Request Demo
Last update 08 May 2025
Post embolisation syndrome
Last update 08 May 2025
Basic Info
Synonyms Post embolisation syndrome, Post embolization syndrome, 塞栓術後症候群 + [1] |
Introduction- |
Related
23
Clinical Trials associated with Post embolisation syndromeTCTR20240924006
Efficacy and safety of oral N-acetylcysteine in prevention of post embolization syndrome
Start Date05 Aug 2024 |
Sponsor / Collaborator |
NCT06039280
Comparison of Dexamethasone and N Acetylcysteine (NAC) Versus N Acetylcysteine (NAC) Alone in the Prevention of Post Embolization Syndrome in Patients With Hepatocellular Carcinoma Following Transarterial Chemoembolization - Randomized Controlled Trial.
N-acetylcysteine (NAC), a glutathione precursor and potent antioxidant, is known as a liver protector. As a steroid preparation, dexamethasone is known to have efficient anti-inflammation and immunosuppression effects. N-acetyl cysteine and Dexamethasone's roles in preventing post-embolization syndrome following TACE have each been researched individually in the past. Up until now, no study has been done that has compared dexamethasone and NAC in post-embolization syndrome. With this study, we aim to study the efficacy of combining dexamethasone with N-acetyl cysteine in the prevention of post-embolization syndrome within 72 hours among patients who undergo transarterial chemoembolization for HCC.
Start Date15 Sep 2023 |
Sponsor / Collaborator |
CTR20232391
羟苯磺酸钙胶囊在健康成年受试者空腹和餐后条件下、单中心、随机、开放、单次给药、两周期、两序列、自身交叉对照中的人体生物等效性试验
[Translation] A single-center, randomized, open-label, single-dose, two-period, two-sequence, self-crossover human bioequivalence study of calcium dobesilate capsules in healthy adult subjects under fasting and fed conditions
主要研究目的:以广东华南药业集团有限公司生产的羟苯磺酸钙胶囊(规格:0.5g)为受试制剂,以Klocke Pharma Service生产的羟苯磺酸钙胶囊(商品名:Doxium®,规格:0.5g)为参比制剂,研究受试制剂与参比制剂的吸收速度和吸收程度,评价两制剂在空腹/餐后条件下单次给药时的生物等效性。
次要研究目的:观察在空腹/餐后条件下单次口服两制剂在健康受试者中的安全性。
[Translation]
The main purpose of the study is to use calcium dobesilate capsules (specification: 0.5g) produced by Guangdong South China Pharmaceutical Group Co., Ltd. as the test preparation and calcium dobesilate capsules (trade name: Doxium®, specification: 0.5g) produced by Klocke Pharma Service as the reference preparation to study the absorption rate and extent of the test preparation and the reference preparation, and to evaluate the bioequivalence of the two preparations when administered in a single dose under fasting/postprandial conditions.
Secondary purpose of the study: To observe the safety of the two preparations in healthy subjects when administered orally in a single dose under fasting/postprandial conditions.
Start Date05 Aug 2023 |
Sponsor / Collaborator |
100 Clinical Results associated with Post embolisation syndrome
Login to view more data
100 Translational Medicine associated with Post embolisation syndrome
Login to view more data
0 Patents (Medical) associated with Post embolisation syndrome
Login to view more data
354
Literatures (Medical) associated with Post embolisation syndrome01 May 2025·British Journal of Radiology
PREDICTing Post-Embolization Syndrome after uterine fibroid embolization: the PREDICT-PES study
Article
Author: Lukies, Matthew W ; Venn, Georgina ; Coleman, Madeleine ; Le Mercier, Laura ; Nandurkar, Rohan ; Clements, Warren ; Koukounaras, Jim
01 May 2025·Clinical Imaging
Safety and efficacy of transarterial therapies for pancreatic acinar cell carcinoma metastases
Article
Author: Blume, Harrison ; Alexander, Erica S ; Zhao, Ken ; Petre, Elena N ; Yuan, Gavin ; Sotirchos, Vlasios ; Rodriguez, Lee ; Ziv, Etay
01 Apr 2025·Annals of Vascular Surgery
Dexamethasone-Based Prophylactic Therapy for Prevention of Post-Embolization Syndrome: A Systematic Review and Meta-Analysis Assessing Its Efficacy and Influence of Dosage and Timing in Patients Undergoing Arterial Embolization
Review
Author: Raza, Muhammad Zain ; Nadeem, Ali Ahmad ; Maqsood, Musab ; Omais, Muhammad ; Arshad, Hafiz Muhammad Ehsan ; Khwaja, Huzaifa Fayyaz
1
News (Medical) associated with Post embolisation syndrome23 Mar 2024
Defining a quantifiable threshold for embolization effectiveness
FAIRFAX, Va., March 23, 2024 /PRNewswire/ -- Early intervention with a minimally invasive treatment called uterine artery embolization (UAE) can help women avoid hysterectomy due to severe bleeding after childbirth, according to a new study being presented at the Society of Interventional Radiology Annual Scientific Meeting in Salt Lake City.
"These findings are important and may help more women avoid hysterectomy and other very serious complications of uncontrolled hemorrhage," said lead author Younes Jahangiri, M.D., a resident in the interventional and diagnostic radiology program at Michigan State University/Corewell Health. "As the medical community looks for ways to provide better care for women to address maternal health and peri-partum care, this is one more option on the table that could help many women."
The study was a retrospective review of 66 patients (median age, 31) who underwent UAE for uncontrolled postpartum hemorrhage at a single, high-volume medical center between 2014 and 2022. UAE successfully controlled postpartum hemorrhaging in 62 of the 66 patients (94%). Four patients required hysterectomies to stop the bleeding, all of whom lost at least 2400 ml blood prior to presentation for UAE and symptoms of diffuse intravascular coagulopathy, a clotting abnormality that can happen after large-volume hemorrhage due to rapid consumption of clotting factors.
Postpartum hemorrhage is a rare but potentially deadly complication of childbirth. To stop it, obstetricians will initially use conservative approaches to replace the lost blood or to promote clotting. If these measures are insufficient, hysterectomy is usually performed. Alternatively, interventional radiologists can be brought in to perform UAE, injecting tiny particles into the arteries that supply blood to the uterus using fluoroscopic imaging guidance. Once placed in the arteries, the particles temporarily block blood flow to stem uterine bleeding.
"Based on these findings, we would encourage obstetricians to involve interventional radiologists early, to be ready to perform UAE if more conservative approaches are not managing postpartum hemorrhage," said senior author James Morrison, M.D., assistant professor of interventional radiology, also at Michigan State University's College of Human Medicine.
Researchers in this study found a 36% incidence of post-embolization syndrome, which presents with abdominal pain and flu-like symptoms. The study found that it was more likely to occur in patients who experienced greater blood loss before embolization.
Dr. Jahangiri, Dr. Morrison and their colleagues plan to expand their research to include multiple institutions and ultimately to conduct a prospective study that examines longer-term outcomes of UAE.
Abstract #189: Short-Term and Long-Term Outcomes of Uterine Artery Embolization for Treatment of Uncontrolled Post-Partum Hemorrhage. Y. Jahangiri, J. Haan, O. Lane, O. Close, J. Morrison. Annual Scientific Meeting, March 23-28, 2024. This abstract can be found at sirmeeting.org.
About the Society of Interventional Radiology
The Society of Interventional Radiology is a nonprofit, professional medical society representing more than 8,000 practicing interventional radiology physicians, trainees, students, scientists and clinical associates, dedicated to improving patient care through the limitless potential of image-guided therapies. SIR's members work in a variety of settings and at different professional levels—from medical students and residents to university faculty and private practice physicians. Visit sirweb.org.
The Society of Interventional Radiology is holding its Annual Scientific Meeting in Salt Lake City, March 23-28, 2024. Visit sirmeeting.org.
SOURCE Society of Interventional Radiology
Clinical Result
Analysis
Perform a panoramic analysis of this field.
login
or
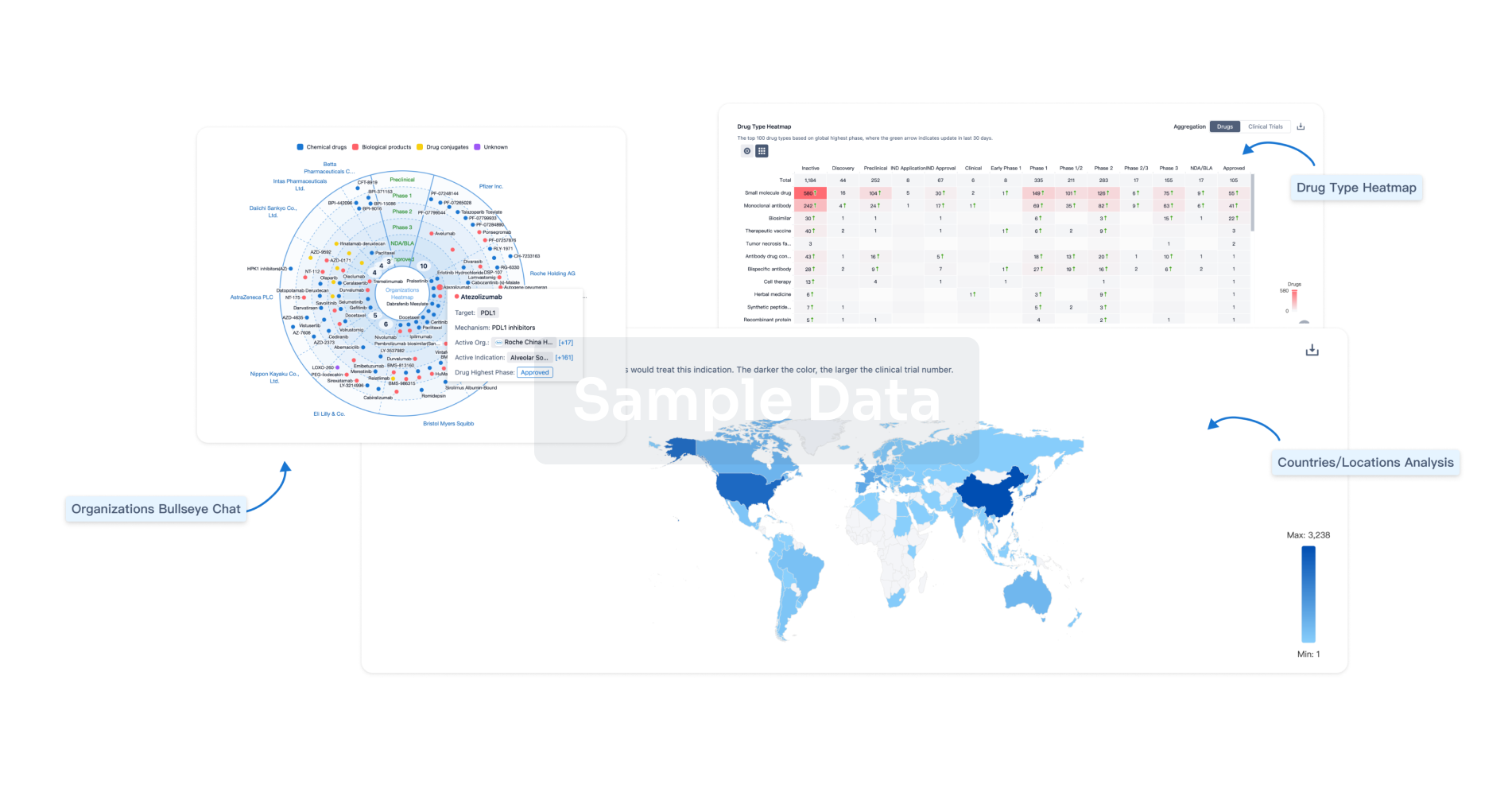
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
