and diarrhea (20%).
In KEYNOTE-045, KEYTRUDA was discontinued due to adverse reactions in 8% of 266 patients with locally advanced or metastatic urothelial carcinoma. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was pneumonitis (1.9%). Serious adverse reactions occurred in 39% of KEYTRUDA-treated patients; those ≥2% were urinary tract infection, pneumonia, anemia, and pneumonitis. The most common adverse reactions (≥20%) in patients who received KEYTRUDA were fatigue (38%), musculoskeletal pain (32%), pruritus (23%), decreased appetite (21%), nausea (21%), and rash (20%).
In KEYNOTE-057, KEYTRUDA was discontinued due to adverse reactions in 11% of 148 patients with high-risk NMIBC. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was pneumonitis (1.4%). Serious adverse reactions occurred in 28% of patients; those ≥2% were pneumonia (3%), cardiac ischemia (2%), colitis (2%), pulmonary embolism (2%), sepsis (2%), and urinary tract infection (2%). The most common adverse reactions (≥20%) were fatigue (29%), diarrhea (24%), and rash (24%).
Adverse reactions occurring in patients with MSI-H or dMMR CRC were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-158 and KEYNOTE-164, adverse reactions occurring in patients with MSI-H or dMMR cancer were similar to those occurring in patients with other solid tumors who received KEYTRUDA as a single agent.
In KEYNOTE-811, fatal adverse reactions occurred in 3 patients who received KEYTRUDA in combination with trastuzumab and CAPOX or FP and included pneumonitis in 2 patients and hepatitis in 1 patient. KEYTRUDA was discontinued due to adverse reactions in 13% of 350 patients with locally advanced unresectable or metastatic HER2-positive gastric or GEJ adenocarcinoma. Adverse reactions resulting in permanent discontinuation of KEYTRUDA in ≥1% of patients were pneumonitis (2.0%) and pneumonia (1.1%). In the KEYTRUDA arm vs placebo, there was a difference of ≥5% incidence between patients treated with KEYTRUDA vs standard of care for diarrhea (53% vs 47%), rash (35% vs 28%), hypothyroidism (11% vs 5%), and pneumonia (11% vs 5%).
In KEYNOTE-859, when KEYTRUDA was administered in combination with fluoropyrimidine- and platinum-containing chemotherapy, serious adverse reactions occurred in 45% of 785 patients. Serious adverse reactions in >2% of patients included pneumonia (4.1%), diarrhea (3.9%), hemorrhage (3.9%), and vomiting (2.4%). Fatal adverse reactions occurred in 8% of patients who received KEYTRUDA, including infection (2.3%) and thromboembolism (1.3%). KEYTRUDA was permanently discontinued due to adverse reactions in 15% of patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA (≥1%) were infections (1.8%) and diarrhea (1.0%). The most common adverse reactions (reported in ≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were peripheral neuropathy (47%), nausea (46%), fatigue (40%), diarrhea (36%), vomiting (34%), decreased appetite (29%), abdominal pain (26%), palmar-plantar erythrodysesthesia syndrome (25%), constipation (22%), and weight loss (20%).
In KEYNOTE-590, when KEYTRUDA was administered with cisplatin and fluorouracil to patients with metastatic or locally advanced esophageal or GEJ (tumors with epicenter 1 to 5 centimeters above the GEJ) carcinoma who were not candidates for surgical resection or definitive chemoradiation, KEYTRUDA was discontinued due to adverse reactions in 15% of 370 patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA (≥1%) were pneumonitis (1.6%), acute kidney injury (1.1%), and pneumonia (1.1%). The most common adverse reactions (≥20%) with KEYTRUDA in combination with chemotherapy were nausea (67%), fatigue (57%), decreased appetite (44%), constipation (40%), diarrhea (36%), vomiting (34%), stomatitis (27%), and weight loss (24%).
Adverse reactions occurring in patients with esophageal cancer who received KEYTRUDA as a monotherapy were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-A18, when KEYTRUDA was administered with CRT (cisplatin plus external beam radiation therapy [EBRT] followed by brachytherapy [BT]) to patients with FIGO 2014 Stage III-IVA cervical cancer, fatal adverse reactions occurred in 1.4% of 292 patients, including 1 case each (0.3%) of large intestinal perforation, urosepsis, sepsis, and vaginal hemorrhage. Serious adverse reactions occurred in 30% of patients; those ≥1% included urinary tract infection (2.7%), urosepsis (1.4%), and sepsis (1%). KEYTRUDA was discontinued for adverse reactions in 7% of patients. The most common adverse reaction (≥1%) resulting in permanent discontinuation was diarrhea (1%). For patients treated with KEYTRUDA in combination with CRT, the most common adverse reactions (≥10%) were nausea (56%), diarrhea (50%), vomiting (33%), urinary tract infection (32%), fatigue (26%), hypothyroidism (20%), constipation (18%), decreased appetite and weight loss (17% each), abdominal pain and pyrexia (12% each), hyperthyroidism, dysuria, rash (11% each), and pelvic pain (10%).
In KEYNOTE-826, when KEYTRUDA was administered in combination with paclitaxel and cisplatin or paclitaxel and carboplatin, with or without bevacizumab (n=307), to patients with persistent, recurrent, or first-line metastatic cervical cancer regardless of tumor PD-L1 expression who had not been treated with chemotherapy except when used concurrently as a radio-sensitizing agent, fatal adverse reactions occurred in 4.6% of patients, including 3 cases of hemorrhage, 2 cases each of sepsis and due to unknown causes, and 1 case each of acute myocardial infarction, autoimmune encephalitis, cardiac arrest, cerebrovascular accident, femur fracture with perioperative pulmonary embolus, intestinal perforation, and pelvic infection. Serious adverse reactions occurred in 50% of patients receiving KEYTRUDA in combination with chemotherapy with or without bevacizumab; those ≥3% were febrile neutropenia (6.8%), urinary tract infection (5.2%), anemia (4.6%), and acute kidney injury and sepsis (3.3% each).
KEYTRUDA was discontinued in 15% of patients due to adverse reactions. The most common adverse reaction resulting in permanent discontinuation (≥1%) was colitis (1%).
For patients treated with KEYTRUDA, chemotherapy, and bevacizumab (n=196), the most common adverse reactions (≥20%) were peripheral neuropathy (62%), alopecia (58%), anemia (55%), fatigue/asthenia (53%), nausea and neutropenia (41% each), diarrhea (39%), hypertension and thrombocytopenia (35% each), constipation and arthralgia (31% each), vomiting (30%), urinary tract infection (27%), rash (26%), leukopenia (24%), hypothyroidism (22%), and decreased appetite (21%).
For patients treated with KEYTRUDA in combination with chemotherapy with or without bevacizumab, the most common adverse reactions (≥20%) were peripheral neuropathy (58%), alopecia (56%), fatigue (47%), nausea (40%), diarrhea (36%), constipation (28%), arthralgia (27%), vomiting (26%), hypertension and urinary tract infection (24% each), and rash (22%).
In KEYNOTE-158, KEYTRUDA was discontinued due to adverse reactions in 8% of 98 patients with previously treated recurrent or metastatic cervical cancer. Serious adverse reactions occurred in 39% of patients receiving KEYTRUDA; the most frequent included anemia (7%), fistula, hemorrhage, and infections [except urinary tract infections] (4.1% each). The most common adverse reactions (≥20%) were fatigue (43%), musculoskeletal pain (27%), diarrhea (23%), pain and abdominal pain (22% each), and decreased appetite (21%).
In KEYNOTE-394, KEYTRUDA was discontinued due to adverse reactions in 13% of 299 patients with previously treated hepatocellular carcinoma. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was ascites (2.3%). The most common adverse reactions in patients receiving KEYTRUDA (≥10%) were pyrexia (18%), rash (18%), diarrhea (16%), decreased appetite (15%), pruritus (12%), upper respiratory tract infection (11%), cough (11%), and hypothyroidism (10%).
In KEYNOTE-966, when KEYTRUDA was administered in combination with gemcitabine and cisplatin, KEYTRUDA was discontinued for adverse reactions in 15% of 529 patients with locally advanced unresectable or metastatic biliary tract cancer. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA (≥1%) was pneumonitis (1.3%). Adverse reactions leading to the interruption of KEYTRUDA occurred in 55% of patients. The most common adverse reactions or laboratory abnormalities leading to interruption of KEYTRUDA (≥2%) were decreased neutrophil count (18%), decreased platelet count (10%), anemia (6%), decreased white blood cell count (4%), pyrexia (3.8%), fatigue (3.0%), cholangitis (2.8%), increased ALT (2.6%), increased AST (2.5%), and biliary obstruction (2.3%).
In KEYNOTE-017 and KEYNOTE-913, adverse reactions occurring in patients with MCC (n=105) were generally similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a single agent.
In KEYNOTE-426, when KEYTRUDA was administered in combination with axitinib, fatal adverse reactions occurred in 3.3% of 429 patients. Serious adverse reactions occurred in 40% of patients, the most frequent (≥1%) were hepatotoxicity (7%), diarrhea (4.2%), acute kidney injury (2.3%), dehydration (1%), and pneumonitis (1%). Permanent discontinuation due to an adverse reaction occurred in 31% of patients; KEYTRUDA only (13%), axitinib only (13%), and the combination (8%); the most common were hepatotoxicity (13%), diarrhea/colitis (1.9%), acute kidney injury (1.6%), and cerebrovascular accident (1.2%). The most common adverse reactions (≥20%) were diarrhea (56%), fatigue/asthenia (52%), hypertension (48%), hepatotoxicity (39%), hypothyroidism (35%), decreased appetite (30%), palmar-plantar erythrodysesthesia (28%), nausea (28%), stomatitis/mucosal inflammation (27%), dysphonia (25%), rash (25%), cough (21%), and constipation (21%).
In KEYNOTE-564, when KEYTRUDA was administered as a single agent for the adjuvant treatment of renal cell carcinoma, serious adverse reactions occurred in 20% of patients receiving KEYTRUDA; the serious adverse reactions (≥1%) were acute kidney injury, adrenal insufficiency, pneumonia, colitis, and diabetic ketoacidosis (1% each). Fatal adverse reactions occurred in 0.2% including 1 case of pneumonia. Discontinuation of KEYTRUDA due to adverse reactions occurred in 21% of 488 patients; the most common (≥1%) were increased ALT (1.6%), colitis (1%), and adrenal insufficiency (1%). The most common adverse reactions (≥20%) were musculoskeletal pain (41%), fatigue (40%), rash (30%), diarrhea (27%), pruritus (23%), and hypothyroidism (21%).
In KEYNOTE-868, when KEYTRUDA was administered in combination with chemotherapy (paclitaxel and carboplatin) to patients with advanced or recurrent endometrial carcinoma (n=382), serious adverse reactions occurred in 35% of patients receiving KEYTRUDA in combination with chemotherapy, compared to 19% of patients receiving placebo in combination with chemotherapy (n=377). Fatal adverse reactions occurred in 1.6% of patients receiving KEYTRUDA in combination with chemotherapy, including COVID-19 (0.5%) and cardiac arrest (0.3%). KEYTRUDA was discontinued for an adverse reaction in 14% of patients. Adverse reactions occurring in patients treated with KEYTRUDA and chemotherapy were generally similar to those observed with KEYTRUDA alone or chemotherapy alone, with the exception of rash (33% all Grades; 2.9% Grades 3-4).
Adverse reactions occurring in patients with MSI-H or dMMR endometrial carcinoma who received KEYTRUDA as a single agent were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a single agent.
Adverse reactions occurring in patients with TMB-H cancer were similar to those occurring in patients with other solid tumors who received KEYTRUDA as a single agent.
Adverse reactions occurring in patients with recurrent or metastatic cSCC or locally advanced cSCC were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-522, when KEYTRUDA was administered with neoadjuvant chemotherapy (carboplatin and paclitaxel followed by doxorubicin or epirubicin and cyclophosphamide) followed by surgery and continued adjuvant treatment with KEYTRUDA as a single agent (n=778) to patients with newly diagnosed, previously untreated, high-risk early-stage TNBC, fatal adverse reactions occurred in 0.9% of patients, including 1 each of adrenal crisis, autoimmune encephalitis, hepatitis, pneumonia, pneumonitis, pulmonary embolism, and sepsis in association with multiple organ dysfunction syndrome and myocardial infarction. Serious adverse reactions occurred in 44% of patients receiving KEYTRUDA; those ≥2% were febrile neutropenia (15%), pyrexia (3.7%), anemia (2.6%), and neutropenia (2.2%). KEYTRUDA was discontinued in 20% of patients due to adverse reactions. The most common reactions (≥1%) resulting in permanent discontinuation were increased ALT (2.7%), increased AST (1.5%), and rash (1%). The most common adverse reactions (≥20%) in patients receiving KEYTRUDA were fatigue (70%), nausea (67%), alopecia (61%), rash (52%), constipation (42%), diarrhea and peripheral neuropathy (41% each), stomatitis (34%), vomiting (31%), headache (30%), arthralgia (29%), pyrexia (28%), cough (26%), abdominal pain (24%), decreased appetite (23%), insomnia (21%), and myalgia (20%).
In KEYNOTE-355, when KEYTRUDA and chemotherapy (paclitaxel, paclitaxel protein-bound, or gemcitabine and carboplatin) were administered to patients with locally recurrent unresectable or metastatic TNBC who had not been previously treated with chemotherapy in the metastatic setting (n=596), fatal adverse reactions occurred in 2.5% of patients, including cardio-respiratory arrest (0.7%) and septic shock (0.3%). Serious adverse reactions occurred in 30% of patients receiving KEYTRUDA in combination with chemotherapy; the serious reactions in ≥2% were pneumonia (2.9%), anemia (2.2%), and thrombocytopenia (2%). KEYTRUDA was discontinued in 11% of patients due to adverse reactions. The most common reactions resulting in permanent discontinuation (≥1%) were increased ALT (2.2%), increased AST (1.5%), and pneumonitis (1.2%). The most common adverse reactions (≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were fatigue (48%), nausea (44%), alopecia (34%), diarrhea and constipation (28% each), vomiting and rash (26% each), cough (23%), decreased appetite (21%), and headache (20%).
Lactation
Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment and for 4 months after the last dose.
Pediatric Use
In KEYNOTE-051, 173 pediatric patients (65 pediatric patients aged 6 months to younger than 12 years and 108 pediatric patients aged 12 years to 17 years) were administered KEYTRUDA 2 mg/kg every 3 weeks. The median duration of exposure was 2.1 months (range: 1 day to 25 months).
Adverse reactions that occurred at a ≥10% higher rate in pediatric patients when compared to adults were pyrexia (33%), leukopenia (30%), vomiting (29%), neutropenia (28%), headache (25%), abdominal pain (23%), thrombocytopenia (22%), Grade 3 anemia (17%), decreased lymphocyte count (13%), and decreased white blood cell count (11%).
Geriatric Use
Of the 564 patients with locally advanced or metastatic urothelial cancer treated with KEYTRUDA in combination with enfortumab vedotin, 44% (n=247) were 65-74 years and 26% (n=144) were 75 years or older. No overall differences in safety or effectiveness were observed between patients 65 years of age or older and younger patients. Patients 75 years of age or older treated with KEYTRUDA in combination with enfortumab vedotin experienced a higher incidence of fatal adverse reactions than younger patients. The incidence of fatal adverse reactions was 4% in patients younger than 75 and 7% in patients 75 years or older.
Additional Selected KEYTRUDA Indications in the U.S.
Melanoma
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic melanoma.
KEYTRUDA is indicated for the adjuvant treatment of adult and pediatric (12 years and older) patients with Stage IIB, IIC, or III melanoma following complete resection.
Malignant Pleural Mesothelioma
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of adult patients with unresectable advanced or metastatic malignant pleural mesothelioma (MPM).
Head and Neck Squamous Cell Cancer
KEYTRUDA, in combination with platinum and fluorouracil (FU), is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent head and neck squamous cell carcinoma (HNSCC).
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent HNSCC whose tumors express PD-L1 [Combined Positive Score (CPS) ≥1] as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic HNSCC with disease progression on or after platinum-containing chemotherapy.
Classical Hodgkin Lymphoma
KEYTRUDA is indicated for the treatment of adult patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
KEYTRUDA is indicated for the treatment of pediatric patients with refractory cHL, or cHL that has relapsed after 2 or more lines of therapy.
Primary Mediastinal Large B-Cell Lymphoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after 2 or more prior lines of therapy. KEYTRUDA is not recommended for treatment of patients with PMBCL who require urgent cytoreductive therapy.
Urothelial Cancer
KEYTRUDA, in combination with enfortumab vedotin, is indicated for the treatment of adult patients with locally advanced or metastatic urothelial cancer.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma:
who are not eligible for any platinum-containing chemotherapy, or
who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, non-muscle invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy.
Microsatellite Instability-High or Mismatch Repair Deficient Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
Microsatellite Instability-High or Mismatch Repair Deficient Colorectal Cancer
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic MSI-H or dMMR colorectal cancer (CRC) as determined by an FDA-approved test.
Gastric Cancer
KEYTRUDA, in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy, is indicated for the first-line treatment of adults with locally advanced unresectable or metastatic HER2-positive gastric or gastroesophageal junction (GEJ) adenocarcinoma whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
KEYTRUDA, in combination with fluoropyrimidine- and platinum-containing chemotherapy, is indicated for the first-line treatment of adults with locally advanced unresectable or metastatic HER2-negative gastric or gastroesophageal junction (GEJ) adenocarcinoma.
Esophageal Cancer
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic esophageal or gastroesophageal junction (GEJ) (tumors with epicenter 1 to 5 centimeters above the GEJ) carcinoma that is not amenable to surgical resection or definitive chemoradiation either:
in combination with platinum- and fluoropyrimidine-based chemotherapy, or
as a single agent after one or more prior lines of systemic therapy for patients with tumors of squamous cell histology that express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Cervical Cancer
KEYTRUDA, in combination with chemoradiotherapy (CRT), is indicated for the treatment of patients with FIGO 2014 Stage III-IVA cervical cancer.
KEYTRUDA, in combination with chemotherapy, with or without bevacizumab, is indicated for the treatment of patients with persistent, recurrent, or metastatic cervical cancer whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
Hepatocellular Carcinoma
KEYTRUDA is indicated for the treatment of patients with hepatocellular carcinoma (HCC) secondary to hepatitis B who have received prior systemic therapy other than a PD-1/PD-L1-containing regimen.
Biliary Tract Cancer
KEYTRUDA, in combination with gemcitabine and cisplatin, is indicated for the treatment of patients with locally advanced unresectable or metastatic biliary tract cancer (BTC).
Merkel Cell Carcinoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with recurrent locally advanced or metastatic Merkel cell carcinoma (MCC).
Renal Cell Carcinoma
KEYTRUDA, in combination with axitinib, is indicated for the first-line treatment of adult patients with advanced renal cell carcinoma (RCC).
KEYTRUDA is indicated for the adjuvant treatment of patients with RCC at intermediate-high or high risk of recurrence following nephrectomy or following nephrectomy and resection of metastatic lesions.
Endometrial Carcinoma
KEYTRUDA, in combination with carboplatin and paclitaxel, followed by KEYTRUDA as a single agent, is indicated for the treatment of adult patients with primary advanced or recurrent endometrial carcinoma.
KEYTRUDA, as a single agent, is indicated for the treatment of adult patients with advanced endometrial carcinoma that is MSI-H or dMMR, as determined by an FDA-approved test, who have disease progression following prior systemic therapy in any setting and are not candidates for curative surgery or radiation.
Tumor Mutational Burden-High Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. The safety and effectiveness of KEYTRUDA in pediatric patients with TMB-H central nervous system cancers have not been established.
Cutaneous Squamous Cell Carcinoma
KEYTRUDA is indicated for the treatment of patients with recurrent or metastatic cutaneous squamous cell carcinoma (cSCC) or locally advanced cSCC that is not curable by surgery or radiation.
Triple-Negative Breast Cancer
KEYTRUDA is indicated for the treatment of patients with high-risk early-stage triple-negative breast cancer (TNBC) in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
KEYTRUDA, in combination with chemotherapy, is indicated for the treatment of patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Merck’s focus on cancer
Every day, we follow the science as we work to discover innovations that can help patients, no matter what stage of cancer they have. As a leading oncology company, we are pursuing research where scientific opportunity and medical need converge, underpinned by our diverse pipeline of more than 25 novel mechanisms. With one of the largest clinical development programs across more than 30 tumor types, we strive to advance breakthrough science that will shape the future of oncology. By addressing barriers to clinical trial participation, screening and treatment, we work with urgency to reduce disparities and help ensure patients have access to high-quality cancer care. Our unwavering commitment is what will bring us closer to our goal of bringing life to more patients with cancer. For more information, visit
https://www.merck.com/research/oncology
.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit
www.merck.com
and connect with us on
X (formerly Twitter)
,
Facebook
,
Instagram
,
YouTube
and
LinkedIn
.
Forward-Looking Statement of Merck & Co., Inc., Rahway, N.J., USA
This news release of Merck & Co., Inc., Rahway, N.J., USA (the “company”) includes “forward-looking statements” within the meaning of the safe harbor provisions of the U.S. Private Securities Litigation Reform Act of 1995. These statements are based upon the current beliefs and expectations of the company’s management and are subject to significant risks and uncertainties. There can be no guarantees with respect to pipeline candidates that the candidates will receive the necessary regulatory approvals or that they will prove to be commercially successful. If underlying assumptions prove inaccurate or risks or uncertainties materialize, actual results may differ materially from those set forth in the forward-looking statements.
Risks and uncertainties include but are not limited to, general industry conditions and competition; general economic factors, including interest rate and currency exchange rate fluctuations; the impact of pharmaceutical industry regulation and health care legislation in the United States and internationally; global trends toward health care cost containment; technological advances, new products and patents attained by competitors; challenges inherent in new product development, including obtaining regulatory approval; the company’s ability to accurately predict future market conditions; manufacturing difficulties or delays; financial instability of international economies and sovereign risk; dependence on the effectiveness of the company’s patents and other protections for innovative products; and the exposure to litigation, including patent litigation, and/or regulatory actions.
The company undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future events or otherwise. Additional factors that could cause results to differ materially from those described in the forward-looking statements can be found in the company’s Annual Report on Form 10-K for the year ended December 31, 2024 and the company’s other filings with the Securities and Exchange Commission (SEC) available at the SEC’s Internet site (
www.sec.gov
)
Please see Prescribing Information for KEYTRUDA (pembrolizumab) at
http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf
and Medication Guide for KEYTRUDA at
http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_mg.pdf
.
Media Contacts:
Olivia Finucane
+44 7881 262476
Diane Foley
(862) 260-0060
Investor Contacts:
Peter Dannenbaum
(732) 594-1579
Steven Graziano
(732) 594-1583
Source: Merck & Co., Inc.
Clinical ResultPhase 3Phase 2
25 Feb 2025
February 25, 2025 7:45 am ET
Acceptance based on results from the KEYNOTE-689 trial: the first Phase 3 trial to demonstrate significant improvement in event-free survival in the neoadjuvant and adjuvant setting for an anti-PD-1 therapy in earlier stages of head and neck squamous cell carcinoma
RAHWAY, N.J.--(BUSINESS WIRE)--
Merck (NYSE: MRK), known as MSD outside of the United States and Canada, today announced the U.S. Food and Drug Administration (FDA) has accepted for priority review a new supplemental Biologics License Application (sBLA) seeking approval for KEYTRUDA
®
(pembrolizumab), Merck’s anti-PD-1 therapy, for the treatment of patients with resectable locally advanced head and neck squamous cell carcinoma (LA-HNSCC) as neoadjuvant treatment, then continued as adjuvant treatment in combination with standard of care radiotherapy with or without cisplatin and then as a single agent. The FDA has set a Prescription Drug User Fee Act (PDUFA), or target action, date of June 23, 2025.
The sBLA is based on data from the Phase 3 KEYNOTE-689 trial. Results from a pre-specified first interim analysis, which will be presented at an upcoming medical meeting, showed that in patients with resectable LA-HNSCC, the KEYTRUDA perioperative treatment regimen demonstrated a statistically significant and clinically meaningful improvement in event-free survival (EFS) compared to adjuvant radiotherapy (with or without cisplatin) alone. The study also showed a statistically significant improvement in major pathological response (mPR), a key secondary endpoint, for patients in the KEYTRUDA arm compared with adjuvant radiotherapy alone. The safety profile of KEYTRUDA was consistent with that observed in previously reported studies; no new safety signals were identified.
"The standard of care for patients with resectable locally advanced head and neck squamous cell carcinoma has remained the same for over two decades, representing a significant unmet need for new treatment options,” said Dr. Marjorie Green, senior vice president and head of oncology, global clinical development, Merck Research Laboratories. “Based on the compelling results of the KEYNOTE-689 trial, we hope to reduce the risk of recurrence and disease progression in earlier stages of disease. We look forward to working with the FDA to potentially bring KEYTRUDA to these patients as soon as possible.”
This review is being conducted under Project Orbis, an initiative of the FDA Oncology Center of Excellence that provides a framework for coordinated submission and review of oncology drugs among its international partners. Health authorities in Israel, Canada, Australia, Singapore, Brazil and Switzerland will review this application as part of Project Orbis.
KEYTRUDA is currently approved as monotherapy and in combination regimens for appropriate patients with metastatic or with unresectable, recurrent HNSCC in the U.S., Europe, China, Japan and other countries around the world. For more information, please see the “Selected KEYTRUDA
®
(pembrolizumab) Indications in the U.S.” section below.
About KEYNOTE-689
KEYNOTE-689 is a randomized, active-controlled, open-label Phase 3 trial (ClinicalTrials.gov,
NCT03765918
) evaluating KEYTRUDA as neoadjuvant treatment and KEYTRUDA in combination with standard of care radiotherapy (with or without cisplatin) as adjuvant treatment in treatment-naïve patients with newly diagnosed, stage III or IVA resectable, locally advanced, head and neck squamous cell carcinoma. Efficacy outcomes are classified by programmed cell death ligand 1 (PD-L1) combined positive score (CPS) status. The primary endpoint is EFS, and key secondary endpoints include overall survival, major pathological response, pathological complete response and safety. The study enrolled an estimated 704 patients who were randomized (1:1) to receive either:
KEYTRUDA (200 mg intravenously [IV] every three weeks [Q3W] for two cycles) as neoadjuvant therapy prior to surgery, followed by either KEYTRUDA (200 mg IV Q3W for 15 cycles) plus standard of care radiotherapy with cisplatin (100 mg/m
2
IV Q3W for three cycles) as adjuvant therapy following surgery for high-risk patients or KEYTRUDA (200 mg IV Q3W for 15 cycles) plus standard of care radiotherapy without cisplatin as adjuvant therapy following surgery for low-risk patients; or
No neoadjuvant therapy prior to surgery, followed by either standard of care radiotherapy with cisplatin (100 mg/m
2
IV Q3W for three cycles) as adjuvant therapy following surgery for high-risk patients or standard of care radiotherapy without cisplatin as adjuvant therapy following surgery for low-risk patients.
About head and neck cancer
Head and neck cancer describes a number of different tumors that develop in or around the throat, larynx, nose, sinuses and mouth. Most head and neck cancers are squamous cell carcinomas that begin in the flat, squamous cells that make up the thin surface layer of the structures in the head and neck. Locally advanced head and neck squamous cell carcinoma (LA-HNSCC) is cancer that has grown outside the original location, but has not yet spread to distant parts of the body. There are several factors that greatly increase the risk of developing head and neck cancer, including tobacco and alcohol use and human papillomavirus (HPV). It is estimated there were more than 891,500 new cases of head and neck cancer diagnosed and over 458,100 deaths from the disease in 2022 globally. In the U.S., it is estimated there will be more than 58,450 new cases of head and neck cancer diagnosed and more than 12,230 deaths from the disease in 2024.
About Merck’s early-stage cancer clinical program
Finding cancer at an earlier stage may give patients a greater chance of long-term survival. Many cancers are considered most treatable and potentially curable in their earliest stage of disease. Building on the strong understanding of the role of KEYTRUDA in later-stage cancers, Merck is evaluating our portfolio of medicines and pipeline candidates in earlier disease states, with approximately 30 ongoing registrational studies across multiple types of cancer.
About KEYTRUDA
®
(pembrolizumab) injection, 100 mg
KEYTRUDA is an anti-programmed death receptor-1 (PD-1) therapy that works by increasing the ability of the body’s immune system to help detect and fight tumor cells. KEYTRUDA is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD- L1 and PD-L2, thereby activating T lymphocytes which may affect both tumor cells and healthy cells.
Merck has the industry’s largest immuno-oncology clinical research program. There are currently more than 1,600 trials studying KEYTRUDA across a wide variety of cancers and treatment settings. The KEYTRUDA clinical program seeks to understand the role of KEYTRUDA across cancers and the factors that may predict a patient's likelihood of benefitting from treatment with KEYTRUDA, including exploring several different biomarkers.
Selected KEYTRUDA
®
(pembrolizumab) Indications in the U.S.
Head and Neck Squamous Cell Cancer
KEYTRUDA, in combination with platinum and fluorouracil (FU), is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent head and neck squamous cell carcinoma (HNSCC).
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with metastatic or with unresectable, recurrent HNSCC whose tumors express PD-L1 [Combined Positive Score (CPS) ≥1] as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic HNSCC with disease progression on or after platinum-containing chemotherapy.
See additional selected KEYTRUDA indications in the U.S. after the Selected Important Safety Information.
Selected Important Safety Information for KEYTRUDA
Severe and Fatal Immune-Mediated Adverse Reactions
KEYTRUDA is a monoclonal antibody that belongs to a class of drugs that bind to either the programmed death receptor-1 (PD-1) or the programmed death ligand 1 (PD-L1), blocking the PD-1/PD-L1 pathway, thereby removing inhibition of the immune response, potentially breaking peripheral tolerance and inducing immune-mediated adverse reactions. Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue, can affect more than one body system simultaneously, and can occur at any time after starting treatment or after discontinuation of treatment. Important immune-mediated adverse reactions listed here may not include all possible severe and fatal immune-mediated adverse reactions.
Monitor patients closely for symptoms and signs that may be clinical manifestations of underlying immune-mediated adverse reactions. Early identification and management are essential to ensure safe use of anti–PD-1/PD-L1 treatments. Evaluate liver enzymes, creatinine, and thyroid function at baseline and periodically during treatment. For patients with TNBC treated with KEYTRUDA in the neoadjuvant setting, monitor blood cortisol at baseline, prior to surgery, and as clinically indicated. In cases of suspected immune-mediated adverse reactions, initiate appropriate workup to exclude alternative etiologies, including infection. Institute medical management promptly, including specialty consultation as appropriate.
Withhold or permanently discontinue KEYTRUDA depending on severity of the immune-mediated adverse reaction. In general, if KEYTRUDA requires interruption or discontinuation, administer systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or equivalent) until improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider administration of other systemic immunosuppressants in patients whose adverse reactions are not controlled with corticosteroid therapy.
Immune-Mediated Pneumonitis
KEYTRUDA can cause immune-mediated pneumonitis. The incidence is higher in patients who have received prior thoracic radiation. Immune-mediated pneumonitis occurred in 3.4% (94/2799) of patients receiving KEYTRUDA, including fatal (0.1%), Grade 4 (0.3%), Grade 3 (0.9%), and Grade 2 (1.3%) reactions. Systemic corticosteroids were required in 67% (63/94) of patients. Pneumonitis led to permanent discontinuation of KEYTRUDA in 1.3% (36) and withholding in 0.9% (26) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 23% had recurrence. Pneumonitis resolved in 59% of the 94 patients.
Pneumonitis occurred in 8% (31/389) of adult patients with cHL receiving KEYTRUDA as a single agent, including Grades 3-4 in 2.3% of patients. Patients received high-dose corticosteroids for a median duration of 10 days (range: 2 days to 53 months). Pneumonitis rates were similar in patients with and without prior thoracic radiation. Pneumonitis led to discontinuation of KEYTRUDA in 5.4% (21) of patients. Of the patients who developed pneumonitis, 42% interrupted KEYTRUDA, 68% discontinued KEYTRUDA, and 77% had resolution.
Pneumonitis occurred in 7% (41/580) of adult patients with resected NSCLC who received KEYTRUDA as a single agent for adjuvant treatment of NSCLC, including fatal (0.2%), Grade 4 (0.3%), and Grade 3 (1%) adverse reactions. Patients received high-dose corticosteroids for a median duration of 10 days (range: 1 day to 2.3 months). Pneumonitis led to discontinuation of KEYTRUDA in 26 (4.5%) of patients. Of the patients who developed pneumonitis, 54% interrupted KEYTRUDA, 63% discontinued KEYTRUDA, and 71% had resolution.
Immune-Mediated Colitis
KEYTRUDA can cause immune-mediated colitis, which may present with diarrhea. Cytomegalovirus infection/reactivation has been reported in patients with corticosteroid-refractory immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup to exclude alternative etiologies. Immune-mediated colitis occurred in 1.7% (48/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (1.1%), and Grade 2 (0.4%) reactions. Systemic corticosteroids were required in 69% (33/48); additional immunosuppressant therapy was required in 4.2% of patients. Colitis led to permanent discontinuation of KEYTRUDA in 0.5% (15) and withholding in 0.5% (13) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 23% had recurrence. Colitis resolved in 85% of the 48 patients.
Hepatotoxicity and Immune-Mediated Hepatitis
KEYTRUDA as a Single Agent
KEYTRUDA can cause immune-mediated hepatitis. Immune-mediated hepatitis occurred in 0.7% (19/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.4%), and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 68% (13/19) of patients; additional immunosuppressant therapy was required in 11% of patients. Hepatitis led to permanent discontinuation of KEYTRUDA in 0.2% (6) and withholding in 0.3% (9) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, none had recurrence. Hepatitis resolved in 79% of the 19 patients.
KEYTRUDA With Axitinib
KEYTRUDA in combination with axitinib can cause hepatic toxicity. Monitor liver enzymes before initiation of and periodically throughout treatment. Consider monitoring more frequently as compared to when the drugs are administered as single agents. For elevated liver enzymes, interrupt KEYTRUDA and axitinib, and consider administering corticosteroids as needed. With the combination of KEYTRUDA and axitinib, Grades 3 and 4 increased alanine aminotransferase (ALT) (20%) and increased aspartate aminotransferase (AST) (13%) were seen at a higher frequency compared to KEYTRUDA alone. Fifty-nine percent of the patients with increased ALT received systemic corticosteroids. In patients with ALT ≥3 times upper limit of normal (ULN) (Grades 2-4, n=116), ALT resolved to Grades 0-1 in 94%. Among the 92 patients who were rechallenged with either KEYTRUDA (n=3) or axitinib (n=34) administered as a single agent or with both (n=55), recurrence of ALT ≥3 times ULN was observed in 1 patient receiving KEYTRUDA, 16 patients receiving axitinib, and 24 patients receiving both. All patients with a recurrence of ALT ≥3 ULN subsequently recovered from the event.
Immune-Mediated Endocrinopathies
Adrenal Insufficiency
KEYTRUDA can cause primary or secondary adrenal insufficiency. For Grade 2 or higher, initiate symptomatic treatment, including hormone replacement as clinically indicated. Withhold KEYTRUDA depending on severity. Adrenal insufficiency occurred in 0.8% (22/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.3%), and Grade 2 (0.3%) reactions. Systemic corticosteroids were required in 77% (17/22) of patients; of these, the majority remained on systemic corticosteroids. Adrenal insufficiency led to permanent discontinuation of KEYTRUDA in <0.1% (1) and withholding in 0.3% (8) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Hypophysitis
KEYTRUDA can cause immune-mediated hypophysitis. Hypophysitis can present with acute symptoms associated with mass effect such as headache, photophobia, or visual field defects. Hypophysitis can cause hypopituitarism. Initiate hormone replacement as indicated. Withhold or permanently discontinue KEYTRUDA depending on severity. Hypophysitis occurred in 0.6% (17/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.3%), and Grade 2 (0.2%) reactions. Systemic corticosteroids were required in 94% (16/17) of patients; of these, the majority remained on systemic corticosteroids. Hypophysitis led to permanent discontinuation of KEYTRUDA in 0.1% (4) and withholding in 0.3% (7) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Thyroid Disorders
KEYTRUDA can cause immune-mediated thyroid disorders. Thyroiditis can present with or without endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate hormone replacement for hypothyroidism or institute medical management of hyperthyroidism as clinically indicated. Withhold or permanently discontinue KEYTRUDA depending on severity. Thyroiditis occurred in 0.6% (16/2799) of patients receiving KEYTRUDA, including Grade 2 (0.3%). None discontinued, but KEYTRUDA was withheld in <0.1% (1) of patients.
Hyperthyroidism occurred in 3.4% (96/2799) of patients receiving KEYTRUDA, including Grade 3 (0.1%) and Grade 2 (0.8%). It led to permanent discontinuation of KEYTRUDA in <0.1% (2) and withholding in 0.3% (7) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement. Hypothyroidism occurred in 8% (237/2799) of patients receiving KEYTRUDA, including Grade 3 (0.1%) and Grade 2 (6.2%). It led to permanent discontinuation of KEYTRUDA in <0.1% (1) and withholding in 0.5% (14) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement. The majority of patients with hypothyroidism required long-term thyroid hormone replacement. The incidence of new or worsening hypothyroidism was higher in 1185 patients with HNSCC, occurring in 16% of patients receiving KEYTRUDA as a single agent or in combination with platinum and FU, including Grade 3 (0.3%) hypothyroidism. The incidence of new or worsening hypothyroidism was higher in 389 adult patients with cHL (17%) receiving KEYTRUDA as a single agent, including Grade 1 (6.2%) and Grade 2 (10.8%) hypothyroidism. The incidence of new or worsening hyperthyroidism was higher in 580 patients with resected NSCLC, occurring in 11% of patients receiving KEYTRUDA as a single agent as adjuvant treatment, including Grade 3 (0.2%) hyperthyroidism. The incidence of new or worsening hypothyroidism was higher in 580 patients with resected NSCLC, occurring in 22% of patients receiving KEYTRUDA as a single agent as adjuvant treatment (KEYNOTE-091), including Grade 3 (0.3%) hypothyroidism.
Type 1 Diabetes Mellitus (DM), Which Can Present With Diabetic Ketoacidosis
Monitor patients for hyperglycemia or other signs and symptoms of diabetes. Initiate treatment with insulin as clinically indicated. Withhold KEYTRUDA depending on severity. Type 1 DM occurred in 0.2% (6/2799) of patients receiving KEYTRUDA. It led to permanent discontinuation in <0.1% (1) and withholding of KEYTRUDA in <0.1% (1) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement.
Immune-Mediated Nephritis With Renal Dysfunction
KEYTRUDA can cause immune-mediated nephritis. Immune-mediated nephritis occurred in 0.3% (9/2799) of patients receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.1%), and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 89% (8/9) of patients. Nephritis led to permanent discontinuation of KEYTRUDA in 0.1% (3) and withholding in 0.1% (3) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, none had recurrence. Nephritis resolved in 56% of the 9 patients.
Immune-Mediated Dermatologic Adverse Reactions
KEYTRUDA can cause immune-mediated rash or dermatitis. Exfoliative dermatitis, including Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms, and toxic epidermal necrolysis, has occurred with anti– PD-1/PD-L1 treatments. Topical emollients and/or topical corticosteroids may be adequate to treat mild to moderate nonexfoliative rashes. Withhold or permanently discontinue KEYTRUDA depending on severity. Immune-mediated dermatologic adverse reactions occurred in 1.4% (38/2799) of patients receiving KEYTRUDA, including Grade 3 (1%) and Grade 2 (0.1%) reactions. Systemic corticosteroids were required in 40% (15/38) of patients. These reactions led to permanent discontinuation in 0.1% (2) and withholding of KEYTRUDA in 0.6% (16) of patients. All patients who were withheld reinitiated KEYTRUDA after symptom improvement; of these, 6% had recurrence. The reactions resolved in 79% of the 38 patients.
Other Immune-Mediated Adverse Reactions
The following clinically significant immune-mediated adverse reactions occurred at an incidence of <1% (unless otherwise noted) in patients who received KEYTRUDA or were reported with the use of other anti–PD-1/PD-L1 treatments. Severe or fatal cases have been reported for some of these adverse reactions. Cardiac/Vascular: Myocarditis, pericarditis, vasculitis; Nervous System: Meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis (including exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune neuropathy; Ocular: Uveitis, iritis and other ocular inflammatory toxicities can occur. Some cases can be associated with retinal detachment. Various grades of visual impairment, including blindness, can occur. If uveitis occurs in combination with other immune-mediated adverse reactions, consider a Vogt-Koyanagi-Harada-like syndrome, as this may require treatment with systemic steroids to reduce the risk of permanent vision loss; Gastrointestinal: Pancreatitis, to include increases in serum amylase and lipase levels, gastritis, duodenitis; Musculoskeletal and Connective Tissue: Myositis/polymyositis, rhabdomyolysis (and associated sequelae, including renal failure), arthritis (1.5%), polymyalgia rheumatica; Endocrine: Hypoparathyroidism; Hematologic/Immune: Hemolytic anemia, aplastic anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid organ transplant rejection, other transplant (including corneal graft) rejection.
Infusion-Related Reactions
KEYTRUDA can cause severe or life-threatening infusion-related reactions, including hypersensitivity and anaphylaxis, which have been reported in 0.2% of 2799 patients receiving KEYTRUDA. Monitor for signs and symptoms of infusion-related reactions. Interrupt or slow the rate of infusion for Grade 1 or Grade 2 reactions. For Grade 3 or Grade 4 reactions, stop infusion and permanently discontinue KEYTRUDA.
Complications of Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)
Fatal and other serious complications can occur in patients who receive allogeneic HSCT before or after anti–PD-1/PD-L1 treatments. Transplant-related complications include hyperacute graft-versus-host disease (GVHD), acute and chronic GVHD, hepatic veno-occlusive disease after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause). These complications may occur despite intervening therapy between anti–PD-1/PD-L1 treatments and allogeneic HSCT. Follow patients closely for evidence of these complications and intervene promptly. Consider the benefit vs risks of using anti–PD-1/PD-L1 treatments prior to or after an allogeneic HSCT.
Increased Mortality in Patients With Multiple Myeloma
In trials in patients with multiple myeloma, the addition of KEYTRUDA to a thalidomide analogue plus dexamethasone resulted in increased mortality. Treatment of these patients with an anti–PD-1/PD-L1 treatment in this combination is not recommended outside of controlled trials.
Embryofetal Toxicity
Based on its mechanism of action, KEYTRUDA can cause fetal harm when administered to a pregnant woman. Advise women of this potential risk. In females of reproductive potential, verify pregnancy status prior to initiating KEYTRUDA and advise them to use effective contraception during treatment and for 4 months after the last dose.
Adverse Reactions
In KEYNOTE-006, KEYTRUDA was discontinued due to adverse reactions in 9% of 555 patients with advanced melanoma; adverse reactions leading to permanent discontinuation in more than one patient were colitis (1.4%), autoimmune hepatitis (0.7%), allergic reaction (0.4%), polyneuropathy (0.4%), and cardiac failure (0.4%). The most common adverse reactions (≥20%) with KEYTRUDA were fatigue (28%), diarrhea (26%), rash (24%), and nausea (21%).
In KEYNOTE-054, when KEYTRUDA was administered as a single agent to patients with stage III melanoma, KEYTRUDA was permanently discontinued due to adverse reactions in 14% of 509 patients; the most common (≥1%) were pneumonitis (1.4%), colitis (1.2%), and diarrhea (1%). Serious adverse reactions occurred in 25% of patients receiving KEYTRUDA. The most common adverse reaction (≥20%) with KEYTRUDA was diarrhea (28%). In KEYNOTE-716, when KEYTRUDA was administered as a single agent to patients with stage IIB or IIC melanoma, adverse reactions occurring in patients with stage IIB or IIC melanoma were similar to those occurring in 1011 patients with stage III melanoma from KEYNOTE-054.
In KEYNOTE-189, when KEYTRUDA was administered with pemetrexed and platinum chemotherapy in metastatic nonsquamous NSCLC, KEYTRUDA was discontinued due to adverse reactions in 20% of 405 patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA were pneumonitis (3%) and acute kidney injury (2%). The most common adverse reactions (≥20%) with KEYTRUDA were nausea (56%), fatigue (56%), constipation (35%), diarrhea (31%), decreased appetite (28%), rash (25%), vomiting (24%), cough (21%), dyspnea (21%), and pyrexia (20%).
In KEYNOTE-407, when KEYTRUDA was administered with carboplatin and either paclitaxel or paclitaxel protein-bound in metastatic squamous NSCLC, KEYTRUDA was discontinued due to adverse reactions in 15% of 101 patients. The most frequent serious adverse reactions reported in at least 2% of patients were febrile neutropenia, pneumonia, and urinary tract infection. Adverse reactions observed in KEYNOTE-407 were similar to those observed in KEYNOTE-189 with the exception that increased incidences of alopecia (47% vs 36%) and peripheral neuropathy (31% vs 25%) were observed in the KEYTRUDA and chemotherapy arm compared to the placebo and chemotherapy arm in KEYNOTE-407.
In KEYNOTE-042, KEYTRUDA was discontinued due to adverse reactions in 19% of 636 patients with advanced NSCLC; the most common were pneumonitis (3%), death due to unknown cause (1.6%), and pneumonia (1.4%). The most frequent serious adverse reactions reported in at least 2% of patients were pneumonia (7%), pneumonitis (3.9%), pulmonary embolism (2.4%), and pleural effusion (2.2%). The most common adverse reaction (≥20%) was fatigue (25%).
In KEYNOTE-010, KEYTRUDA monotherapy was discontinued due to adverse reactions in 8% of 682 patients with metastatic NSCLC; the most common was pneumonitis (1.8%). The most common adverse reactions (≥20%) were decreased appetite (25%), fatigue (25%), dyspnea (23%), and nausea (20%).
In KEYNOTE-671, adverse reactions occurring in patients with resectable NSCLC receiving KEYTRUDA in combination with platinum-containing chemotherapy, given as neoadjuvant treatment and continued as single-agent adjuvant treatment, were generally similar to those occurring in patients in other clinical trials across tumor types receiving KEYTRUDA in combination with chemotherapy.
The most common adverse reactions (reported in ≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were fatigue/asthenia, nausea, constipation, diarrhea, decreased appetite, rash, vomiting, cough, dyspnea, pyrexia, alopecia, peripheral neuropathy, mucosal inflammation, stomatitis, headache, weight loss, abdominal pain, arthralgia, myalgia, insomnia, palmar-plantar erythrodysesthesia, urinary tract infection, and hypothyroidism.
In the neoadjuvant phase of KEYNOTE-671, when KEYTRUDA was administered in combination with platinum-containing chemotherapy as neoadjuvant treatment, serious adverse reactions occurred in 34% of 396 patients. The most frequent (≥2%) serious adverse reactions were pneumonia (4.8%), venous thromboembolism (3.3%), and anemia (2%). Fatal adverse reactions occurred in 1.3% of patients, including death due to unknown cause (0.8%), sepsis (0.3%), and immune-mediated lung disease (0.3%). Permanent discontinuation of any study drug due to an adverse reaction occurred in 18% of patients who received KEYTRUDA in combination with platinum-containing chemotherapy; the most frequent adverse reactions (≥1%) that led to permanent discontinuation of any study drug were acute kidney injury (1.8%), interstitial lung disease (1.8%), anemia (1.5%), neutropenia (1.5%), and pneumonia (1.3%).
Of the KEYTRUDA-treated patients who received neoadjuvant treatment, 6% of 396 patients did not receive surgery due to adverse reactions. The most frequent (≥1%) adverse reaction that led to cancellation of surgery in the KEYTRUDA arm was interstitial lung disease (1%).
In the adjuvant phase of KEYNOTE-671, when KEYTRUDA was administered as a single agent as adjuvant treatment, serious adverse reactions occurred in 14% of 290 patients. The most frequent serious adverse reaction was pneumonia (3.4%). One fatal adverse reaction of pulmonary hemorrhage occurred. Permanent discontinuation of KEYTRUDA due to an adverse reaction occurred in 12% of patients who received KEYTRUDA as a single agent, given as adjuvant treatment; the most frequent adverse reactions (≥1%) that led to permanent discontinuation of KEYTRUDA were diarrhea (1.7%), interstitial lung disease (1.4%), increased aspartate aminotransferase (1%), and musculoskeletal pain (1%).
Adverse reactions observed in KEYNOTE-091 were generally similar to those occurring in other patients with NSCLC receiving KEYTRUDA as a single agent, with the exception of hypothyroidism (22%), hyperthyroidism (11%), and pneumonitis (7%). Two fatal adverse reactions of myocarditis occurred.
In KEYNOTE-048, KEYTRUDA monotherapy was discontinued due to adverse events in 12% of 300 patients with HNSCC; the most common adverse reactions leading to permanent discontinuation were sepsis (1.7%) and pneumonia (1.3%). The most common adverse reactions (≥20%) were fatigue (33%), constipation (20%), and rash (20%).
In KEYNOTE-048, when KEYTRUDA was administered in combination with platinum (cisplatin or carboplatin) and FU chemotherapy, KEYTRUDA was discontinued due to adverse reactions in 16% of 276 patients with HNSCC. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA were pneumonia (2.5%), pneumonitis (1.8%), and septic shock (1.4%). The most common adverse reactions (≥20%) were nausea (51%), fatigue (49%), constipation (37%), vomiting (32%), mucosal inflammation (31%), diarrhea (29%), decreased appetite (29%), stomatitis (26%), and cough (22%).
In KEYNOTE-012, KEYTRUDA was discontinued due to adverse reactions in 17% of 192 patients with HNSCC. Serious adverse reactions occurred in 45% of patients. The most frequent serious adverse reactions reported in at least 2% of patients were pneumonia, dyspnea, confusional state, vomiting, pleural effusion, and respiratory failure. The most common adverse reactions (≥20%) were fatigue, decreased appetite, and dyspnea. Adverse reactions occurring in patients with HNSCC were generally similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy, with the exception of increased incidences of facial edema and new or worsening hypothyroidism.
In KEYNOTE-204, KEYTRUDA was discontinued due to adverse reactions in 14% of 148 patients with cHL. Serious adverse reactions occurred in 30% of patients receiving KEYTRUDA; those ≥1% were pneumonitis, pneumonia, pyrexia, myocarditis, acute kidney injury, febrile neutropenia, and sepsis. Three patients died from causes other than disease progression: 2 from complications after allogeneic HSCT and 1 from unknown cause. The most common adverse reactions (≥20%) were upper respiratory tract infection (41%), musculoskeletal pain (32%), diarrhea (22%), and pyrexia, fatigue, rash, and cough (20% each).
In KEYNOTE-087, KEYTRUDA was discontinued due to adverse reactions in 5% of 210 patients with cHL. Serious adverse reactions occurred in 16% of patients; those ≥1% were pneumonia, pneumonitis, pyrexia, dyspnea, GVHD, and herpes zoster. Two patients died from causes other than disease progression: 1 from GVHD after subsequent allogeneic HSCT and 1 from septic shock. The most common adverse reactions (≥20%) were fatigue (26%), pyrexia (24%), cough (24%), musculoskeletal pain (21%), diarrhea (20%), and rash (20%).
In KEYNOTE-170, KEYTRUDA was discontinued due to adverse reactions in 8% of 53 patients with PMBCL. Serious adverse reactions occurred in 26% of patients and included arrhythmia (4%), cardiac tamponade (2%), myocardial infarction (2%), pericardial effusion (2%), and pericarditis (2%). Six (11%) patients died within 30 days of start of treatment. The most common adverse reactions (≥20%) were musculoskeletal pain (30%), upper respiratory tract infection and pyrexia (28% each), cough (26%), fatigue (23%), and dyspnea (21%).
In KEYNOTE-A39, when KEYTRUDA was administered in combination with enfortumab vedotin to patients with locally advanced or metastatic urothelial cancer (n=440), fatal adverse reactions occurred in 3.9% of patients, including acute respiratory failure (0.7%), pneumonia (0.5%), and pneumonitis/ILD (0.2%). Serious adverse reactions occurred in 50% of patients receiving KEYTRUDA in combination with enfortumab vedotin; the serious adverse reactions in ≥2% of patients were rash (6%), acute kidney injury (5%), pneumonitis/ILD (4.5%), urinary tract infection (3.6%), diarrhea (3.2%), pneumonia (2.3%), pyrexia (2%), and hyperglycemia (2%). Permanent discontinuation of KEYTRUDA occurred in 27% of patients. The most common adverse reactions (≥2%) resulting in permanent discontinuation of KEYTRUDA were pneumonitis/ILD (4.8%) and rash (3.4%). The most common adverse reactions (≥20%) occurring in patients treated with KEYTRUDA in combination with enfortumab vedotin were rash (68%), peripheral neuropathy (67%), fatigue (51%), pruritus (41%), diarrhea (38%), alopecia (35%), weight loss (33%), decreased appetite (33%), nausea (26%), constipation (26%), dry eye (24%), dysgeusia (21%), and urinary tract infection (21%).
In KEYNOTE-052, KEYTRUDA was discontinued due to adverse reactions in 11% of 370 patients with locally advanced or metastatic urothelial carcinoma. Serious adverse reactions occurred in 42% of patients; those ≥2% were urinary tract infection, hematuria, acute kidney injury, pneumonia, and urosepsis. The most common adverse reactions (≥20%) were fatigue (38%), musculoskeletal pain (24%), decreased appetite (22%), constipation (21%), rash (21%), and diarrhea (20%).
In KEYNOTE-045, KEYTRUDA was discontinued due to adverse reactions in 8% of 266 patients with locally advanced or metastatic urothelial carcinoma. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was pneumonitis (1.9%). Serious adverse reactions occurred in 39% of KEYTRUDA-treated patients; those ≥2% were urinary tract infection, pneumonia, anemia, and pneumonitis. The most common adverse reactions (≥20%) in patients who received KEYTRUDA were fatigue (38%), musculoskeletal pain (32%), pruritus (23%), decreased appetite (21%), nausea (21%), and rash (20%).
In KEYNOTE-057, KEYTRUDA was discontinued due to adverse reactions in 11% of 148 patients with high-risk NMIBC. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was pneumonitis (1.4%). Serious adverse reactions occurred in 28% of patients; those ≥2% were pneumonia (3%), cardiac ischemia (2%), colitis (2%), pulmonary embolism (2%), sepsis (2%), and urinary tract infection (2%). The most common adverse reactions (≥20%) were fatigue (29%), diarrhea (24%), and rash (24%).
Adverse reactions occurring in patients with MSI-H or dMMR CRC were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-158 and KEYNOTE-164, adverse reactions occurring in patients with MSI-H or dMMR cancer were similar to those occurring in patients with other solid tumors who received KEYTRUDA as a single agent.
In KEYNOTE-811, when KEYTRUDA was administered in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy, KEYTRUDA was discontinued due to adverse reactions in 6% of 217 patients with locally advanced unresectable or metastatic HER2+ gastric or GEJ adenocarcinoma. The most common adverse reaction resulting in permanent discontinuation was pneumonitis (1.4%). In the KEYTRUDA arm vs placebo, there was a difference of ≥5% incidence between patients treated with KEYTRUDA vs standard of care for diarrhea (53% vs 44%) and nausea (49% vs 44%).
In KEYNOTE-859, when KEYTRUDA was administered in combination with fluoropyrimidine- and platinum-containing chemotherapy, serious adverse reactions occurred in 45% of 785 patients. Serious adverse reactions in >2% of patients included pneumonia (4.1%), diarrhea (3.9%), hemorrhage (3.9%), and vomiting (2.4%). Fatal adverse reactions occurred in 8% of patients who received KEYTRUDA, including infection (2.3%) and thromboembolism (1.3%). KEYTRUDA was permanently discontinued due to adverse reactions in 15% of patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA (≥1%) were infections (1.8%) and diarrhea (1.0%). The most common adverse reactions (reported in ≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were peripheral neuropathy (47%), nausea (46%), fatigue (40%), diarrhea (36%), vomiting (34%), decreased appetite (29%), abdominal pain (26%), palmar-plantar erythrodysesthesia syndrome (25%), constipation (22%), and weight loss (20%).
In KEYNOTE-590, when KEYTRUDA was administered with cisplatin and fluorouracil to patients with metastatic or locally advanced esophageal or GEJ (tumors with epicenter 1 to 5 centimeters above the GEJ) carcinoma who were not candidates for surgical resection or definitive chemoradiation, KEYTRUDA was discontinued due to adverse reactions in 15% of 370 patients. The most common adverse reactions resulting in permanent discontinuation of KEYTRUDA (≥1%) were pneumonitis (1.6%), acute kidney injury (1.1%), and pneumonia (1.1%). The most common adverse reactions (≥20%) with KEYTRUDA in combination with chemotherapy were nausea (67%), fatigue (57%), decreased appetite (44%), constipation (40%), diarrhea (36%), vomiting (34%), stomatitis (27%), and weight loss (24%).
Adverse reactions occurring in patients with esophageal cancer who received KEYTRUDA as a monotherapy were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-A18, when KEYTRUDA was administered with CRT (cisplatin plus external beam radiation therapy [EBRT] followed by brachytherapy [BT]) to patients with FIGO 2014 Stage III-IVA cervical cancer, fatal adverse reactions occurred in 1.4% of 292 patients, including 1 case each (0.3%) of large intestinal perforation, urosepsis, sepsis, and vaginal hemorrhage. Serious adverse reactions occurred in 30% of patients; those ≥1% included urinary tract infection (2.7%), urosepsis (1.4%), and sepsis (1%). KEYTRUDA was discontinued for adverse reactions in 7% of patients. The most common adverse reaction (≥1%) resulting in permanent discontinuation was diarrhea (1%). For patients treated with KEYTRUDA in combination with CRT, the most common adverse reactions (≥10%) were nausea (56%), diarrhea (50%), vomiting (33%), urinary tract infection (32%), fatigue (26%), hypothyroidism (20%), constipation (18%), decreased appetite and weight loss (17% each), abdominal pain and pyrexia (12% each), hyperthyroidism, dysuria, rash (11% each), and pelvic pain (10%).
In KEYNOTE-826, when KEYTRUDA was administered in combination with paclitaxel and cisplatin or paclitaxel and carboplatin, with or without bevacizumab (n=307), to patients with persistent, recurrent, or first-line metastatic cervical cancer regardless of tumor PD-L1 expression who had not been treated with chemotherapy except when used concurrently as a radio-sensitizing agent, fatal adverse reactions occurred in 4.6% of patients, including 3 cases of hemorrhage, 2 cases each of sepsis and due to unknown causes, and 1 case each of acute myocardial infarction, autoimmune encephalitis, cardiac arrest, cerebrovascular accident, femur fracture with perioperative pulmonary embolus, intestinal perforation, and pelvic infection. Serious adverse reactions occurred in 50% of patients receiving KEYTRUDA in combination with chemotherapy with or without bevacizumab; those ≥3% were febrile neutropenia (6.8%), urinary tract infection (5.2%), anemia (4.6%), and acute kidney injury and sepsis (3.3% each).
KEYTRUDA was discontinued in 15% of patients due to adverse reactions. The most common adverse reaction resulting in permanent discontinuation (≥1%) was colitis (1%).
For patients treated with KEYTRUDA, chemotherapy, and bevacizumab (n=196), the most common adverse reactions (≥20%) were peripheral neuropathy (62%), alopecia (58%), anemia (55%), fatigue/asthenia (53%), nausea and neutropenia (41% each), diarrhea (39%), hypertension and thrombocytopenia (35% each), constipation and arthralgia (31% each), vomiting (30%), urinary tract infection (27%), rash (26%), leukopenia (24%), hypothyroidism (22%), and decreased appetite (21%).
For patients treated with KEYTRUDA in combination with chemotherapy with or without bevacizumab, the most common adverse reactions (≥20%) were peripheral neuropathy (58%), alopecia (56%), fatigue (47%), nausea (40%), diarrhea (36%), constipation (28%), arthralgia (27%), vomiting (26%), hypertension and urinary tract infection (24% each), and rash (22%).
In KEYNOTE-158, KEYTRUDA was discontinued due to adverse reactions in 8% of 98 patients with previously treated recurrent or metastatic cervical cancer. Serious adverse reactions occurred in 39% of patients receiving KEYTRUDA; the most frequent included anemia (7%), fistula, hemorrhage, and infections [except urinary tract infections] (4.1% each). The most common adverse reactions (≥20%) were fatigue (43%), musculoskeletal pain (27%), diarrhea (23%), pain and abdominal pain (22% each), and decreased appetite (21%).
In KEYNOTE-394, KEYTRUDA was discontinued due to adverse reactions in 13% of 299 patients with previously treated hepatocellular carcinoma. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA was ascites (2.3%). The most common adverse reactions in patients receiving KEYTRUDA (≥10%) were pyrexia (18%), rash (18%), diarrhea (16%), decreased appetite (15%), pruritus (12%), upper respiratory tract infection (11%), cough (11%), and hypothyroidism (10%).
In KEYNOTE-966, when KEYTRUDA was administered in combination with gemcitabine and cisplatin, KEYTRUDA was discontinued for adverse reactions in 15% of 529 patients with locally advanced unresectable or metastatic biliary tract cancer. The most common adverse reaction resulting in permanent discontinuation of KEYTRUDA (≥1%) was pneumonitis (1.3%). Adverse reactions leading to the interruption of KEYTRUDA occurred in 55% of patients. The most common adverse reactions or laboratory abnormalities leading to interruption of KEYTRUDA (≥2%) were decreased neutrophil count (18%), decreased platelet count (10%), anemia (6%), decreased white blood cell count (4%), pyrexia (3.8%), fatigue (3.0%), cholangitis (2.8%), increased ALT (2.6%), increased AST (2.5%), and biliary obstruction (2.3%).
In KEYNOTE-017 and KEYNOTE-913, adverse reactions occurring in patients with MCC (n=105) were generally similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a single agent.
In KEYNOTE-426, when KEYTRUDA was administered in combination with axitinib, fatal adverse reactions occurred in 3.3% of 429 patients. Serious adverse reactions occurred in 40% of patients, the most frequent (≥1%) were hepatotoxicity (7%), diarrhea (4.2%), acute kidney injury (2.3%), dehydration (1%), and pneumonitis (1%). Permanent discontinuation due to an adverse reaction occurred in 31% of patients; KEYTRUDA only (13%), axitinib only (13%), and the combination (8%); the most common were hepatotoxicity (13%), diarrhea/colitis (1.9%), acute kidney injury (1.6%), and cerebrovascular accident (1.2%). The most common adverse reactions (≥20%) were diarrhea (56%), fatigue/asthenia (52%), hypertension (48%), hepatotoxicity (39%), hypothyroidism (35%), decreased appetite (30%), palmar-plantar erythrodysesthesia (28%), nausea (28%), stomatitis/mucosal inflammation (27%), dysphonia (25%), rash (25%), cough (21%), and constipation (21%).
In KEYNOTE-564, when KEYTRUDA was administered as a single agent for the adjuvant treatment of renal cell carcinoma, serious adverse reactions occurred in 20% of patients receiving KEYTRUDA; the serious adverse reactions (≥1%) were acute kidney injury, adrenal insufficiency, pneumonia, colitis, and diabetic ketoacidosis (1% each). Fatal adverse reactions occurred in 0.2% including 1 case of pneumonia. Discontinuation of KEYTRUDA due to adverse reactions occurred in 21% of 488 patients; the most common (≥1%) were increased ALT (1.6%), colitis (1%), and adrenal insufficiency (1%). The most common adverse reactions (≥20%) were musculoskeletal pain (41%), fatigue (40%), rash (30%), diarrhea (27%), pruritus (23%), and hypothyroidism (21%).
In KEYNOTE-868, when KEYTRUDA was administered in combination with chemotherapy (paclitaxel and carboplatin) to patients with advanced or recurrent endometrial carcinoma (n=382), serious adverse reactions occurred in 35% of patients receiving KEYTRUDA in combination with chemotherapy, compared to 19% of patients receiving placebo in combination with chemotherapy (n=377). Fatal adverse reactions occurred in 1.6% of patients receiving KEYTRUDA in combination with chemotherapy, including COVID-19 (0.5%) and cardiac arrest (0.3%). KEYTRUDA was discontinued for an adverse reaction in 14% of patients. Adverse reactions occurring in patients treated with KEYTRUDA and chemotherapy were generally similar to those observed with KEYTRUDA alone or chemotherapy alone, with the exception of rash (33% all Grades; 2.9% Grades 3-4).
Adverse reactions occurring in patients with MSI-H or dMMR endometrial carcinoma who received KEYTRUDA as a single agent were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a single agent.
Adverse reactions occurring in patients with TMB-H cancer were similar to those occurring in patients with other solid tumors who received KEYTRUDA as a single agent.
Adverse reactions occurring in patients with recurrent or metastatic cSCC or locally advanced cSCC were similar to those occurring in patients with melanoma or NSCLC who received KEYTRUDA as a monotherapy.
In KEYNOTE-522, when KEYTRUDA was administered with neoadjuvant chemotherapy (carboplatin and paclitaxel followed by doxorubicin or epirubicin and cyclophosphamide) followed by surgery and continued adjuvant treatment with KEYTRUDA as a single agent (n=778) to patients with newly diagnosed, previously untreated, high-risk early-stage TNBC, fatal adverse reactions occurred in 0.9% of patients, including 1 each of adrenal crisis, autoimmune encephalitis, hepatitis, pneumonia, pneumonitis, pulmonary embolism, and sepsis in association with multiple organ dysfunction syndrome and myocardial infarction. Serious adverse reactions occurred in 44% of patients receiving KEYTRUDA; those ≥2% were febrile neutropenia (15%), pyrexia (3.7%), anemia (2.6%), and neutropenia (2.2%). KEYTRUDA was discontinued in 20% of patients due to adverse reactions. The most common reactions (≥1%) resulting in permanent discontinuation were increased ALT (2.7%), increased AST (1.5%), and rash (1%). The most common adverse reactions (≥20%) in patients receiving KEYTRUDA were fatigue (70%), nausea (67%), alopecia (61%), rash (52%), constipation (42%), diarrhea and peripheral neuropathy (41% each), stomatitis (34%), vomiting (31%), headache (30%), arthralgia (29%), pyrexia (28%), cough (26%), abdominal pain (24%), decreased appetite (23%), insomnia (21%), and myalgia (20%).
In KEYNOTE-355, when KEYTRUDA and chemotherapy (paclitaxel, paclitaxel protein-bound, or gemcitabine and carboplatin) were administered to patients with locally recurrent unresectable or metastatic TNBC who had not been previously treated with chemotherapy in the metastatic setting (n=596), fatal adverse reactions occurred in 2.5% of patients, including cardio-respiratory arrest (0.7%) and septic shock (0.3%). Serious adverse reactions occurred in 30% of patients receiving KEYTRUDA in combination with chemotherapy; the serious reactions in ≥2% were pneumonia (2.9%), anemia (2.2%), and thrombocytopenia (2%). KEYTRUDA was discontinued in 11% of patients due to adverse reactions. The most common reactions resulting in permanent discontinuation (≥1%) were increased ALT (2.2%), increased AST (1.5%), and pneumonitis (1.2%). The most common adverse reactions (≥20%) in patients receiving KEYTRUDA in combination with chemotherapy were fatigue (48%), nausea (44%), alopecia (34%), diarrhea and constipation (28% each), vomiting and rash (26% each), cough (23%), decreased appetite (21%), and headache (20%).
Lactation
Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment and for 4 months after the last dose.
Pediatric Use
In KEYNOTE-051, 173 pediatric patients (65 pediatric patients aged 6 months to younger than 12 years and 108 pediatric patients aged 12 years to 17 years) were administered KEYTRUDA 2 mg/kg every 3 weeks. The median duration of exposure was 2.1 months (range: 1 day to 25 months).
Adverse reactions that occurred at a ≥10% higher rate in pediatric patients when compared to adults were pyrexia (33%), leukopenia (30%), vomiting (29%), neutropenia (28%), headache (25%), abdominal pain (23%), thrombocytopenia (22%), Grade 3 anemia (17%), decreased lymphocyte count (13%), and decreased white blood cell count (11%).
Geriatric Use
Of the 564 patients with locally advanced or metastatic urothelial cancer treated with KEYTRUDA in combination with enfortumab vedotin, 44% (n=247) were 65-74 years and 26% (n=144) were 75 years or older. No overall differences in safety or effectiveness were observed between patients 65 years of age or older and younger patients. Patients 75 years of age or older treated with KEYTRUDA in combination with enfortumab vedotin experienced a higher incidence of fatal adverse reactions than younger patients. The incidence of fatal adverse reactions was 4% in patients younger than 75 and 7% in patients 75 years or older.
Additional Selected KEYTRUDA Indications in the U.S.
Melanoma
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic melanoma.
KEYTRUDA is indicated for the adjuvant treatment of adult and pediatric (12 years and older) patients with Stage IIB, IIC, or III melanoma following complete resection.
Non-Small Cell Lung Cancer
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of patients with metastatic nonsquamous non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic tumor aberrations.
KEYTRUDA, in combination with carboplatin and either paclitaxel or paclitaxel protein-bound, is indicated for the first-line treatment of patients with metastatic squamous NSCLC.
KEYTRUDA, as a single agent, is indicated for the first-line treatment of patients with NSCLC expressing PD-L1 [Tumor Proportion Score (TPS) ≥1%] as determined by an FDA-approved test, with no EGFR or ALK genomic tumor aberrations, and is:
Stage III where patients are not candidates for surgical resection or definitive chemoradiation, or
metastatic.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with metastatic NSCLC whose tumors express PD-L1 (TPS ≥1%) as determined by an FDA-approved test, with disease progression on or after platinum-containing chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving KEYTRUDA.
KEYTRUDA is indicated for the treatment of patients with resectable (tumors ≥4 cm or node positive) NSCLC in combination with platinum-containing chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
KEYTRUDA, as a single agent, is indicated as adjuvant treatment following resection and platinum-based chemotherapy for adult patients with Stage IB (T2a ≥4 cm), II, or IIIA NSCLC.
Malignant Pleural Mesothelioma
KEYTRUDA, in combination with pemetrexed and platinum chemotherapy, is indicated for the first-line treatment of adult patients with unresectable advanced or metastatic malignant pleural mesothelioma (MPM).
Classical Hodgkin Lymphoma
KEYTRUDA is indicated for the treatment of adult patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
KEYTRUDA is indicated for the treatment of pediatric patients with refractory cHL, or cHL that has relapsed after 2 or more lines of therapy.
Primary Mediastinal Large B-Cell Lymphoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after 2 or more prior lines of therapy. KEYTRUDA is not recommended for treatment of patients with PMBCL who require urgent cytoreductive therapy.
Urothelial Cancer
KEYTRUDA, in combination with enfortumab vedotin, is indicated for the treatment of adult patients with locally advanced or metastatic urothelial cancer.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma:
who are not eligible for any platinum-containing chemotherapy, or
who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, non-muscle invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy.
Microsatellite Instability-High or Mismatch Repair Deficient Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
Microsatellite Instability-High or Mismatch Repair Deficient Colorectal Cancer
KEYTRUDA is indicated for the treatment of patients with unresectable or metastatic MSI-H or dMMR colorectal cancer (CRC) as determined by an FDA-approved test.
Gastric Cancer
KEYTRUDA, in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy, is indicated for the first-line treatment of adults with locally advanced unresectable or metastatic HER2-positive gastric or gastroesophageal junction (GEJ) adenocarcinoma whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval of this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
KEYTRUDA, in combination with fluoropyrimidine- and platinum-containing chemotherapy, is indicated for the first-line treatment of adults with locally advanced unresectable or metastatic HER2-negative gastric or gastroesophageal junction (GEJ) adenocarcinoma.
Esophageal Cancer
KEYTRUDA is indicated for the treatment of patients with locally advanced or metastatic esophageal or gastroesophageal junction (GEJ) (tumors with epicenter 1 to 5 centimeters above the GEJ) carcinoma that is not amenable to surgical resection or definitive chemoradiation either:
in combination with platinum- and fluoropyrimidine-based chemotherapy, or
as a single agent after one or more prior lines of systemic therapy for patients with tumors of squamous cell histology that express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Cervical Cancer
KEYTRUDA, in combination with chemoradiotherapy (CRT), is indicated for the treatment of patients with FIGO 2014 Stage III-IVA cervical cancer.
KEYTRUDA, in combination with chemotherapy, with or without bevacizumab, is indicated for the treatment of patients with persistent, recurrent, or metastatic cervical cancer whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
KEYTRUDA, as a single agent, is indicated for the treatment of patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test.
Hepatocellular Carcinoma
KEYTRUDA is indicated for the treatment of patients with hepatocellular carcinoma (HCC) secondary to hepatitis B who have received prior systemic therapy other than a PD-1/PD-L1-containing regimen.
Biliary Tract Cancer
KEYTRUDA, in combination with gemcitabine and cisplatin, is indicated for the treatment of patients with locally advanced unresectable or metastatic biliary tract cancer (BTC).
Merkel Cell Carcinoma
KEYTRUDA is indicated for the treatment of adult and pediatric patients with recurrent locally advanced or metastatic Merkel cell carcinoma (MCC).
Renal Cell Carcinoma
KEYTRUDA, in combination with axitinib, is indicated for the first-line treatment of adult patients with advanced renal cell carcinoma (RCC).
KEYTRUDA is indicated for the adjuvant treatment of patients with RCC at intermediate-high or high risk of recurrence following nephrectomy, or following nephrectomy and resection of metastatic lesions.
Endometrial Carcinoma
KEYTRUDA, in combination with carboplatin and paclitaxel, followed by KEYTRUDA as a single agent, is indicated for the treatment of adult patients with primary advanced or recurrent endometrial carcinoma.
KEYTRUDA, as a single agent, is indicated for the treatment of adult patients with advanced endometrial carcinoma that is MSI-H or dMMR, as determined by an FDA-approved test, who have disease progression following prior systemic therapy in any setting and are not candidates for curative surgery or radiation.
Tumor Mutational Burden-High Cancer
KEYTRUDA is indicated for the treatment of adult and pediatric patients with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. The safety and effectiveness of KEYTRUDA in pediatric patients with TMB-H central nervous system cancers have not been established.
Cutaneous Squamous Cell Carcinoma
KEYTRUDA is indicated for the treatment of patients with recurrent or metastatic cutaneous squamous cell carcinoma (cSCC) or locally advanced cSCC that is not curable by surgery or radiation.
Triple-Negative Breast Cancer
KEYTRUDA is indicated for the treatment of patients with high-risk early-stage triple-negative breast cancer (TNBC) in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
KEYTRUDA, in combination with chemotherapy, is indicated for the treatment of patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1 (CPS ≥10) as determined by an FDA-approved test.
Merck’s focus on cancer
Every day, we follow the science as we work to discover innovations that can help patients, no matter what stage of cancer they have. As a leading oncology company, we are pursuing research where scientific opportunity and medical need converge, underpinned by our diverse pipeline of more than 25 novel mechanisms. With one of the largest clinical development programs across more than 30 tumor types, we strive to advance breakthrough science that will shape the future of oncology. By addressing barriers to clinical trial participation, screening and treatment, we work with urgency to reduce disparities and help ensure patients have access to high-quality cancer care. Our unwavering commitment is what will bring us closer to our goal of bringing life to more patients with cancer. For more information, visit
https://www.merck.com/research/oncology
.
About Merck
At Merck, known as MSD outside of the United States and Canada, we are unified around our purpose: We use the power of leading-edge science to save and improve lives around the world. For more than 130 years, we have brought hope to humanity through the development of important medicines and vaccines. We aspire to be the premier research-intensive biopharmaceutical company in the world – and today, we are at the forefront of research to deliver innovative health solutions that advance the prevention and treatment of diseases in people and animals. We foster a diverse and inclusive global workforce and operate responsibly every day to enable a safe, sustainable and healthy future for all people and communities. For more information, visit
www.merck.com
and connect with us on
X (formerly Twitter)
,
Facebook
,
Instagram
,
YouTube
and
LinkedIn
.
Forward-Looking Statement of Merck & Co., Inc., Rahway, N.J., USA
This news release of Merck & Co., Inc., Rahway, N.J., USA (the “company”) includes “forward-looking statements” within the meaning of the safe harbor provisions of the U.S. Private Securities Litigation Reform Act of 1995. These statements are based upon the current beliefs and expectations of the company’s management and are subject to significant risks and uncertainties. There can be no guarantees with respect to pipeline candidates that the candidates will receive the necessary regulatory approvals or that they will prove to be commercially successful. If underlying assumptions prove inaccurate or risks or uncertainties materialize, actual results may differ materially from those set forth in the forward-looking statements.
Risks and uncertainties include but are not limited to, general industry conditions and competition; general economic factors, including interest rate and currency exchange rate fluctuations; the impact of pharmaceutical industry regulation and health care legislation in the United States and internationally; global trends toward health care cost containment; technological advances, new products and patents attained by competitors; challenges inherent in new product development, including obtaining regulatory approval; the company’s ability to accurately predict future market conditions; manufacturing difficulties or delays; financial instability of international economies and sovereign risk; dependence on the effectiveness of the company’s patents and other protections for innovative products; and the exposure to litigation, including patent litigation, and/or regulatory actions.
The company undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future events or otherwise. Additional factors that could cause results to differ materially from those described in the forward-looking statements can be found in the company’s Annual Report on Form 10-K for the year ended December 31, 2023 and the company’s other filings with the Securities and Exchange Commission (SEC) available at the SEC’s Internet site (
www.sec.gov
).
Media:
Julie Cunningham
(617) 519-6264
Julie Loesch
(609) 477-8351
Investor:
Peter Dannenbaum
(732) 594-1579
Steven Graziano
(732) 594-1583
Source: Merck & Co., Inc.
Phase 3Clinical ResultPriority ReviewDrug Approval
Analysis
Perform a panoramic analysis of this field.
login
or
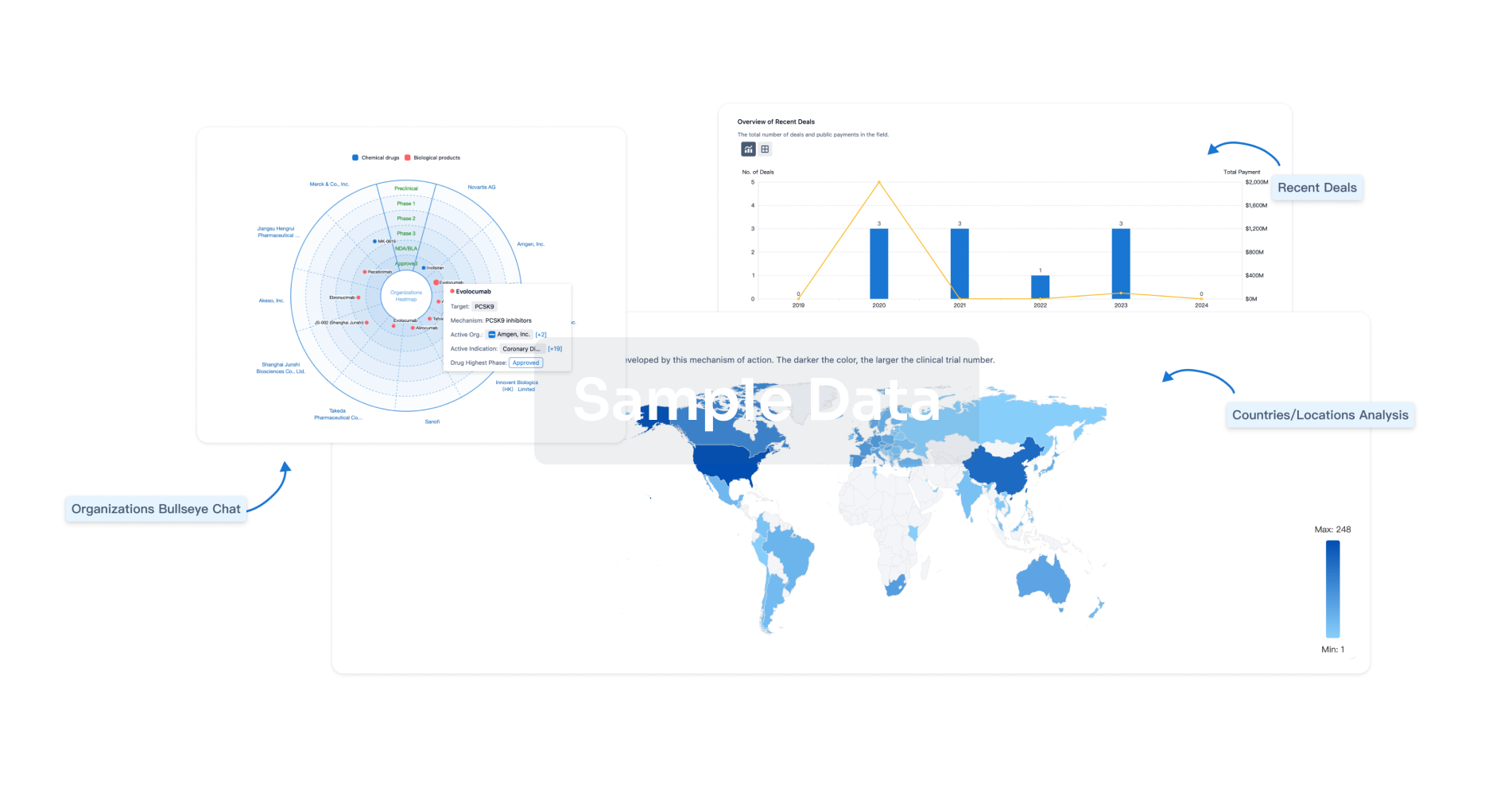
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free