Request Demo
Last update 08 May 2025
DOCK4
Last update 08 May 2025
Basic Info
Synonyms dedicator of cytokinesis 4, Dedicator of cytokinesis protein 4, DOCK4 + [2] |
Introduction Functions as a guanine nucleotide exchange factor (GEF) that promotes the exchange of GDP to GTP, converting inactive GDP-bound small GTPases into their active GTP-bound form (PubMed:12628187, PubMed:16464467). Involved in regulation of adherens junction between cells (PubMed:12628187). Plays a role in cell migration (PubMed:20679435).
Has a higher guanine nucleotide exchange factor activity compared to other isoforms. |
Analysis
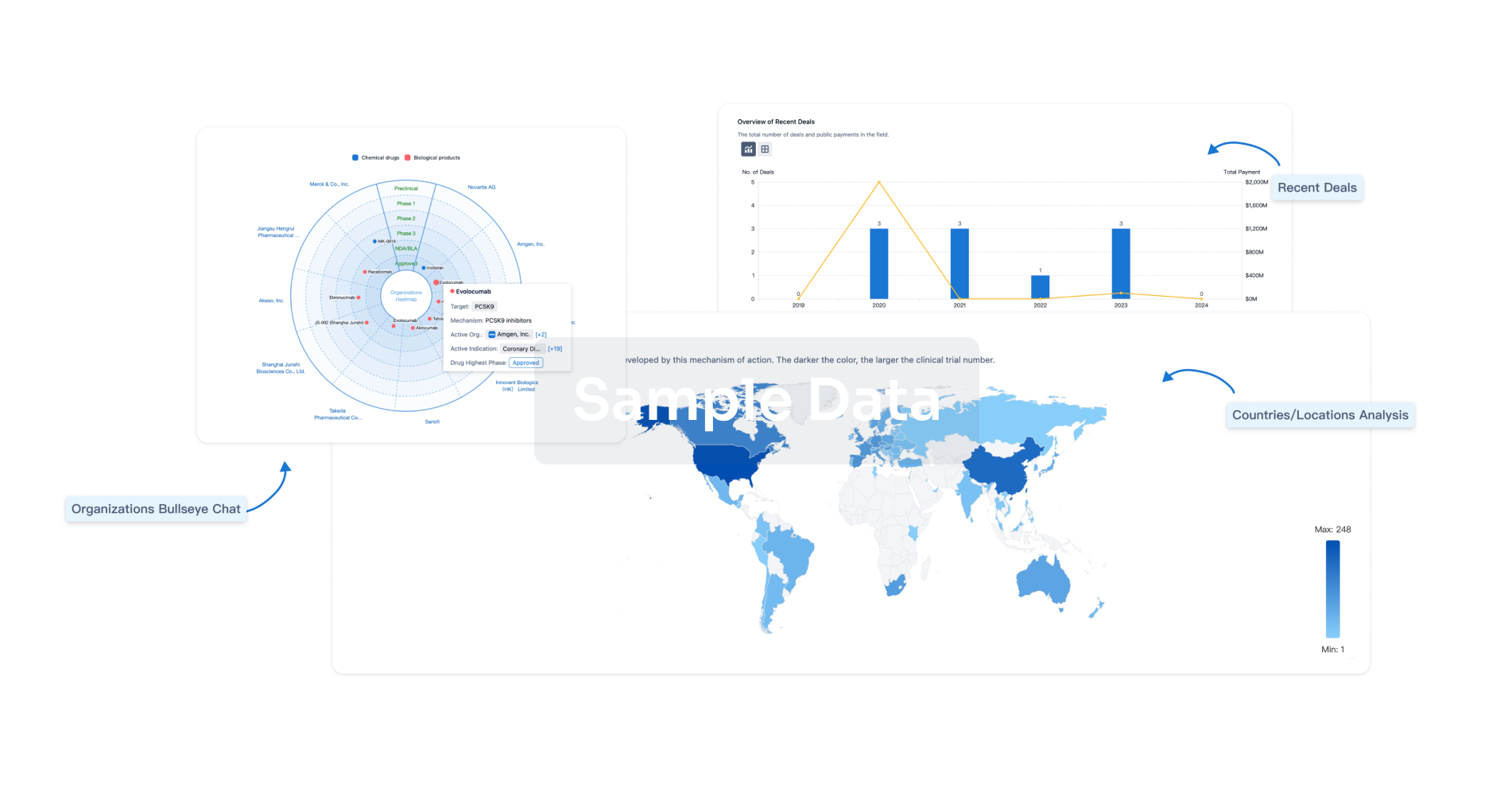
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free