4
Clinical Trials associated with Lamivudine/Zidovudine/Efavirenz / CompletedNot ApplicableIIT Investigating Influence of Pregnancy-induced Changes in Antiretroviral Pharmacokinetics, Together With Polymorphisms in Drug Disposition Genes, on Viral Decay Dynamics in HIV Positive Women Starting Therapy Late in Pregnancy and Postpartum
More than 150,000 babies became infected with HIV in 2015 alone. When HIV drugs are started before or early in pregnancy, HIV positive women can give birth to HIV negative baby. This is possible because HIV drugs can reduce the amount of the virus in the body to the extent that they become undetectable by the time of delivery and during the breastfeeding period. However, some women do not start taking these drugs on time because they become infected during pregnancy or lactation. This leads to detectable virus at the time of delivery and puts the baby at risk of becoming infected. Also, the amounts of HIV drugs in the body have to be at certain levels for them to work effectively. But findings from some research have recently showed that pregnancy increases the rate at which the body removes some HIV drugs used to prevent the transfer of HIV from mother to child. While this may not cause any problem in women with no detectable virus before pregnancy, it may affect the rate at which the HIV virus is removed from the body in those starting treatment late and may put the baby at risk. This project will investigate whether the changes in drug exposure caused by pregnancy or other factors have any effect on the rate at which the HIV virus is removed from the body. HIV positive pregnant women and those who recently delivered will be recruited from different hospitals and follow up will be until breastfeeding ends. The investigators will not be involved in treatment decisions and the primary care provider will be responsible for prescribing antiretroviral regimen based on current guidelines. Samples will be collected to measure levels of the virus and the drugs in three fluids that transfer the virus to the baby: blood, genital fluid, and breastmilk. The HIV status of the babies will be monitored until they stop breastfeeding.
The Adult Antiretroviral Treatment and Resistance Study (Tshepo)
The "Adult Antiretroviral Treatment and Resistance Study," hereafter referred to as "The Tshepo Study," is the first large-scale research study of antiretroviral therapy to treat AIDS and HIV infection in Botswana. The Tshepo Study is an open-label, randomized study comparing: (1) the rate of development and specific types of drug resistance mutations with various antiretroviral combination therapies to HIV-1C, the subtype of HIV found in southern Africa, and (2) the short and long-term effectiveness of two operational modifications of Directly Observed Therapy (DOT) medication adherence strategies for antiretroviral therapy. Specifically, treatment follow-up via the Standard of Care, the national standard of care as it evolves in Botswana, with intensive clinic-based follow up including regular adherence education sessions, will be compared to Community-Based Directly Observed Therapy (Com-DOT). Com-DOT involves the SOC with added community or family-based DOT. This Com-DOT component would involve a trained, community or family-based Medication Partner ("mopati") who observes the patient take his or medications daily.
Phase 3, Single Center, Controlled, Investigator-blinded, Randomized Matched Pair Design Study of CD4 Cell Recovery in HIV-1 Patients With Sustained Virologic Response Comparing Protease Inhibitor and Non-nucleoside Reverse Transcriptase Inhibitor Based Treatment Regimes
Therapy guidelines recommend the use of either the non-nucleoside reverse transcriptase inhibitor (NNRTI) efavirenz or a ritonavir-boostered protease inhibitor (PI) plus 2 nucleoside reverse transcriptase inhibitors (NRTI) as first-line treatment regimes of HIV-1 infection. Recent clinical studies suggest potential advantages of NNRTI- over PI-based regimes in therapy initiation due to lower rates of virologic failure and less metabolic side-effects. In contrast, PI regimes were claimed to cause greater increases in CD4 cell count than NNRTI regimes, which has been attributed to intrinsic antiapoptotic effects of the PI. However, it is still unclear whether the immunological response to a PI-containing regime is greater than to an NNRTI-containing regime, whether there is a difference in the extent of reduction of apoptosis between PI and NNRTI regimes and whether a difference in apoptosis is associated with a difference in CD4 cell recovery.
We conducted a controlled, long-term, random matched pair design study in HIV-1 infected individuals under sustained virologic suppression to evaluate in head-to-head comparison the clinical effects of a constant PI-based or NNRTI-based regime on CD4 cell recovery and the underlying molecular, biochemical and functional mechanisms.
100 Clinical Results associated with Lamivudine/Zidovudine/Efavirenz
100 Translational Medicine associated with Lamivudine/Zidovudine/Efavirenz
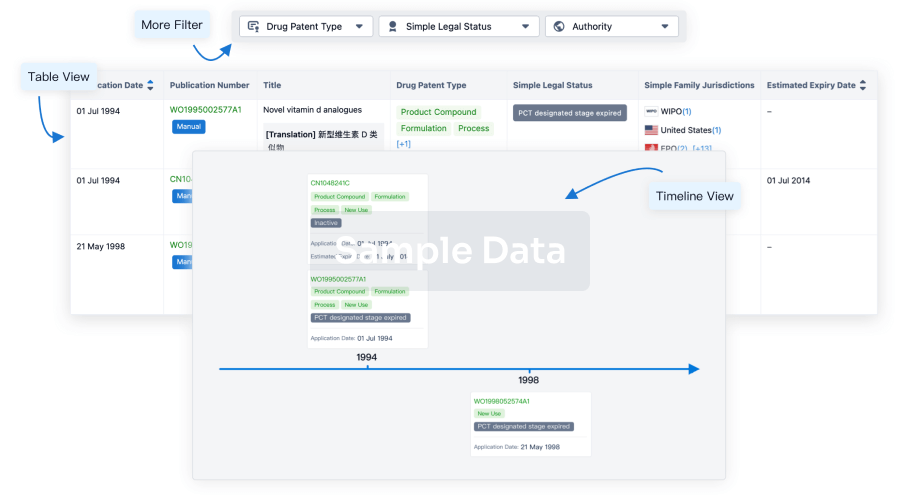
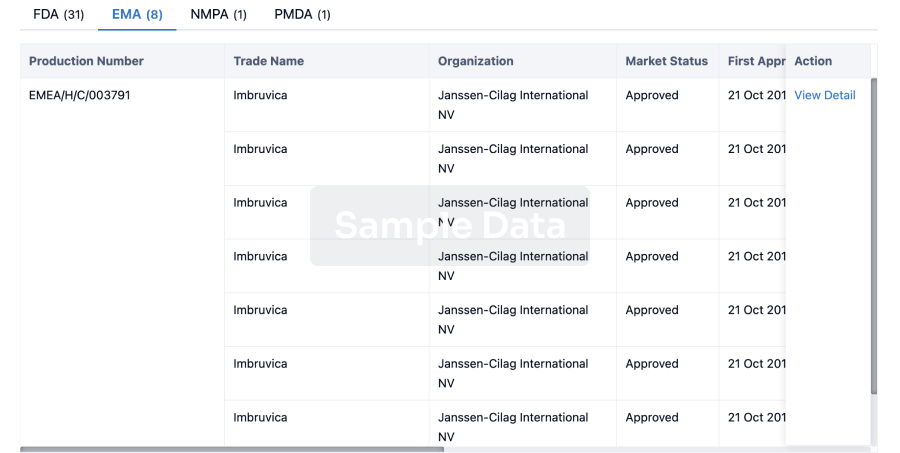
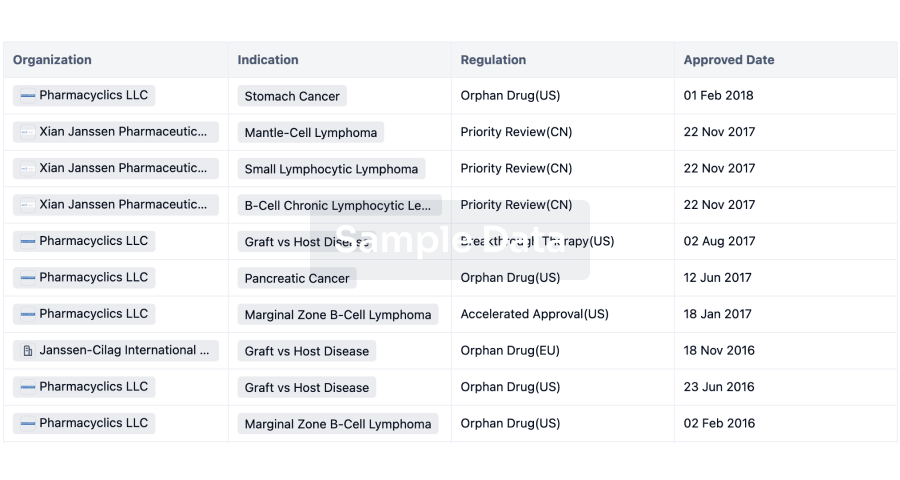
100 Patents (Medical) associated with Lamivudine/Zidovudine/Efavirenz
100 Deals associated with Lamivudine/Zidovudine/Efavirenz