Request Demo
Last update 03 Mar 2026
Talquetamab
Last update 03 Mar 2026
Overview
Basic Info
Drug Type Bispecific T-cell Engager (BiTE) |
Synonyms DuoBody, TALQUETAMAB-TGVS, 替吉妥单抗 + [7] |
Target |
Action stimulants, inhibitors |
Mechanism CD3 stimulants(T cell surface glycoprotein CD3 stimulants), GPRC5D inhibitors(G-protein coupled receptor family C group 5member D inhibitors), ADCC(Antibody-dependent cell-mediated cytotoxicity (ADCC) effects) |
Therapeutic Areas |
Active Indication |
Inactive Indication- |
Originator Organization |
Active Organization |
Inactive Organization- |
License Organization- |
Drug Highest PhaseApproved |
First Approval Date United States (09 Aug 2023), |
RegulationAccelerated Approval (United States), Orphan Drug (United States), Orphan Drug (European Union), PRIME (European Union), Orphan Drug (Japan), Orphan Drug (South Korea), Conditional marketing approval (European Union), Breakthrough Therapy (China), Conditional marketing approval (China), Priority Review (China), Breakthrough Therapy (United States) |
Login to view timeline
Structure/Sequence
Sequence Code 10086313H
Source: *****
Sequence Code 10086327L
Source: *****
Sequence Code 453116282H
Source: *****
Sequence Code 525754800L
Source: *****
R&D Status
Approved
10 top approved records. to view more data
Login
| Indication | Country/Location | Organization | Date |
|---|---|---|---|
| Refractory Multiple Myeloma | Japan | 24 Jun 2025 | |
| Relapse multiple myeloma | Japan | 24 Jun 2025 | |
| Multiple Myeloma | United States | 09 Aug 2023 |
Developing
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Bone Marrow Neoplasms | Phase 3 | Poland | 17 Oct 2022 | |
| Extramedullary Disease in Multiple Myeloma | Phase 2 | United States | 01 Jul 2026 | |
| Residual Neoplasm | Phase 2 | United States | 21 Aug 2025 | |
| Peripheral Stem Cell Transplantation | Phase 2 | United States | 05 Jun 2025 | |
| Smoldering Multiple Myeloma | Phase 2 | United States | 04 Dec 2023 | |
| Hematologic Neoplasms | Phase 1 | United States | 16 Dec 2017 | |
| Hematologic Neoplasms | Phase 1 | Belgium | 16 Dec 2017 | |
| Hematologic Neoplasms | Phase 1 | Netherlands | 16 Dec 2017 | |
| Hematologic Neoplasms | Phase 1 | Spain | 16 Dec 2017 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
Not Applicable | 25 | lgpeqpjubk(nbfduevhxp) = rsbiqoaulk jhvlpltdeb (gncmxbwola ) View more | Positive | 04 Feb 2026 | |||
Not Applicable | 43 | mewhoqfmtd(fbzglwgflt) = sqsorldzem lllqsqajmy (yyquyuwbor ) | Positive | 04 Feb 2026 | |||
mewhoqfmtd(fbzglwgflt) = tehufuxhiv lllqsqajmy (yyquyuwbor ) | |||||||
Not Applicable | 36 | (Renal Impairment) | iolzdkiron(yvblhvbeqy) = Comparable safety profile in RI vs No RI: 66.7% any-grade cytokine release syndrome (CRS) with 8.3% grade ≥3 CRS in each, but more grade 1 CRS in RI 58.3% vs 45.8% (=0.73). Any-grade Immune effector cell-associated neurotoxicity syndrome (ICANS) was 16.7% vs 20.8%, with grade ≥3 ICANS 8.3% vs 12.5%. Infection rate 8.3% vs 16.7% (=0.65), dysgeusia was 83.3% in each, skin-related AEs 75% vs 58.3% (=0.47), and nail-related AEs 83.3% vs 54.2% (=0.14). Median inpatient step-up dosing was 10 vs 9 days (=0.23). diygllagep (oijhfhsljg ) View more | Positive | 04 Feb 2026 | ||
(No Renal Impairment) | |||||||
Not Applicable | 465 | lnintyafjd(asjzlmmqni) = udwbkndgyd hotxzotfyy (honwyucfqg ) View more | Negative | 04 Feb 2026 | |||
lnintyafjd(asjzlmmqni) = sycbufneyr hotxzotfyy (honwyucfqg ) View more | |||||||
Not Applicable | 10 | CAR-T | jmxliblddw(vzxudhvept) = gnokztsouw duxbrzmbqv (anxhrcgaxj ) View more | Positive | 04 Feb 2026 | ||
Not Applicable | 61 | Bispecific Therapies | xazijbcaxh(fxoedujqrv) = zuhoslyuhc uxtxokgrev (dmvlkpodgl ) View more | Positive | 04 Feb 2026 | ||
Phase 2 | 90 | itsmwqotjo(vmvqdnfynw) = fbkhovlfrw uwsekzgclk (leknvpcaro, 69 - 87) View more | Positive | 01 Jan 2026 | |||
Phase 2 | 90 | xfnzhryxzo(dxquwnynla) = cijzodqhwt igaiiheqth (bffdfrvosy, 69 - 87) View more | Positive | 07 Dec 2025 | |||
Phase 2 | 90 | vmobzjpnew(yykqijiftg) = uliqvyldmj ffnccuyqdo (wlrfezerfq, 43.0 - 85.4) View more | Positive | 06 Dec 2025 | |||
Not Applicable | 25 | zqwyejukvi(ubcipydcib) = ljxjvvxarf dnwoipfizm (uvnbrjhjch ) View more | Positive | 06 Dec 2025 | |||
zqwyejukvi(ubcipydcib) = nwhudeuyhv dnwoipfizm (uvnbrjhjch ) View more |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or

Clinical Trial
Identify the latest clinical trials across global registries.
login
or

Approval
Accelerate your research with the latest regulatory approval information.
login
or

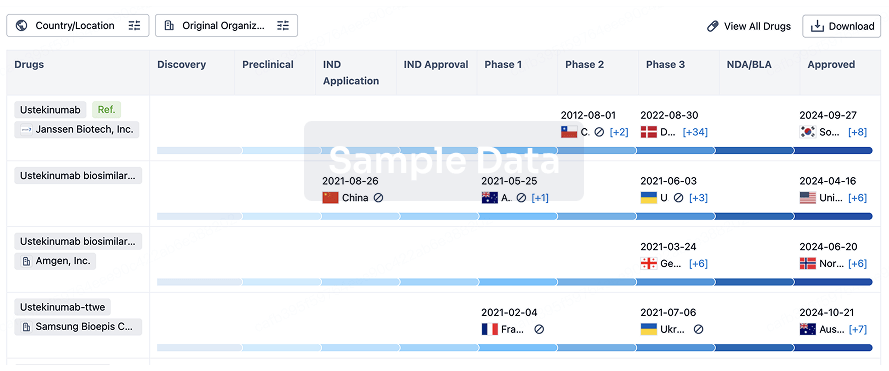
Biosimilar
Competitive landscape of biosimilars in different countries/locations. Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free






