Request Demo
Last update 27 Feb 2026
Imdusiran
Last update 27 Feb 2026
Overview
Basic Info
Drug Type siRNA |
Synonyms Imdusiran Sodium, AB 729, AB-729 + [1] |
Target |
Action inhibitors |
Mechanism HBsAg inhibitors(HBsAg inhibitors) |
Therapeutic Areas |
Active Indication |
Inactive Indication- |
Originator Organization |
Active Organization |
Inactive Organization |
License Organization |
Drug Highest PhasePhase 2 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Boost your research with our RNA technology data.
login
or
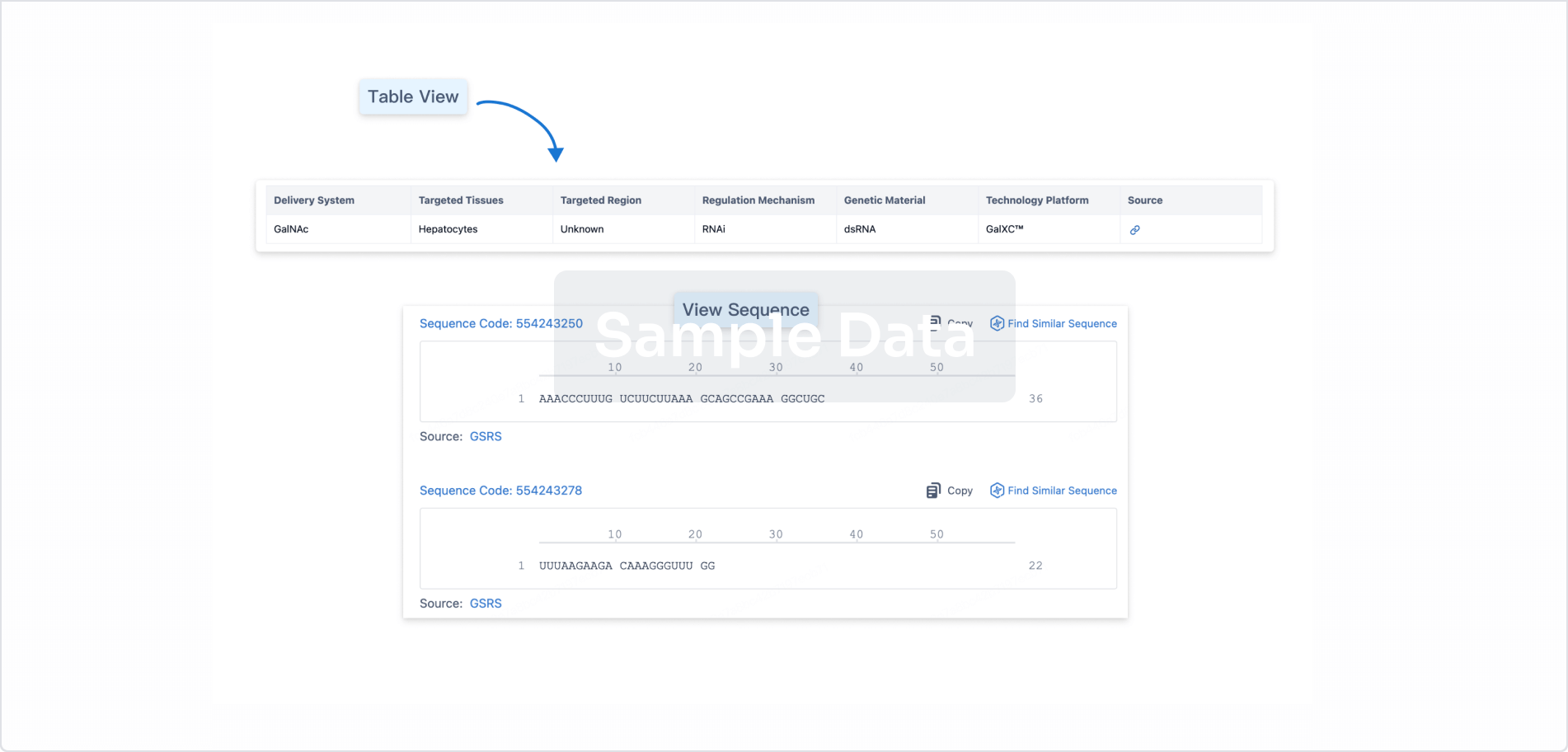
Sequence Code 453110990
Source: *****
Sequence Code 453110991
Source: *****
Related
7
Clinical Trials associated with ImdusiranNCT06154278
Pilot Study to Evaluate Intrahepatic and Peripheral Responses to Small Interfering RNA, Imdusiran (AB-729), Among People With Chronic Hepatitis B
The goal of this clinical trial is to learn about the action of Imdusiran (AB-729) in the liver of people with chronic hepatitis B. The main questions it aims to answer are:
* how well is it working in the liver
* how does Imdusiran affect the hepatitis B virus
Participants will receive injections of Imdusiran, one injection every 8 weeks, for a total of 4 doses. They will also undergo 2 liver biopsies: one with the first dose of Imdusiran, and the second 8 weeks after the last dose of Imdusiran.
* how well is it working in the liver
* how does Imdusiran affect the hepatitis B virus
Participants will receive injections of Imdusiran, one injection every 8 weeks, for a total of 4 doses. They will also undergo 2 liver biopsies: one with the first dose of Imdusiran, and the second 8 weeks after the last dose of Imdusiran.
Start Date25 Jul 2024 |
Sponsor / Collaborator |
NCT06245291
A Phase 2a, Open-Label Multiple Dose Study Evaluating the Safety, Tolerability, and Pharmacodynamics of Imdusiran (AB-729) in Combination With Intermittent Dosing of Durvalumab, a PD-L1 Monoclonal Antibody, in Subjects With Chronic HBV Infection
This is a phase 2a, open-label, multicenter study investigating the safety, tolerability, and antiviral activity of durvalumab administered at targeted times during a 48-week treatment period of imdusiran in virologically-suppressed CHB subjects
Start Date01 May 2024 |
Sponsor / Collaborator |
ACTRN12622000317796
A Phase 2a, Randomized, Blinded, Multicenter Study Investigating a Combination of AB-729 and VTP-300 to evaluate their safety and reactogenicity in Virologically-Suppressed Chronic Hepatitis B Participants.
Start Date02 Jun 2022 |
Sponsor / Collaborator |
100 Clinical Results associated with Imdusiran
Login to view more data
100 Translational Medicine associated with Imdusiran
Login to view more data
100 Patents (Medical) associated with Imdusiran
Login to view more data
3
Literatures (Medical) associated with Imdusiran11 Oct 2024·ACS Infectious Diseases
Control of Hepatitis B Virus with Imdusiran, a Small Interfering RNA Therapeutic
Article
Author: Cuconati, Andrea ; Paratala, Bhavna ; Thi, Emily P. ; Graves, Ingrid E. ; Ye, Xin ; Rijnbrand, Rene ; McClintock, Kevin ; Micolochick Steuer, Holly M. ; Espiritu, Christine ; Sofia, Michael J. ; Lee, Amy C. H. ; Harasym, Troy ; Jarosz, Agnes ; Snead, Nicholas M. ; Teng, Xiaowei ; Abbott, Cory ; Ardzinski, Andrzej ; Lam, Angela M.
Chronic hepatitis B is a global health concern with a high risk of end-stage liver disease. Current standard-of-care agents have low cure rates, and new therapies are needed. Small interfering RNAs (siRNAs) that target viral RNAs fulfill a gap not addressed by standard-of-care agents and may contribute to a functional cure. Here, we describe the preclinical characterization of imdusiran (AB-729), a novel, pan-genotypic siRNA therapeutic that effectively reduces HBsAg, viral antigens, and viral replication in chronic hepatitis B patients and is currently in Phase 2 clinical studies. In hepatitis B virus (HBV) cell-based systems, imdusiran possessed pan-genotypic nanomolar potency and retained activity against HBV target site polymorphisms. Imdusiran was active against nucleos(t)ide analogue- and capsid assembly modulator-resistant HBV isolates, and combination with standard-of-care agents was additive. In an HBV adeno-associated virus mouse model, HBsAg was reduced up to 3.7 log10 after a single imdusiran dose, with sustained suppression for 10 weeks. Imdusiran did not intrinsically stimulate cytokine release in healthy donor human whole blood, supportive of its mechanism of action as a direct acting RNA interference antiviral. Taken together, these data support imdusiran in combination treatment approaches toward chronic hepatitis B functional cure.
Hepatology communications
Measuring hepatitis B pgRNA stability using an updated automated HBV pgRNA assay with increased sensitivity
Article
Author: Anderson, Mark ; Stec, Michael ; Thi, Emily P. ; Mbanya, Dora ; Picchio, Gaston ; Cloherty, Gavin
Background::
HBV pregenomic RNA (pgRNA) is a circulating biomarker for covalently closed circular DNA activity in HBV-infected individuals and has been studied for treatment efficacy, disease staging, and off-therapy outcomes; however, data on the stability are scarce. Increasing HBV pgRNA assay sensitivity may improve its predictive value and provide additional insights at low viral levels.
Methods::
Modifications to a fully automated first (v1) generation HBV pgRNA assay improved sensitivity up to 15-fold over the previous assay. Flexible sample input volumes yielded lower limits of quantitation of 10 and 22 copies/mL for 0.6 and 0.2 mL assays, respectively. Results are standardized to secondary standards that are traceable to the WHO HBV DNA standard, and internal and external controls are included.
Results::
Comparison between v1 and modified v2 assays showed increased sensitivity from 152 copies/mL with v1 to 10 (0.6 mL) and 22 (0.2 mL) copies/mL with v2, respectively. Quantitated v2 results were indistinguishable from v1, indicating that comparisons can be made to previous studies. Single timepoint treatment-naive blood donors or longitudinal draws from patients with chronic hepatitis B on AB-729, an investigational siRNA therapy, showed improved detection and quantifiable pgRNA with v2 compared with v1. Stability testing demonstrated excellent HBV pgRNA plasma stability after 3 freeze-thaw cycles, for at least 7 days at 25–37 °C and at least 30 days at 4°C, with ≤0.25 Log U/mL decrease.
Conclusion::
HBV pgRNA v2 assays with increased sensitivity and flexible input volumes demonstrated increased detection and quantitation of low viral titer samples. Highly sensitive HBV pgRNA assays may be useful in refining predictive treatment outcomes based on this marker. HBV pgRNA was stable under multiple conditions, which increases the reliability of this marker.
AIDS reviewsQ4 · MEDICINE
Hepatitis B Gene Therapy Coming to Age.
Q4 · MEDICINE
Review
Author: Soriano, Vicente
The major pandemics caused by chronic viral infections is produced by HIV, hepatitis C virus (HCV), and hepatitis B virus (HBV), with estimates of 38, 70, and 250 million people worldwide, respectively (Fig. 1). During the last couple of years, the advent of direct oral antivirals has allowed pursuing global HCV eradication. In an unprecedented manner, these drugs cure more than 95% of hepatitis C patients when given for only 2-3 months. The enthusiasm on HCV has renewed the interest for curative strategies for both HIV and HBV. However, important biological differences between all three viruses may preclude envisioning a similar rapid success for either HIV or HBV than for HCV infection. As shown in figure 1, once infection of targeted cells has occurred, the viral genetic material only replicates in the cytosol for HCV whereas it enters the nucleus and integrates into the chromosomes as provirus for HIV or is converted in a circular covalently closed form (cccDNA) for HBV (Fig. 1). Blocking viral nucleic acid replication for a minimum lag of time allows definitive clearance of HCV infection, with degradation of residual cytoplasmic HCV-RNA strands. In contrast, blocking viral replication has only a transient effect on HIV or HBV, as mRNA expression resumes following treatment discontinuation, given the stability of the HIV provirus or the HBV cccDNA, respectively. The European Liver meeting took held in Paris on April 2018. A relatively large number of presentations addressed distinct new hepatitis B therapeutic strategies. Table 1 summarizes some of the molecules that have been investigated so far with more promising results, grouping them into distinct drug classes (Soriano et al. Exp Op Inv Drugs 2017;26:843-51), based on their distinct mechanism of action and targeted steps in the HBV life cycle (Fig. 2). Considering the pros and cons of novel HBV therapeutic candidates, it has become apparent new HBV gene therapies among the most attractive. Several advances have contributed to position gene therapy in front within the experimental HBV armamentarium. First, progresses in delivery systems, including the use of polymers and nanoformulations have allowed developing easier forms of administration that now are becoming subcutaneous and monthly. Second, the synthetic production of oligonucleotide formulations has reduced costs. Third, the specificity against HBV is higher than for other experimental agents, as immune modulators that enhance innate immunity, such as TLR agonists (i.e., GS-9620) or checkpoint inhibitors (i.e., nivolumab). Fourth, significant declines in serum hepatitis B surface antigen (HBsAg) are demonstrated during gene therapy, which have never been seen using the most potent polymerase inhibitors (i.e., tenofovir or entecavir). Finally, unanticipated significant reductions in cccDNA are seen with HBV gene therapy, most likely as prove of an indirect benefit of waning the immunosuppressive effect of large over amounts of HBsAg released by infected hepatocytes that contributes to T-cell exhaustion. In a pioneering study, Roche was the first to publish the potent effect of an oral small molecule that blocked HBV gene expression (Mueller et al. J Hepatol 2018;68:412-20). The drug belonged to the dihydroquinolizinone class, and directly or indirectly modified viral RNAs, promoting their degradation. This posttranscriptional silencing was accompanied by rapid drops in HBV-DNA and more importantly in serum HBsAg in the humanized mice. However, Roche decided to discontinue any further clinical development of the drug. Nowadays, two major groups of agents are being developed as HBV gene therapies. At this time, interference RNA (iRNA) molecules and nucleic acid polymers (NAPs) are the most promising. Overall, iRNA is double-stranded RNA molecules, 20 nucleotides long. One strand matches a segment of specific HBV mRNA and induces its degradation. Several iRNA molecules have entered into Phase II clinical trials (Flisiak et al. Exp Op Biol Ther, in press), including ARB-1467 and AB-729 (Arbutus), ARO-HBV (Arrowhead), ALN-HBV (Alnylam), and IONIS-HBVRx (Ionis). In most cases, they are tested as part of combination therapy with nucleos(t)ide analogs and/or peginterferon. NAPs are phosphorothioate 40 length oligonucleotides that no map any HBV sequence. However, they interact with a liver host target protein (apolipoprotein-like) and result in specific inhibition of HBV mRNAs. This is followed by rapid suppression of HBsAg release (Roehl et al. Mol Ther Nuc Acids 2017;8:1-12). In a pilot study with intravenous REP-2139, investigators from Replicor demonstrated strong reductions in HBV-DNA along with significant drops in HBsAg and seroconversion in some patients. More interestingly was the recognition of significant reductions in hepatic cccDNA, most likely a result of an indirect effect following the removal of large amounts of HBsAg from the bloodstream that contributes to impaired T-cell responses in chronic hepatitis B patients (Bazinet et al. EASL, Paris 2018; abstract FRI-343). An improved NAP, named REP-2165 and subcutaneous administration are currently being tested.
131
News (Medical) associated with Imdusiran27 Jan 2026
Insilico Medicine unveiled its cardiometabolic disease portfolio in November.\n Qilu Pharmaceutical has struck a deal to tap into Insilico Medicine’s artificial intelligence drug development capabilities, offering up to $120 million to collaborate on small molecules for treating cardiometabolic diseases.Insilico has established itself at the forefront of efforts to use AI to improve drug development over the past decade. Using a range of AI tools, the Hong Kong-listed biotech discovers drug targets, generates molecules and otherwise seeks to automate and accelerate R&D. The platform has yielded a phase 2b/3 lung disease candidate and deals with companies including Eli Lilly, Sanofi and Servier. China’s Qilu has now joined the ranks of those Insilico partners. Insilico will use its Pharma.AI platform, the umbrella for its array of AI tools, to design and optimize small molecules against specific, undisclosed targets for cardiometabolic disease management. Examples of cardiometabolic diseases include obesity, Type 2 diabetes and heart failure. The partners are yet to specify which diseases they are targeting.Once Insilico has designed and optimized the molecules, Qilu will handle all further development and commercialization of the assets. Qilu’s R&D team, which employs more than 5,000 people, has delivered more than 300 products, including 55 that were first to launch in China. The company’s pipeline spans more than 200 programs. Qilu has put up almost $120 million, including development and commercialization milestone payments, for the chance to add cardiometabolic disease candidates to its pipeline. Neither party has disclosed the size of the upfront fee, with Insilico’s press release and financial regulatory filing (PDF) only giving the total figure including all milestones. Upfront fees are typically a small part of Insilico’s deals, as is common across the industry for agreements covering early-stage assets. Insilico’s IPO paperwork revealed (PDF) that the company received about $12 million upfront in its deal with Sanofi and $20 million from one of its pacts with Stemline Therapeutics. Exelixis paid a larger upfront, $80 million, but secured a phase 1-ready asset in return.The Qilu deal follows Insilico’s unveiling of its cardiometabolic disease portfolio in November. With cash flooding into the space after the success of Eli Lilly and Novo Nordisk, Insilico revealed small molecules designed to realize the full potential of established targets such as GLP-1R, GIPR, amylin, APJ and Lp(a). The portfolio includes an oral small molecule GLP-1 receptor agonist designed for once-weekly dosing. Qilu made changes to its pipeline last year, paying about $38 million for a B7-H3-targeted antibody-drug conjugate from Minghui Pharmaceutical and severing its ties to Arbutus Biopharma’s hepatitis B candidate imdusiran.
IPOPhase 1ADC
08 Jan 2026
GSK said that the drug met its primary endpoint, with more patients achieving functional cure with bepirovirsen plus standard of care compared to standard of care alone. Image credit: Magda Wygralak / Shutterstock.com
GSK’s six-monthly triple-action investigational antisense oligonucleotide (ASO) candidate has demonstrated a clinically and statistically significant functional cure in chronic hepatitis B in two Phase III trials.
The B-Well 1 (NCT05630807) and B-Well 2 (NCT05630820) studies, which enrolled over 1,800 patients from 29 countries, met their primary endpoint, and bepirovirsen demonstrated a statistically significant and clinically meaningful functional cure rate.
Functional cure rates were significantly higher with
bepirovirsen
plus standard of care (SoC) compared with SoC alone.
All ranked endpoints were statistically significant, including in patients with baseline surface antigen (HBsAg) <=1000 IU/ml where an even greater effect was demonstrated. The drug also proved to be safe and tolerable in the trials.
Based on the Phase III trials, GSK will be filing for regulatory approval of the drug globally. Full data will be presented at an upcoming medical meeting.
Tony Wood, chief scientific officer, GSK, said: “Bepirovirsen has the potential to transform treatment goals for people living with CHB by achieving significant functional cure rates – a first for the disease. CHB affects more than 250 million people and leads to approximately 56% of liver cancer cases worldwide. Today’s result supports our plans to progress bepirovirsen as a treatment and also continue its development as a backbone in future sequential therapies.”
GlobalData Strategic Intelligence
US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData
Learn more about Strategic Intelligence
Current SoC for hepatitis B is nucleoside and nucleotide analogues, which often require lifelong therapy and the functional cure rates remain low, typically only 1%.
Bepirovirsen acts by inhibiting the replication of viral DNA in the body, suppressing the level of hepatitis B surface antigen (HBsAg) in the blood, and stimulating the immune system to increase the chances of a durable and sustained response.
GSK licensed the drug from Ionis in 2019, following a positive Phase II trial, and collaborated with the company on its development.
The drug gained Fast Track designation from the US Food and Drug Administration (FDA), Breakthrough Therapy designation from the Chinese National Medical Products Administration (NMPA) and SENKU designation from the Japanese Pharmaceuticals and Medical Devices Agency (PMDA).
GlobalData predicts the
hepatitis B therapeutics market
to reach $3.2bn across seven major markets (7MM: the US, France, Germany, Italy, Spain, the UK, and Japan) in 2034. By this year, more than 65% of the market will be attributed to sales from specific functional cure drugs.
As well as bepirovirsen, GlobalData also believes that a host of rival drugs will launch before 2034. This includes Gilead Sciences’ toll-like receptor 8 (TLR8) agonist, selgantolimod; GSK’s small interfering ribonucleic acid, daplusiran plus tomligisiran; Aligos Therapeutics’ capsid protein inhibitor, ALG-000184; and Arbutus Biopharma’s hepatitis B virus (HBV) surface antigen inhibitor, imdusiran.
Stephanie Kurdach, infectious disease analyst at GlobalData, said: “Functional cure drugs are projected to be more expensive than the currently marketed chronic hepatitis B therapeutics, thereby driving the growth of the market. By 2034, the forecasted functional cure drugs will account for over 65% of the chronic hepatitis B market sales.”
GlobalData is the parent company of
Clinical Trials Arena
.
Clinical ResultPhase 3Phase 2Fast TrackBreakthrough Therapy
13 Nov 2025
WARMINSTER, Pa., Nov. 13, 2025 (GLOBE NEWSWIRE) -- Arbutus Biopharma Corporation (Nasdaq: ABUS) (“Arbutus” or the “Company”), a clinical-stage biopharmaceutical company focused on infectious disease, today reported third quarter 2025 financial results and provided a corporate update.
“The strength of our third quarter performance reflects our disciplined focus on executing strategic priorities,” said Lindsay Androski, President and CEO of Arbutus. “We are also excited to share additional analysis of imdusiran clinical data being conducted as part of our ongoing strategic review. Notably, in addition to the eight patients who initially achieved functional cure with imdusiran at 60mg in our Phase 2a trials, forty more patients across all cohorts discontinued nucleos(t)ide analogue therapy after meeting study-defined criteria. In total, a combined 46% of all Phase 2a patients were able to discontinue all treatment. All but one patient who achieved functional cure or who we are following after discontinuing nucleos(t)ide analogue therapy remain off all treatment long-term, now exceeding two years for some patients. Across our Phase 1b and Phase 2a trials, imdusiran has demonstrated sustained benefits in chronic hepatitis B patients, regardless of baseline hepatitis B surface antigen levels, hepatitis B virus DNA presence or absence, and hepatitis B e-antigen positivity or negativity. We remain dedicated to accelerating the development and potential approval of imdusiran.”
LNP Litigation
Arbutus continues to consult closely with and support its exclusive licensee, Genevant Sciences, to protect and defend Arbutus’s intellectual property, which is the subject of on-going lawsuits against Moderna and Pfizer/BioNTech. The Company, together with Genevant, is seeking fair compensation for Moderna’s and Pfizer/BioNTech’s use of Arbutus’s patented LNP technology that was developed with great effort and at a great expense, and without which Moderna’s and Pfizer/BioNTech’s COVID-19 vaccines would not have been successful. In the Moderna U.S. litigation, fact discovery, expert discovery and summary judgment briefing have been completed. A jury trial is scheduled for March 2026. In March 2025, the Company, alongside Genevant Sciences, filed five international lawsuits against Moderna and its affiliates seeking to enforce patents protecting the Company’s patented LNP technology across 30 countries. Public oral hearings for two of the five cases which are before the Unified Patent Court are scheduled for May 2026, and a trial in the Canadian case is set to begin in September 2027. The claim construction hearing for the lawsuit against Pfizer/BioNTech occurred in December 2024, and the court issued a claim construction ruling in September 2025, which construed the disputed claim terms in a manner the Company generally considers to be favorable.
Corporate Updates
The Company showcased four poster presentations featuring data from its hepatitis B virus (HBV) programs at AASLD 2025. One poster presented new analysis from the Company’s IM-PROVE I Phase 2a clinical trial showing beneficial clinical outcomes were observed across all evaluated HBV genotypes (A to E). The Company also had a Poster of Distinction highlighting AB-101’s maximal PD-L1 receptor occupancy between 68-100% at a 30mg daily dose. Today, the Company published an updated Corporate Presentation on its website, which includes the results of its recently completed analysis of imdusiran clinical data. In addition to the eight functional cures, an additional 40 patients across all cohorts in its Phase 2a trials met study-defined criteria for nucleos(t)ide analogue (NA) therapy discontinuation. In total, 46% (48/105) of all Phase 2a patients either achieved functional cure or remained off NA therapy for at least 48 weeks after discontinuing NA therapy following treatment with imdusiran. Eighteen patients consented to long-term follow-up, including all functionally cured patients and 10 patients who discontinued NA therapy. To date, 94% of those follow-up patients have remained off all treatment for between 58 to 109 weeks. One functionally cured patient seroreverted but remains virally suppressed and off all treatment. Additionally, 56% (5/9) of Phase 1b patients (only received imdusiran and NA therapy) who elected to discontinue NA therapy, remained off all treatment for at least 3 years. Imdusiran has also demonstrated steep and durable declines in HBV DNA, and, with NA therapy, achieved full HBV DNA suppression significantly faster than NA therapy alone. By week 18 of treatment with imdusiran and NA therapy, 100% of Phase 1b HBV DNA positive patients achieved HBV DNA levels below the level of quantification, The eight Phase 2a patients who achieved functional cure continue to have HBV DNA levels below the level of quantification. In 30 hepatitis B e-antigen (HBeAg) positive patients in our Phase 1 and 2a trials, HBeAg decreased in all patients in a dose-dependent manner.
In addition to the eight functional cures, an additional 40 patients across all cohorts in its Phase 2a trials met study-defined criteria for nucleos(t)ide analogue (NA) therapy discontinuation. In total, 46% (48/105) of all Phase 2a patients either achieved functional cure or remained off NA therapy for at least 48 weeks after discontinuing NA therapy following treatment with imdusiran. Eighteen patients consented to long-term follow-up, including all functionally cured patients and 10 patients who discontinued NA therapy. To date, 94% of those follow-up patients have remained off all treatment for between 58 to 109 weeks. One functionally cured patient seroreverted but remains virally suppressed and off all treatment. Additionally, 56% (5/9) of Phase 1b patients (only received imdusiran and NA therapy) who elected to discontinue NA therapy, remained off all treatment for at least 3 years. Imdusiran has also demonstrated steep and durable declines in HBV DNA, and, with NA therapy, achieved full HBV DNA suppression significantly faster than NA therapy alone. By week 18 of treatment with imdusiran and NA therapy, 100% of Phase 1b HBV DNA positive patients achieved HBV DNA levels below the level of quantification, The eight Phase 2a patients who achieved functional cure continue to have HBV DNA levels below the level of quantification. In 30 hepatitis B e-antigen (HBeAg) positive patients in our Phase 1 and 2a trials, HBeAg decreased in all patients in a dose-dependent manner.
Financial Results
Cash, Cash Equivalents and Investments
As of September 30, 2025, the Company had cash, cash equivalents and investments in marketable securities of $93.7 million compared to $122.6 million as of December 31, 2024. During the nine months ended September 30, 2025, the Company used $35.0 million in operating activities, which included one-time payments related to its restructuring efforts. This was partially offset by $3.9 million of proceeds from the exercise of stock options.
Revenue
Total revenue was $0.5 million for the quarter ended September 30, 2025, compared to $1.3 million for the same period in 2024. The decrease of $0.8 million was due to a decrease in license royalty revenues, primarily due to a decline in Alnylam’s sales of ONPATTRO.
Operating Expenses
Research and development expenses were $5.8 million for the quarter ended September 30, 2025, compared to $14.3 million for the same period in 2024. The decrease of $8.5 million was due primarily to cost savings from the Company’s decisions to streamline the organization to focus its efforts on advancing the clinical development of imdusiran and AB-101, which included ceasing all discovery efforts, discontinuing its IM-PROVE III clinical trial, and reducing the Company’s workforce.
General and administrative expenses were $3.0 million for the quarter ended September 30, 2025, compared to $4.5 million for the same period in 2024. This decrease was due primarily to cost-cutting efforts by the Company, which drove reductions in employee compensation-related expenses and legal fees.
Restructuring costs in the quarter ended September 30, 2025 were $0.1 million, and all remaining restructuring-related payments are expected to be made by the first quarter of 2026.
Net Loss
For the quarter ended September 30, 2025, the Company’s net loss was $7.7 million, or a loss of $0.04 per basic and diluted common share, as compared to a net loss of $19.7 million, or a loss of $0.10 per basic and diluted common share, for the quarter ended September 30, 2024.
Outstanding Shares
As of September 30, 2025, the Company had 192.0 million common shares issued and outstanding, as well as 14.9 million stock options and unvested restricted stock units outstanding.
About Imdusiran (AB-729)
Imdusiran is an RNAi therapeutic specifically designed to reduce all hepatitis B viral proteins and antigens including HBsAg, which is thought to be a key prerequisite to enable reawakening of a patient’s immune system to control the virus. Imdusiran targets hepatocytes using Arbutus’ novel covalently conjugated N-Acetylgalactosamine (“GalNAc”) delivery technology enabling subcutaneous delivery. To date, Arbutus has reported a total of eight patients with cHBV who have achieved a functional cure following treatment with imdusiran and NA therapy in combination with either IFN or low dose nivolumab plus an immunotherapeutic, with seven out of the eight patients continuing to sustain functional cure for over a year after treatment. An additional 40 patients across our Phase 2a clinical trials were able to remain off NA therapy for at least 48 weeks after discontinuing NA therapy following treatment with imdusiran. Clinical data generated thus far has shown imdusiran to be generally safe and well-tolerated, while also providing meaningful reductions in HBsAg and hepatitis B virus DNA.
About HBV
Hepatitis B is a potentially life-threatening liver infection caused by HBV. HBV can cause chronic infection which leads to a higher risk of death from cirrhosis and liver cancer. cHBV infection represents a significant unmet medical need. The World Health Organization estimates that over 250 million people worldwide suffer from cHBV infection, while other estimates indicate that approximately 2 million people in the United States suffer from cHBV infection. Approximately 1.1 million people die every year from complications related to cHBV infection despite the availability of effective vaccines and current treatment options.
About Arbutus
Arbutus Biopharma Corporation (Nasdaq: ABUS) is a clinical-stage biopharmaceutical company focused on infectious disease. The Company is currently developing imdusiran (AB-729) and an oral PD-L1 inhibitor (AB-101) for the treatment of cHBV infection. The Company is also consulting closely with and supporting its exclusive licensee, Genevant Sciences, to protect and defend its intellectual property, which is the subject of on-going lawsuits against Moderna and Pfizer/BioNTech for use of Arbutus’s patented LNP technology in their COVID-19 vaccines. For more information, visit www.arbutusbio.com.
Forward-Looking Statements and Information
This press release contains forward-looking statements within the meaning of the Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934, and forward-looking information within the meaning of Canadian securities laws (collectively, forward-looking statements). Forward-looking statements in this press release include statements about: the potential to lead to a functional cure for HBV and/or the discontinuation of HBV therapies after treatment with Arbutus’ product candidates; the durability of clinical benefits from Arbutus’ product candidates; the potential for Arbutus’ product candidates to achieve success in clinical trials; Arbutus’ pipeline and development plans for its cHBV programs; and Arbutus’ plans with respect to the ongoing patent litigation matters, and the expected timing thereof.
With respect to the forward-looking statements contained in this press release, Arbutus has made numerous assumptions regarding, among other things: the effectiveness and timeliness of clinical trials, and the usefulness of the data; the continued demand for Arbutus’ assets; and the stability of economic and market conditions. While Arbutus considers these assumptions to be reasonable, these assumptions are inherently subject to significant business, economic, competitive, market and social uncertainties and contingencies. Additionally, there are known and unknown risk factors which could cause Arbutus’ actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by the forward-looking statements contained herein. Known risk factors include, among others: ongoing and anticipated clinical trials may be more costly or take longer to complete than anticipated, and may never be initiated or completed, or may not generate results that warrant future development of the tested product candidate; Arbutus may elect to change its strategy regarding its product candidates and clinical development activities; Arbutus may not receive the necessary regulatory approvals for the clinical development of Arbutus’ product candidates; uncertainties associated with litigation generally and patent litigation specifically; economic and market conditions may worsen; market shifts may require a change in strategic focus; Arbutus’ workforce reduction and plans to reduce its net cash burn may not materially extend the cash runway and may create a distraction or uncertainty that may adversely affect its operating results, business, or investor perceptions; and risks related to the sufficiency of Arbutus’ cash resources for its foreseeable and unforeseeable operating expenses and capital expenditures.
A more complete discussion of the risks and uncertainties facing Arbutus appears in Arbutus’ Annual Report on Form 10-K, Arbutus’ Quarterly Reports on Form 10-Q and Arbutus’ continuous and periodic disclosure filings, which are available at www.sedar.com and at www.sec.gov. All forward-looking statements herein are qualified in their entirety by this cautionary statement, and Arbutus disclaims any obligation to revise or update any such forward-looking statements or to publicly announce the result of any revisions to any of the forward-looking statements contained herein to reflect future results, events or developments, except as required by law.
Arbutus Biopharma Corporation / ir@arbutusbio.com
Clinical ResultPhase 2VaccineFinancial Statement
100 Deals associated with Imdusiran
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Hepatitis B, Chronic | Phase 2 | Australia | 07 May 2021 | |
| Hepatitis B, Chronic | Phase 2 | Bulgaria | 07 May 2021 | |
| Hepatitis B, Chronic | Phase 2 | Canada | 07 May 2021 | |
| Hepatitis B, Chronic | Phase 2 | New Zealand | 07 May 2021 | |
| Hepatitis B | IND Application | China | 10 May 2022 | |
| Hepatitis B | IND Application | China | 10 May 2022 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
Phase 2 | 62 | rfrsvywgcn(wxwuaejkhv) = uuybhycvtv rmfubzscfw (xilnevywdh ) | Positive | 07 May 2025 | |||
rfrsvywgcn(wxwuaejkhv) = hnwudzrdth rmfubzscfw (xilnevywdh ) View more | |||||||
Phase 2 | 22 | qrizksfmxu(bywcbkmssl) = lbymlytgnx jvorthhxcr (gpyimpmiyn ) | Positive | 15 Nov 2024 | |||
Phase 2 | 43 | (A1: 24 wks IFN + 2 imdusiran doses + NA) | zlbfvvwwhl(lkqwutrurt) = fgdayjgvzs uhmhdovlqn (tjdlpwwhix ) View more | Positive | 01 Jun 2024 | ||
(A2: 24 wks IFN + NA) | zlbfvvwwhl(lkqwutrurt) = iosqdczcmi uhmhdovlqn (tjdlpwwhix ) View more | ||||||
Phase 2 | 65 | juekxgwyjk = lklyywclrb zgzwsoutjp (cjopijtgud, zvlujuyoog - fmzmcpxwxn) View more | - | 14 Nov 2023 | |||
juekxgwyjk = jojjqkidwk zgzwsoutjp (cjopijtgud, xgxgsgdoqu - dfhsuvlese) View more | |||||||
Phase 2 | 40 | imdusilan+VTP-300 | ydpjmnujfr(uqymmkxndl) = There were no serious adverse events, Grade 3 or 4 adverse events or treatment discontinuations. gvkegaustq (ofwtqwmqsh ) View more | Positive | 09 Nov 2023 | ||
imdusilan+placebo | |||||||
Phase 2 | HBV RNA transcripts | HBV DNA | hepatitis B surface antigen (HBsAg) | - | dbrkdqchwo(nwbxkckcct) = nbpxsymtuf wmbnulikvi (cgixqtuteg ) | Positive | 25 Jun 2022 | ||
Control GalNAc siRNA | dbrkdqchwo(nwbxkckcct) = csraxsdhyk wmbnulikvi (cgixqtuteg ) | ||||||
Phase 2 | 27 | hkmqnlnqhl(jabuinncys) = hjeregrilb jorfntmpdq (hrofpgiamy ) | Positive | 22 Jun 2022 |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or

Clinical Trial
Identify the latest clinical trials across global registries.
login
or

Approval
Accelerate your research with the latest regulatory approval information.
login
or

Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free






