Request Demo
Last update 17 Mar 2025
TNF x TNF-α x TNFR x TNFR1 x TRADD x TRAF2
Last update 17 Mar 2025
Related
100 Clinical Results associated with TNF x TNF-α x TNFR x TNFR1 x TRADD x TRAF2
Login to view more data
100 Translational Medicine associated with TNF x TNF-α x TNFR x TNFR1 x TRADD x TRAF2
Login to view more data
0 Patents (Medical) associated with TNF x TNF-α x TNFR x TNFR1 x TRADD x TRAF2
Login to view more data
7
Literatures (Medical) associated with TNF x TNF-α x TNFR x TNFR1 x TRADD x TRAF201 Jan 2016·Journal of orthopaedic research : official publication of the Orthopaedic Research Society
Does progranulin account for the opposite effects of etanercept and infliximab/adalimumab in osteoarthritis?
Letter
Author: Buza, John ; Liu, Chuan‐ju ; Wei, Jian‐lu
Dear Editors:
We read with great interest the recent article by Guilak et al1, which summarizes the significant advancements that have been made in our understanding of the development of post-traumatic arthritis (PTOA) after articular fracture (AF). We would like to congratulate the authors on their significant contributions to this field, including the development of a murine model of AF2, the assessment of histologic changes and quantitative synovial fluid biomarker concentrations involved in PTOA3,4, and the identification of pharmacologic agents that can lessen the severity of PTOA after AF5,6.
We were most interested in the authors recent study on the use of anti-cytokine therapy to prevent PTOA, in which the authors hypothesized that the intra-articular inhibition of IL-1, TNF-α, or both would prevent the development of PTOA after AF6. The authors demonstrated that sustained local inhibition of IL-1 by Interleukin-1 Receptor antagonist (IL-1RA, anakinra, Kineret®) reduced the severity of arthritic changes in both the cartilage and synovium after AF. Paradoxically, however, the authors found that the local inhibition of TNF-α using soluble tumor necrosis factor receptor II (sTNFRII, etanercept, Enbrel®) resulted in detrimental effects on bone morphology, cartilage degeneration, and synovial inflammation6.
There has been much interest in the role of TNF-α in the development of PTOA, as it is significantly up-regulated after fracture4,7 and is associated with chondrocyte destruction and death8. There exists two distinct receptors for TNF-α, TNFR1 and TNFR29,10. Although these receptors bind to TNF-α with almost equal affinity, they have been shown to mediate different intracellular pathways. TNFR1 recruits TRADD, TRAF-2, and FADD, and activates an inflammatory response11. While TNFR2 signaling is less well understood, several studies have shown that TNFR2 instead mediates an anti-inflammatory response12,13. Using mouse models of inflammatory arthritis, investigators have shown that TNFR2 has an immunoregulatory role in reducing inflammation and preventing bone destruction12,14. Studies from other fields have confirmed these findings, as TNF-α induced cardiomyopathy and heart failure is mediated largely through TNFR1, whereas TNFR2 has been shown to have cardioprotective effects15.
Studies from our laboratory also reveal the differential role of TNFR1 and TNFR2 in fracture healing and OA16-18. Our area of focus has been on a molecule termed progranulin (PGRN), a potent anti-inflammatory growth factor19-23. Interestingly, our global genetic screen for PGRN-associated proteins led to the discovery of TNFRs as PGRN-binding receptors16. PGRN and TNFα showed comparable binding affinity to TNFR1, in contrast, PGRN had an approximately 600-fold higher binding affinity for TFNR2 than TNFα16. Since PGRN and TNFα compete for binding to the same extracellular CRD2 and CRD3 domains of TNFR24, PGRN acts as a physiological antagonist of TNFα and disturbs the binding of TNFα and TNFRs16. More importantly, PGRN also acts as an optimal ligand of TNFR2 and directly activates the PGRN/TNFR2 protective and anti-inflammatory pathway. We have demonstrated that TNFR2 is critical for PGRN-mediated protection in OA development and bone fracture healing17,18,25. Another group recently showed that Atsttrin, an engineered protein composed of three TNFR-binding fragments of PGRN, ameliorated OA development in a surgically-induced mouse model26. In brief, PGRN and its derived Atsttrin appear to exert their anti-inflammatory and protective activities in OA by activation of the PGRN/TNFR2 protective/anabolic pathway12,14,27-29, and by inhibition of TNFα/TNFR1 inflammatory/catabolic signaling17,26.
Etanercept (Enbrel) is a fusion-soluble TNFR2 extracellular protein, and therefore inhibits both TNFα and PGRN. PGRN may be even more inhibited than TNFα, as PGRN has a much higher binding affinity to TNFR2 than TNFα16. In this way, Etanercept may be blocking PGRN’s protective and anti-inflammatory effect against the development of OA. This would explain the detrimental effects of Etanercept in OA observed by Olson et al1,6. Unlike Etanercept, mouse TNFα monoclonal antibody (Infliximab, Remicade) and humanized TNFα monoclonal antibody (Adalimumab, Humira) are specific for TNFα, and have been shown to be protective against the development of OA in animal models30-32. This is supported by clinical trials in which Infliximab and Adalimumab have been reported to alleviate symptoms of OA33-35. The opposing effects of TNFα-specific (i.e. Infliximab and Adalimumab) and non-specific (i.e. Etanercept) inhibitors in OA indicate the critical role of other ligand(s) of TNFR, such as PGRN, in the regulation of OA. TNFα is known to be the dominant inflammatory molecule in the pathogenesis of rheumatoid arthritis, and blocking TNFα with Etanercept is thus beneficial to the patients with rheumatoid arthritis. However, in the case of OA, the PGRN/TNFR2 protective/anabolic pathway is likely to outweigh the TNFα/TNFR1 inflammatory/catabolic pathway in regulating OA development. Therefore, blocking both PGRN and TNFα with Etanercept may lead to more severe OA.
In summary, the findings of Guilak et al on the negative effect of Etanercept in OA1,6, reports on the positive role of Infliximab and Adalimumab in OA30-32, and our data on PGRN-mediated protection in OA through TNFR signaling16,17, all suggest a complex interplay between TNFα, PGRN and their receptors in the pathogenesis of OA. Future studies are warranted to clarify these molecular mechanisms, which will not only better our understanding of TNFR signaling in the pathogenesis of OA, but may lead to innovative therapies for OA and other degenerative joint diseases via selectively targeting distinct TNFR pathways.
01 Sep 2011·The American journal of pathologyQ2 · MEDICINE
Characterization of DISC Formation and TNFR1 Translocation to Mitochondria in TNF-α–Treated Hepatocytes
Q2 · MEDICINE
Article
Author: Timothy R. Billiar ; Raghuveer Vallabhaneni ; Patricia A. Loughran ; Hyun Ae Eum ; Yinna Wang ; Donna Beer Stolz
Tumor necrosis factor receptor 1 (TNFR1) activation in hepatocytes can trigger apoptotic or inflammatory signaling. The factors that determine which signaling pathway dominates are not clear and are thought to relate to the efficiency of death-inducing signaling complex (DISC) formation. However, the steps involved in DISC formation in hepatocytes are poorly understood. In characterizing DISC formation within cultured hepatocytes, we demonstrated that TNF-α exposure leads to the rapid formation of a DISC involving TNF-α, the TNFR-associated death domain adaptor molecule (TRADD), the Fas-associated death domain adaptor molecule (FADD), caspase-8, TNFR-associated factor 2 (TRAF2), and receptor-interacting protein (RIP). The inclusion of the sensitizing agent actinomycin D both accelerated and amplified the appearance of the DISC. Notably, TNFR1 along with some DISC components also appeared within mitochondria within 30 minutes. Whereas TNFR1 consistently co-localized with the TRADD, FADD, the caspase-8, and TRAF2 in the cytosolic fraction, TNFR1 in the mitochondria was associated only with caspase-8 after TNF-α exposure. Similar observations were made in vivo using TNF-α with D-galactosamine. Actinomycin D alone also enhanced the appearance of DISC components in both cytosol and the mitochondria. Thus the DISC that includes TNFR1 forms in the cytosol of hepatocytes under both survival and pro-apoptotic conditions. The observations also suggest that TNF-α-mediated signaling includes the translocation of TNFR1 to mitochondria.
01 Sep 2005·ParasitologyQ3 · MEDICINE
Tumor necrosis factor receptor-mediated apoptosis inTrichinella spiralis-infected muscle cells
Q3 · MEDICINE
Article
Author: I. Nagano ; Y. Takahashi ; T. Boonmars ; Z. Wu
In order to reveal the mechanisms underlying nurse cell formation duringTrichinella spiralisinfection, the expression of the factors of tumor necrosis factor-alpha (TNF-α)/TNF receptor 1 (TNFR-1) signalling pathway mediating apoptosis was investigated. The analysed factors included TNF-α, TNFR-1, TNF receptor-associated death-domain (TRADD), caspase 3, caspase 8, TNF receptor associated factor-2 (TRAF2) and receptor interactive protein (RIP), all of which are involved in the TNF-α/TNFR-1 signalling pathway-mediated apoptosis. The quantitative RT-PCR indicated that the infected muscle tissues up-regulate the expression of pro-apoptosis genes (TNF-α, TNFR-1 and TRADD, caspase 3 and caspase 8), and anti-apoptosis genes (TRAF2 and RIP) at the beginning of cyst formation. The expression returned to the normal level after cyst formation. The quantitative RT-PCR analysis of mRNA from tissue samples isolated by laser capture micro-dissection confirmed that the up-regulation of these genes was restricted in infected muscle cells, was not in the inflammation cells around infected muscle cells nor in normal muscle cells. Thein situlocalization study of pro-apoptosis (TRADD, caspase 3) and anti-apoptosis gene products (TRAF2) indicated that these were expressed in the basophilic cytoplasm (infected muscle cell origin) of the nurse cells. Thus the present study suggests that the TNF-α/TNFR-1 signalling pathway is involved in nurse cell formation.
Analysis
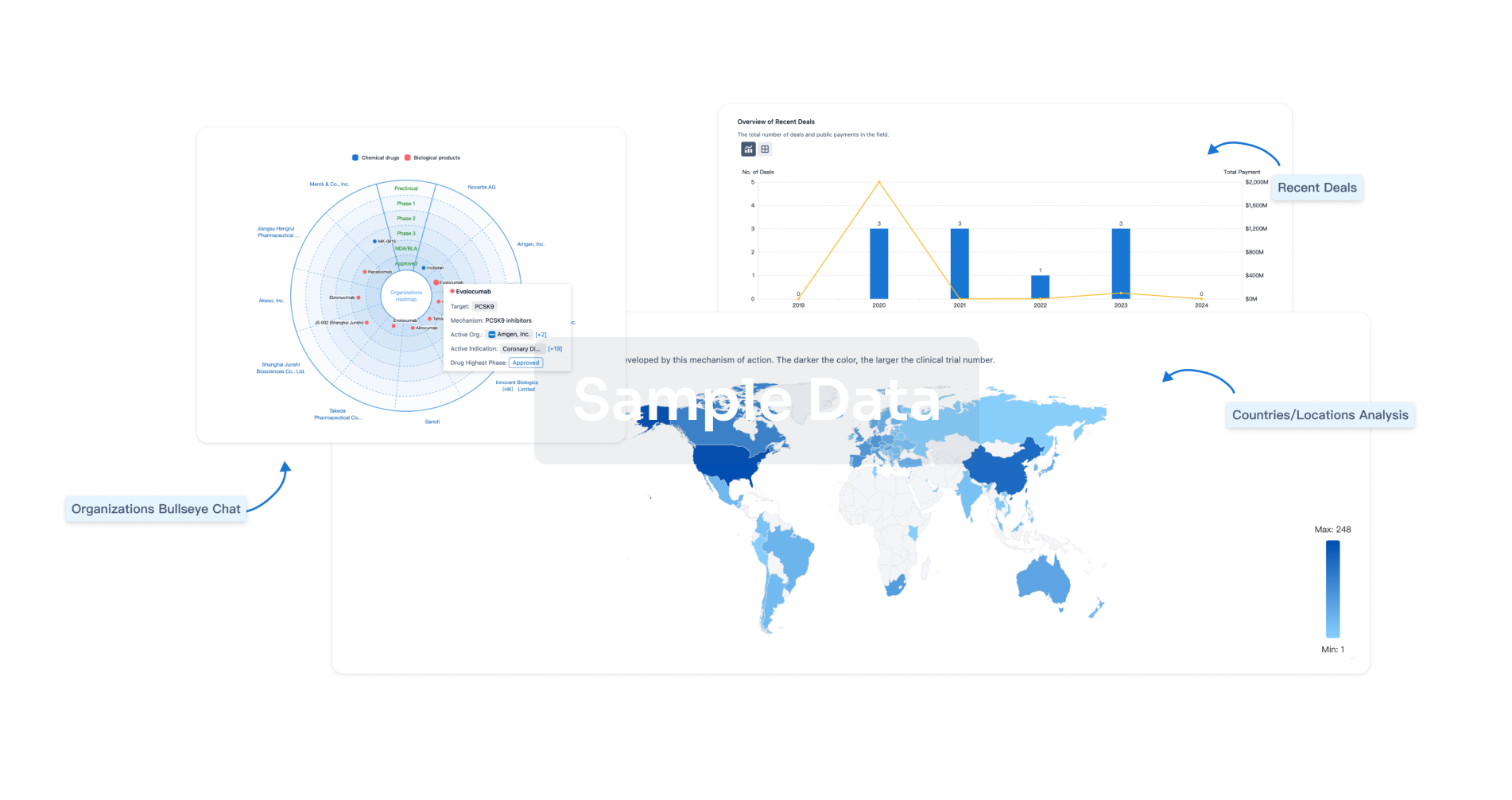
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free