Request Demo
Last update 08 May 2025
VHLL
Last update 08 May 2025
Basic Info
Synonyms VHL like, VHL-like protein, VHLL + [3] |
Introduction Functions as a dominant-negative VHL to serve as a protector of HIFalpha. |
Related
100 Clinical Results associated with VHLL
Login to view more data
100 Translational Medicine associated with VHLL
Login to view more data
0 Patents (Medical) associated with VHLL
Login to view more data
1,138
Literatures (Medical) associated with VHLL01 Jul 2025·European Journal of Medicinal Chemistry
Discovery of the first-in-class DOT1L PROTAC degrader
Article
Author: Xie, Ling ; Cao, Tao ; Xu, Zhongli ; Chen, Xian ; Sun, Renhong ; Kaniskan, H Ümit ; Kim, Minjeong ; Jin, Jian ; Kim, Huen Suk ; Yim, Hyerin
24 Apr 2025·Journal of Medicinal Chemistry
Discovery of a Potent and Selective Protein Arginine Methyltransferase 5 (PRMT5) PROTAC Degrader
Article
Author: Xie, Ling ; Qian, Chao ; Guccione, Ernesto ; Xiong, Yan ; Chen, Xian ; Shen, Yudao ; Jin, Jian ; Chen, Matthew ; Hu, Jacqueline ; Kim, Huensuk ; Zhong, Yue
01 Apr 2025·Zhonghua wai ke za zhi [Chinese journal of surgery]
[Diagnosis and treatment of pancreatic tumors in children:a retrospective study in a single center].
Article
Author: Li, M ; Liu, D H ; Li, Y ; Tang, X L
Analysis
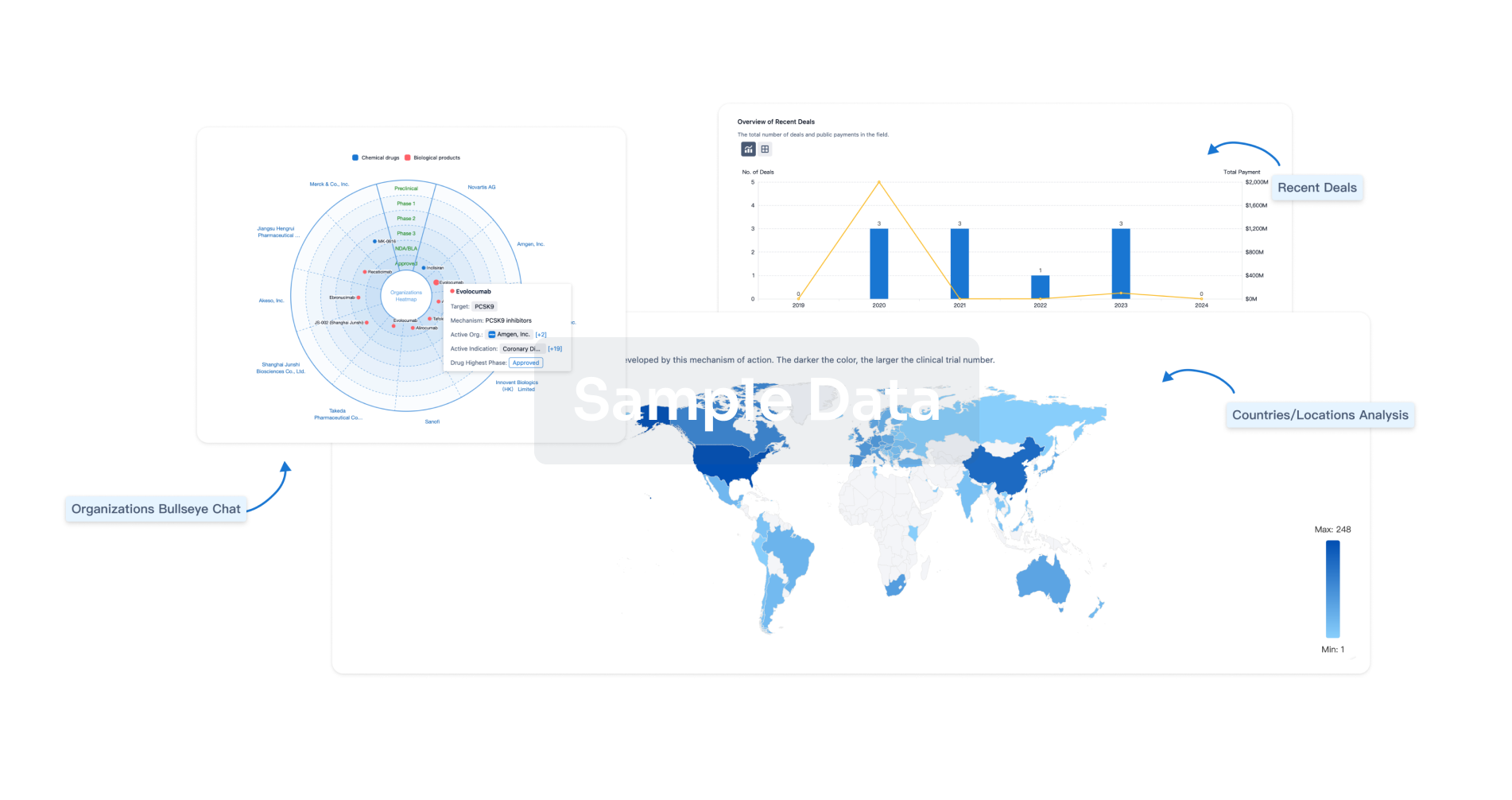
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free