Request Demo
Last update 06 May 2025
CD40 x MUC1
Last update 06 May 2025
Related
100 Clinical Results associated with CD40 x MUC1
Login to view more data
100 Translational Medicine associated with CD40 x MUC1
Login to view more data
0 Patents (Medical) associated with CD40 x MUC1
Login to view more data
17
Literatures (Medical) associated with CD40 x MUC116 Sep 2022·Oncogene
BTLA+CD200+ B cells dictate the divergent immune landscape and immunotherapeutic resistance in metastatic vs. primary pancreatic cancer
Article
Author: Aykut, Berk ; Diskin, Brian ; Weitzner, Yael ; Glinski, John ; Buttar, Chandan ; Farooq, Mohammad Saad ; Adam, Salma ; Wang, Wei ; Chen, Ruonan ; Leinwand, Joshua ; Miller, George ; Fnu, Amreek ; Soto, Gustavo Sanchez ; Asghar, Usman ; Werba, Gregor ; Panjwani, Angilee ; Shadaloey, Sorin A A ; Li, Eric ; Cohen, Deirdre ; Yang, Fan ; Sundberg, Belen ; Liria, Miguel ; Kim, Mirhee ; Salas, Ruben D ; Cassini, Marcelo F ; Hirsch, Carolina
Response to cancer immunotherapy in primary versus metastatic disease has not been well-studied. We found primary pancreatic ductal adenocarcinoma (PDA) is responsive to diverse immunotherapies whereas liver metastases are resistant. We discovered divergent immune landscapes in each compartment. Compared to primary tumor, liver metastases in both mice and humans are infiltrated by highly anergic T cells and MHCIIloIL10+ macrophages that are unable to present tumor-antigen. Moreover, a distinctive population of CD24+CD44-CD40- B cells dominate liver metastases. These B cells are recruited to the metastatic milieu by Muc1hiIL18hi tumor cells, which are enriched >10-fold in liver metastases. Recruited B cells drive macrophage-mediated adaptive immune-tolerance via CD200 and BTLA. Depleting B cells or targeting CD200/BTLA enhanced macrophage and T-cell immunogenicity and enabled immunotherapeutic efficacy of liver metastases. Our data detail the mechanistic underpinnings for compartment-specific immunotherapy-responsiveness and suggest that primary PDA models are poor surrogates for evaluating immunity in advanced disease.
17 Sep 2014·CELL CYCLE
Understanding Crohn's disease through genetics
Communications
Author: van Lookeren Campagne, Menno ; Murthy, Aditya
Crohn's disease (CD) is a chronic inflammatory bowel disease (IBD) with an eitologically complex pathology. Current evidence implicates dysregulation of the immune response to intestinal microflora and a parallel defect in maintenance of the epithelial barrier.1 The host genetic makeup is a key variable that underlies risk of disease, as highlighted by genome-wide association studies (GWAS). This, along with positive evidence for an impact of industrialization on IBD incidence strongly suggests that, in addition to genetic factors, host – environment interactions need to be tightly controlled to prevent mucosal inflammation.2
GWAS have highlighted disease-associated susceptibility loci associated with regulators of innate immunity (NOD2/CARD15, RIPK2, TLR4, CARD9, ICOSLG, CD40, LGALS9), adaptive immunity (IL23R, IL18RAP, RORC, IL10, PTPN22, IFNAR1, STAT3), epithelial barrier function/stress response (MUC1, XBP1, IBD5), and autophagy (ATG16L1, LRRK2, IRGM).1 Autophagy is a highly conserved and fundamental cytosolic recycling pathway that has the potential to impact the numerous cellular processes including cellular metabolism, turnover of cytosolic cargo (i.e. damaged organelles, cytotoxic aggregates), growth factor/cytokine secretion and intracellular pathogen clearance that are perturbed in Crohn's disease.2
A missense variant in the autophagy gene ATG16L1 (rs2241880) has been consistently associated with increase incidence of Crohn's disease. This variant results in an amino acid change of Thr-300-Ala (T300A) in exon 9 of human ATG16L1.3 By performing multiple sequence alignments of ATG16L1 exon 9 across species, the presence of a highly conserved putative caspase cleavage substrate spanning amino acids 296-299 (296-DNVD-299) was observed.4 Previous work has demonstrated that Glycine, Serine, or Alanine are preferred at the P1’ site of a caspase cleavage substrate.5 We hypothesized that the T300A variant would therefore be more sensitive to Caspase-mediated cleavage at D299. This was demonstrated first by cell-free assays of in vitro translated human ATG16L1β harboring the non-risk (T300), risk (A300) and non-cleavable (D299E) variants in exon 9. Next, using primary macrophages from healthy donors and a murine knock-in model of the T300A variant, Caspase 3 activation by death receptor stimulation was shown to result in enhanced ATG16L1 processing in the presence of the Crohn's disease risk variants. Knock down of individual effector caspases revealed Caspase 3 as the relevant protease needed for ATG16L1 processing, and this was confirmed in primary macrophages cultured from Caspase 3 knockout mice. Thus, the presence of a Crohn's disease risk variant and caspase-activating conditions results in enhanced degradation of ATG16L1, as also demonstrated by Lassen et al. (Fig. 1).6 Compatible with the importance of this pathway in disease, loss-of-function mutations in X-linked Inhibitor of Apoptosis (XIAP), a negative regulator of Caspase 3 activation and NOD1/2 signaling, have been associated inflammatory bowel disease.7
Figure 1.
Interaction between IBD-associated genes coordinates gut inflammation. The T300A variant sensitizes ATG16L1 to processing by Caspase 3, which is inhibited by XIAP. Autophagy regulates processes such as pathogen sensing and ER-stress responses arising ...
While autophagy is constitutively active as a cellular recycling program, it is strongly upregulated upon cellular stress conditions such as nutrient starvation or infection with intracellular pathogens. Consistently, defective autophagosome biogenesis in murine and human cells expressing the T300A variant of ATG16L1 was correlated with induction of Caspase 3 activation upon starvation.4 Defective autophagosome biogenesis further impacts bacterial clearance by xenophagy, an evolutionarily conserved, cell autonomous anti-bacterial defense program. Host-microbe interactions in the intestinal microenviroment in turn strongly influence the onset and progression of IBD by controlling inflammation and dysbiosis, a state where pathogenic microbial strains bloom; these are usually suppressed under healthy conditions.2 Defective clearance of intracellular bacteria, dysbiosis and inflammation act in concert to precipitate IBD. Genetics further contributes to disruption of intestinal homeostasis as the T300A variant of ATG16L1 impairs clearance of the enteric pathogen Yersinia enterocolitica in the ileum, a region of the small intestine commonly affected in Crohn's disease. In T316A knock-in mice, reduced clearance of Y.enterocolitica was evidenced by increased colonization in mesenteric lymph nodes following oral administration of the pathogen. Thus the Crohn's disease-associated variant in ATG16L1 results in defective autophagy following nutrient starvation or infection with an ileal pathogen, further emphasizing the importance of this pathway in disease.4,6
The successes of adalimumab and etanercept, inhibitors of tumor necrosis factor α, in treating IBD, highlights a central role of this inflammatory cytokine in Crohn's disease.2 Further upstream, understanding how autophagy proteins are implicated in sensing pathogens and regulating inflammatory responses is critical for understanding the impact of the genetic variants on disease. Using live and heat-killed Y.enterocolitica, we made 2 distinct observations: First, T300A knock-in macrophages produced elevated levels of IL-1β, TNF and IL-6 upon infection with live bacteria. Second, TNF levels correlated with intracellular bacterial survival, as no elevation in TNF was observed when T300A knock-in macrophages were infected with heat-killed bacteria. On the other hand, IL-6 and IL-1β levels were elevated even under comparable loads of killed bacteria.5 These observations raise the intriguing possibility that innate inflammatory signaling downstream of specific pathogen stimuli may also be regulated by ATG16L1 genotype.
Recent studies have proposed functional cooperation between IBD associated genes (Fig. 1). Interactions between NOD2 and ATG16L1 seem to regulate cytokine production following recognition of bacterial peptidoglycan, whereas autophagy mitigates chronic ER-stress induced by loss of XBP1 in intestinal epithelial cells.2 These studies reveal the molecular pathways that are regulated at multiple nodes by IBD associated genes and provide critical clues for new therapeutic targets and accompanying diagnostics.
01 Jan 2010·Journal of innate immunityQ2 · MEDICINE
Deletion of the Mucin-Like Molecule Muc1 Enhances Dendritic Cell Activation in Response to Toll-Like Receptor Ligands
Q2 · MEDICINE
ArticleOA
Author: Lu, Wenju ; Guo, Jia ; Bauer, Stephen ; Walter, Scott ; Lillehoj, Erik P. ; Williams, Marc A. ; Georas, Steve N. ; Bushnell, Timothy P.
Dendritic cells (DC) are potent professional antigen-presenting cells that drive primary immune responses to infections or other agonists perceived as ‘dangerous’. Muc1 is the only cell surface mucin or MUC gene product that is expressed in DC. Unlike other members of this glycoprotein family, Muc1 possesses a unique cytosolic region capable of signal transduction and attenuating toll-like receptor (TLR) activation. The expression and function of Muc1 has been intensively investigated on epithelial and tumor cells, but relatively little is known about its function on DC. We hypothesized that Muc1 would influence in vitro generation and primary DC activation in response to the TLR4 and TLR5 ligands lipopolysaccharide and flagellin. Compared with Muc1+/+ DC, we found that Muc1–/– DC were constitutively activated, as determined by higher expression of co-stimulatory molecules (CD40, CD80 and CD86), greater secretion of immunoregulatory cytokines (TNF-α and VEGF), and better stimulation of allogeneic naïve CD4+ T cell proliferation. After activation by either LPS or flagellin and co-culture with allogeneic CD4+ T cells, Muc1–/– DC also induced greater secretion of TNF-α and IFN-γ compared to similarly activated Muc1+/+ DC. Taken together, our results indicate that deletion of Muc1 promotes a heightened functional response of DC in response to TLR4 and TLR5 signaling pathways, and suggests a previously under-appreciated role for Muc1 in regulating innate immune responses of DC.
Analysis
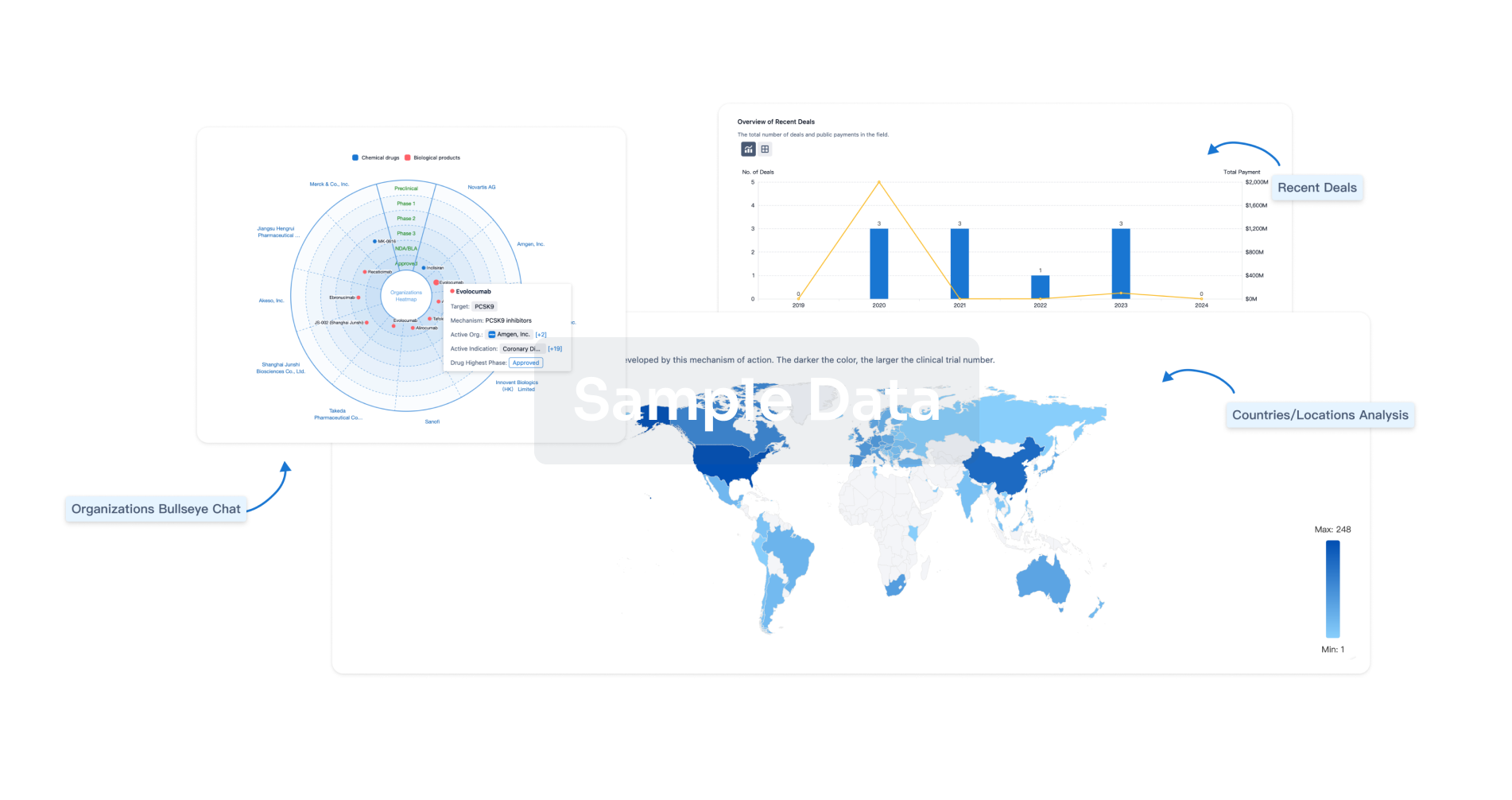
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free