Request Demo
Last update 08 May 2025
PAPD7
Last update 08 May 2025
Basic Info
Synonyms DNA polymerase sigma, LAK-1, Non-canonical poly(A) RNA polymerase PAPD7 + [14] |
Introduction Terminal nucleotidyltransferase that catalyzes preferentially the transfer of ATP and GTP on RNA 3' poly(A) tail creating a heterogeneous 3' poly(A) tail leading to mRNAs stabilization by protecting mRNAs from active deadenylation (PubMed:23376078, PubMed:30026317). Also functions as a catalytic subunit of a TRAMP-like complex which has a poly(A) RNA polymerase activity and is involved in a post-transcriptional quality control mechanism. Polyadenylation with short oligo(A) tails is required for the degradative activity of the exosome on several of its nuclear RNA substrates. Has no terminal uridylyltransferase activity, and does not play a role in replication-dependent histone mRNA degradation via uridylation (PubMed:23376078). |
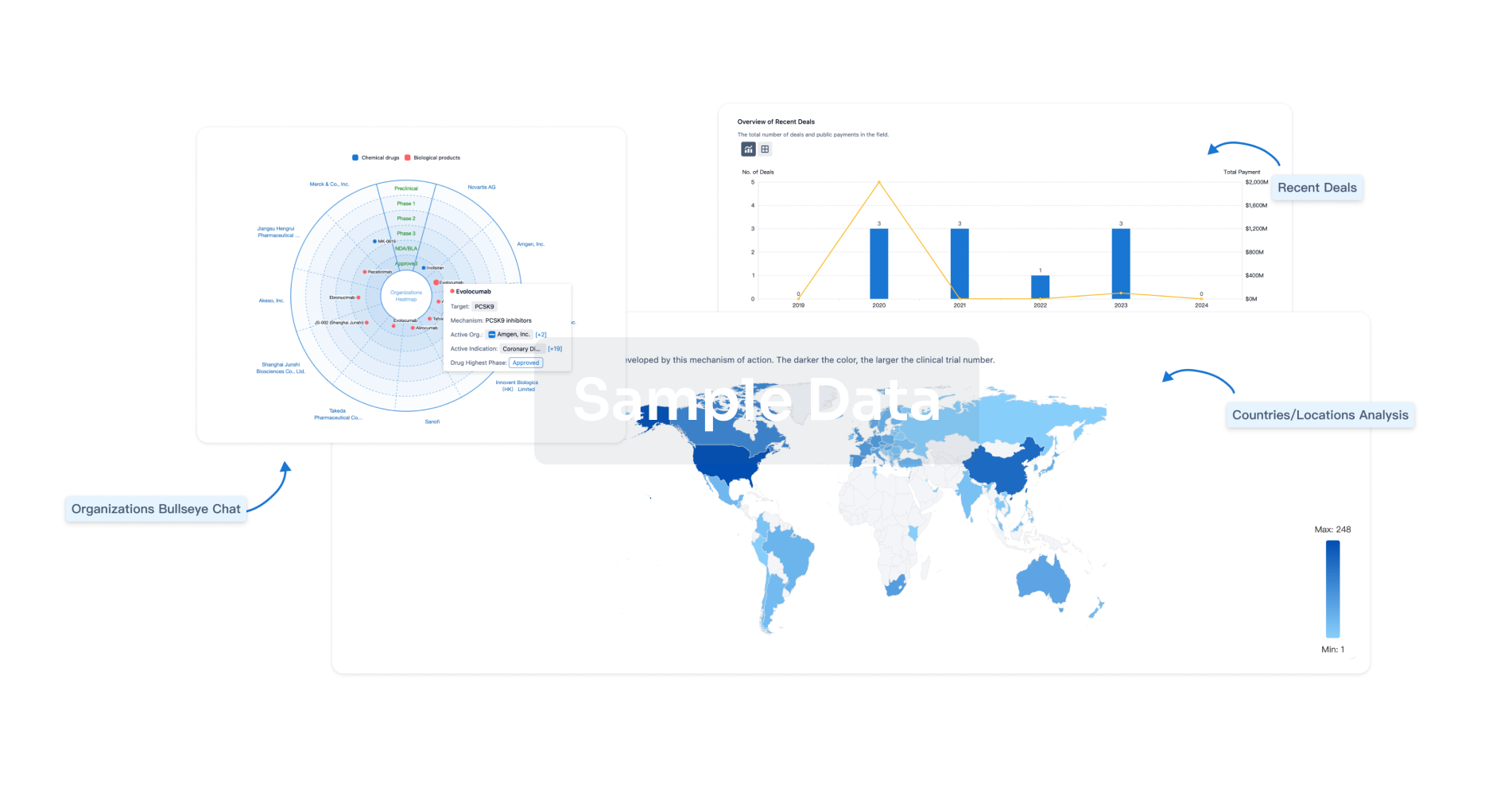
Analysis
Perform a panoramic analysis of this field.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free




