Request Demo
Last update 08 May 2025
Simian Acquired Immunodeficiency Syndrome
Last update 08 May 2025
Basic Info
Synonyms AIDS, Simian, AIDS-サル, AIDS-猿 + [26] |
Introduction Acquired defect of cellular immunity that occurs naturally in macaques infected with SRV serotypes, experimentally in monkeys inoculated with SRV or MASON-PFIZER MONKEY VIRUS; (MPMV), or in monkeys infected with SIMIAN IMMUNODEFICIENCY VIRUS. |
Related
1
Drugs associated with Simian Acquired Immunodeficiency SyndromeTarget |
Mechanism DNMT1 inhibitors [+1] |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication |
Drug Highest PhaseApproved |
First Approval Ctry. / Loc. United States |
First Approval Date19 May 2004 |
2
Clinical Trials associated with Simian Acquired Immunodeficiency SyndromeNCT03643809
Epidemiology and Clinico-genetic Correlations of Auto-inflammatory Diseases
Systemic autoinflammatory diseases (SAIDs) are inflammatory conditions caused by a defect of the innate immune system. Most are hereditary, but little is known on recent entities. The investigators aim to (1) establish correlations between the main mutations and symptoms presented by patients (genotype-phenotype correlation), and (2) describe the most recently described clinical, genetic, and demographic characteristics of SAIDs.
Start Date07 Jul 2018 |
Sponsor / Collaborator |
NCT02985190
A Phase II Study of Efficacy and Tolerance of Azacitidine (AZA) In MDS-associated Steroid Dependent/Refractory Systemic Auto-immune and Inflammatory Disorders (SAID)
This study is a phase II of effcicacy and tolerance of azacitidine in patients with myelodysplatic syndrome and steroid dependent or resistent systemic auto-immune and inflammatory disorders
Start Date26 Jan 2017 |
Sponsor / Collaborator |
100 Clinical Results associated with Simian Acquired Immunodeficiency Syndrome
Login to view more data
100 Translational Medicine associated with Simian Acquired Immunodeficiency Syndrome
Login to view more data
0 Patents (Medical) associated with Simian Acquired Immunodeficiency Syndrome
Login to view more data
714
Literatures (Medical) associated with Simian Acquired Immunodeficiency Syndrome01 Jun 2025·Nutrition, Metabolism and Cardiovascular Diseases
Causal effects and mediating pathways of metabolic dysfunction-associated fatty liver disease on novel subtypes of adult-onset diabetes: A two-step Mendelian randomization study
Article
Author: Fan, Yawei ; Luo, Hongping ; Wang, Ting ; Tian, Ye ; Li, Rongrong ; Guan, Yan
01 Apr 2025·The American Journal of Emergency Medicine
Case report: Hyponatremia due to syndrome of inappropriate antidiuresis associated with normal pressure hydrocephalus
Article
Author: Martin, Julia ; McCoin, Nicole ; Marcum, Samuel
01 Apr 2025·Brain Research Bulletin
Differential tissue and cellular distribution of chemokine C-C motif ligand 2 in grey/white matters of healthy and simian immunodeficiency virus infected monkey
Article
Author: Xiong, Huangui ; Zhu, Junyi ; Shi, Xue ; Li, Hongjun ; Zhao, Huangying ; Zhang, Jingdong
Analysis
Perform a panoramic analysis of this field.
login
or
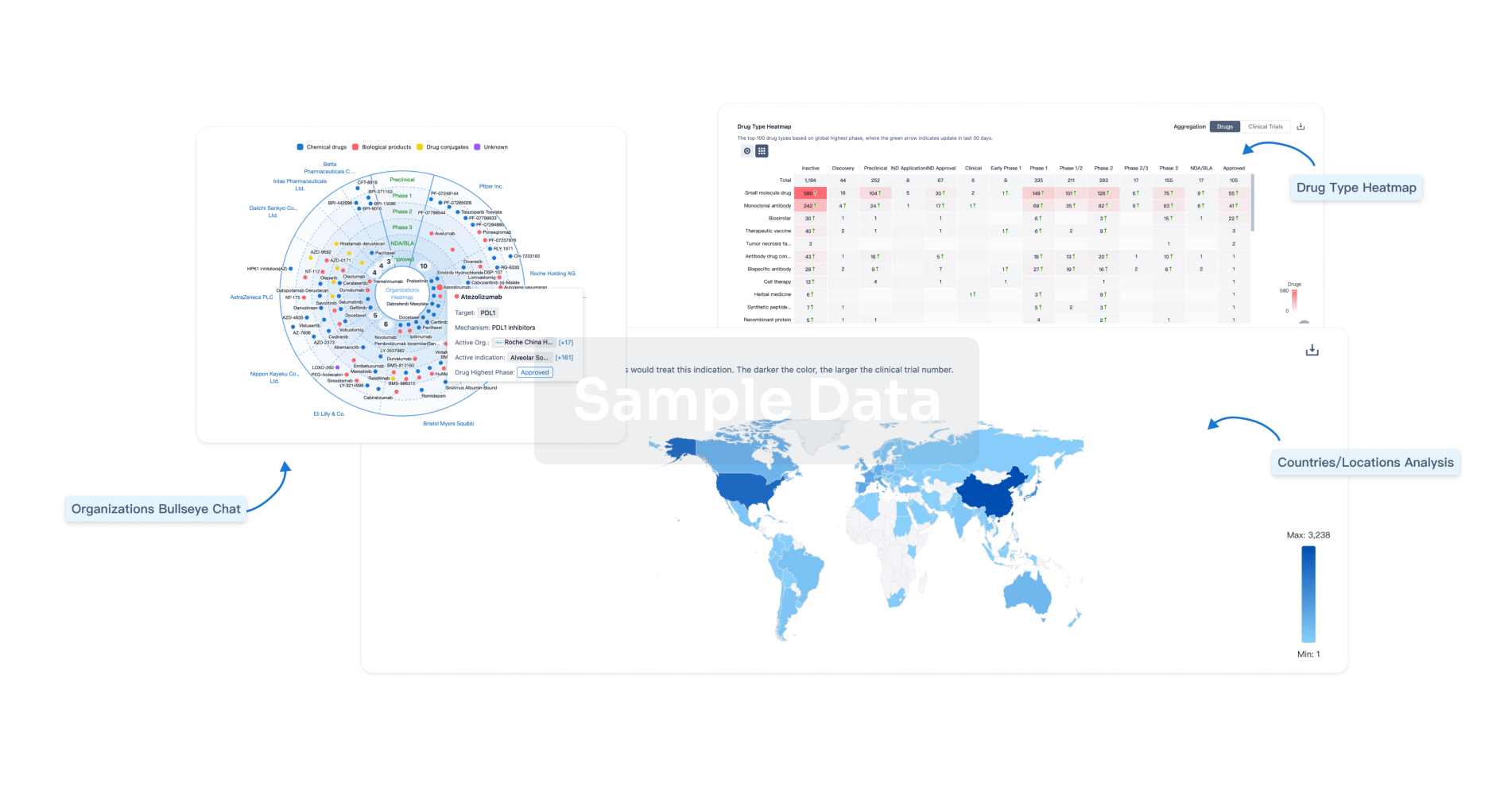
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free