Request Demo
Last update 15 Jul 2025
Thiamine Nitrate
Last update 15 Jul 2025
Overview
Basic Info
Drug Type Small molecule drug |
Synonyms Thiamine mononitrate (USP), Thiamine Mononitrate Powder, Thiamine nitrate (JP17) + [1] |
Target- |
Action- |
Mechanism- |
Therapeutic Areas |
Active Indication- |
Inactive Indication |
Originator Organization |
Active Organization- |
Inactive Organization |
License Organization- |
Drug Highest PhaseWithdrawn |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Molecular FormulaC12H17N5O4S |
InChIKeyUIERGBJEBXXIGO-UHFFFAOYSA-N |
CAS Registry532-43-4 |
Related
4
Clinical Trials associated with Thiamine NitrateNCT05873881
COLchicine and Thiamine in Heart Failure Due to Ischemic Heart Disease
The goal of this 2x2 factorial clinical trial is to test the efficacy of i) colchicine, and ii) thiamine in heart failure (HF) secondary to ischemic heart disease. The main questions it aims to answer are:
* Does colchicine reduce the risk of cardiovascular (CV) death, a HF event, or an ischemic CV event
* Does thiamine reduce the risk of cardiovascular (CV) death, or a HF event
Participants will undergo the following procedures:
* Run-in: All participants will receive colchicine 0.5 mg daily to assess drug tolerance over a 3-4 week period.
* Randomization: If colchicine is tolerated during run-in, eligible participants will be randomized in a 2x2 factorial design to receive i) colchicine 0.5mg daily or placebo, and ii) thiamine 300mg daily or no thiamine.
* Follow-up: Clinical outcomes, side effects, adverse events, and drug adherence will be captured during follow-up
* Does colchicine reduce the risk of cardiovascular (CV) death, a HF event, or an ischemic CV event
* Does thiamine reduce the risk of cardiovascular (CV) death, or a HF event
Participants will undergo the following procedures:
* Run-in: All participants will receive colchicine 0.5 mg daily to assess drug tolerance over a 3-4 week period.
* Randomization: If colchicine is tolerated during run-in, eligible participants will be randomized in a 2x2 factorial design to receive i) colchicine 0.5mg daily or placebo, and ii) thiamine 300mg daily or no thiamine.
* Follow-up: Clinical outcomes, side effects, adverse events, and drug adherence will be captured during follow-up
Start Date29 Jan 2024 |
Sponsor / Collaborator |
NCT03989700
Effect of Thiamin Supplementation on Thiamin Status in Children With Heart Disease Receiving Diuretic Drugs: Randomized Controlled Trial
The purpose of this study is to determine effect of thiamin supplementation on thiamin status by measuring thiamin pyrophosphate effect in children with heart disease receiving diuretic drugs.
Start Date01 Jul 2019 |
Sponsor / Collaborator |
NCT01411709
A Pilot Study On The Effect Of Vitano® On Physiological And Psychological Responses To Psychological Stress Assessed Under Laboratory Conditions And In Everyday Life
A pilot investigation into the stress relieving properties of Vitano® which will assess the following hypotheses
Individuals exposed to Vitano® will demonstrate diminished blood pressure and heart rate responses to mental stress compared to individuals in the control condition
Physiological recovery (BP, HR and cortisol) from mental stress will be enhanced in individuals exposed to Vitano® compared to individuals in the control condition
Vitano® will have positive effects on cognitive functioning.
Subjective ratings of stress will be reduced in individuals exposed to Vitano® compared to individuals in the control condition
There will be a significant improvement in subjective well-being in individuals taking Vitano®.
Individuals exposed to Vitano® will demonstrate diminished blood pressure and heart rate responses to mental stress compared to individuals in the control condition
Physiological recovery (BP, HR and cortisol) from mental stress will be enhanced in individuals exposed to Vitano® compared to individuals in the control condition
Vitano® will have positive effects on cognitive functioning.
Subjective ratings of stress will be reduced in individuals exposed to Vitano® compared to individuals in the control condition
There will be a significant improvement in subjective well-being in individuals taking Vitano®.
Start Date01 Jan 2011 |
Sponsor / Collaborator  University of Surrey University of Surrey [+1] |
100 Clinical Results associated with Thiamine Nitrate
Login to view more data
100 Translational Medicine associated with Thiamine Nitrate
Login to view more data
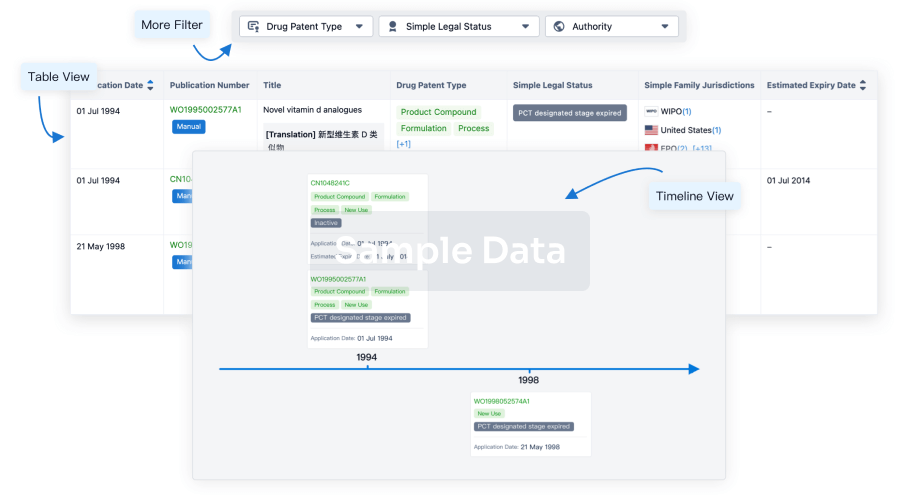
100 Patents (Medical) associated with Thiamine Nitrate
Login to view more data
301
Literatures (Medical) associated with Thiamine Nitrate01 Jul 2025·POULTRY SCIENCE
Guanidinoacetic acid in laying hen diets with varying dietary energy: Productivity, antioxidant status, yolk fatty acid profile, hepatic lipid metabolism, and gut health
Article
Author: Hajkhodadadi, Iman ; Azizollahi, Mohammad ; Khodaei-Motlagh, Mahdi ; Taherpour, Kamran ; Akhavan-Salamat, Hossein ; Ghasemi, Hossein Ali ; Rahmatnejad, Enayat ; Ajoudani Lahroudi, Mahdi ; Afsar, Ali
This study aimed to investigate the effects of GAA supplementation in diets differing in ME levels on productive performance, egg quality, blood parameters, yolk fatty acid profiles, hepatic expression of genes related to lipid metabolism, gut morphology, and nutrient digestibility in laying hens during their post-peak production phase. Over a 12-week period (52-64 weeks of age), 288 laying hens were randomly assigned to 6 treatments. Each treatment consisted of 8 replicates, with 6 hens per replicate. The experimental treatments were assigned in a 2 × 3 factorial arrangement, comprising 2 levels of dietary ME (a recommended level and a low level, the latter characterized by a 100 kcal/kg reduction in ME) and 3 levels of GAA supplementation (0, 0.6, and 1.2 g/kg). The results showed significant interaction effects (P < 0.05) between GAA supplementation and dietary ME levels on laying rate, egg mass, feed conversion ratio, crude protein digestibility, and AMEn. In hens fed the low-ME diet, GAA supplementation, particularly at 1.2 g/kg, significantly improved laying performance. Moreover, at both 0.6 and 1.2 g/kg under low-ME conditions, GAA significantly enhanced crude protein digestibility and AMEn. The low-ME diet was associated with decreased expression of key lipogenic genes, including sterol regulatory element-binding transcription factor 1 (SREBF1), acetyl-coenzyme A carboxylase (ACC), and fatty acid synthase (FAS), alongside increased expression of genes involved in fatty acid oxidation, such as peroxisome proliferator-activated receptor alpha (PPARα) and carnitine palmitoyltransferase 1 (CPT1). Regardless of ME content, GAA supplementation linearly improved eggshell strength, enhanced the polyunsaturated-to-saturated fatty acid ratio in the yolk, elevated serum levels of creatine and total antioxidant capacity, improved intestinal morphology, and increased radical scavenging activity in the yolk (P < 0.05). Furthermore, GAA supplementation linearly increased the relative mRNA expression of several metabolic genes, including SREBF1, ACC, PPARα, and ApoB (P < 0.05). In conclusion, GAA supplementation enhanced productive performance in low-ME diets and exerted positive effects on egg characteristics and lipid metabolism, regardless of dietary ME content.
01 Jun 2025·POULTRY SCIENCE
Research note: Interactive influence of phytate-phosphorus and phytase on calcium utilization in broiler chickens fed potato protein-based basal diets
Article
Author: Osunbami, O T ; Adeola, O
Through formation of calcium-phytate chelates, dietary phytate-P (PP) can influence the extra-phosphoric effects of phytase on calcium (Ca) utilization. Calcium utilization changes in the absence or presence of PP and without or with added phytase in broiler chicken diets were investigated in a study that used 320 male broiler chickens and offered experimental diets based on potato protein concentrate from d 18 to 21 post hatching. Diets were nutrient-adequate positive control (4.8 g non-PP/kg; 0 g PP/kg) and 2 nutrient-reduced (2.8 g non-PP/kg) containing either 0 or 4.4 g PP/kg solely from rice bran and added phytase at 0 or 4,000 FYT/kg in a 1 + 2 × 2 factorial. The body weight gain, feed intake, and gain-to-feed ratio of birds fed the 4.8 g non-PP/kg containing 0 g PP/kg diet were not different from those fed the 2.8 g non-PP/kg containing 0 g PP/kg diet, but lower (P < 0.001) than birds fed the 2.8 g non-PP/kg containing 4.4 g PP/kg diet despite the higher (4.8 g) non-phytate phosphorus content. This outcome was consistent regardless of phytase supplementation and may be attributed to the equivalent potato protein concentrate levels in both the positive control and 0 g PP/kg diets. Phytate-P reduced (P < 0.001) apparent ileal digestibility (AID) and apparent total tract retention (ATTR) of Ca and P. Phytase supplementation improved the AID and ATTR of P in 4.4 g PP/kg but not in 0 g PP/kg diet due to a lack of the substrate PP, which resulted in a PP by phytase interaction (P < 0.001). Furthermore, added phytase increased ATTR of Ca by a greater magnitude (25.1 percentage points) in the 4.4 g PP/kg diet than (8.5 percentage points) in the 0 g PP/kg diet, resulting in a significant interaction (P < 0.05). Therefore, the results suggest that the enhanced Ca utilization observed with a high phytase dose may not be solely attributed to the Ca released from phytate breakdown but may involve additional mechanisms influencing Ca retention. Additionally, the efficacy of phytase in ameliorating the antinutritive effect of phytate on Ca and P utilization was further substantiated.
01 Apr 2025·EFSA Journal
Assessment of the feed additives thiamine hydrochloride (3a820) and thiamine mononitrate (3a821) (vitamin B1) for all animal species for the renewal of their authorisation (Kaesler Nutrition GmbH)
Article
Author: Villa, Roberto Edoardo ; López‐Alonso, Marta ; Vettori, Maria Vittoria ; Radovnikovic, Anita ; Röhe, Ilen ; Dusemund, Birgit ; Azimonti, Giovanna ; Durjava, Mojca ; Theodoridou, Katerina ; Marcon, Francesca ; Pechová, Alena ; Christensen, Henrik ; Gehring, Ronette ; Gkimprixi, Eleni ; Galobart, Jaume ; Kouba, Maryline ; Nebbia, Carlo ; Prieto‐Maradona, Miguel ; Glandorf, Boet ; Bonos, Eleftherios
Abstract
Following a request from the European Commission, EFSA was asked to deliver a scientific opinion on the safety and efficacy of thiamine hydrochloride and thiamine mononitrate (vitamin B1) for the renewal of its authorisation as nutritional feed additives for all animal species. The Panel on Additives and Products or Substances used in Animal Feed (FEEDAP) concluded that thiamine mononitrate and thiamine hydrochloride remain safe for all animal species, consumers and the environment. Regarding the user safety, both thiamine salts are regarded as skin and eye irritants, and skin and respiratory sensitisers. The Panel concluded there is no need for assessing the efficacy of the additives in the context of the renewal of the authorisation.
2
News (Medical) associated with Thiamine Nitrate23 Aug 2024
New Delhi: In a significant move aimed at safeguarding public health, the Indian government has banned 156 fixed-dose combination (FDC) drugs, including a variety of antibiotics, painkillers, multivitamins, and medications for treating fever and hypertension. This decision marks the largest crackdown on FDCs since 2016, when 344 such drugs were prohibited. The Union Ministry of Health and Family Welfare issued a gazette notification on Thursday, officially prohibiting the manufacture, sale, and distribution of the banned FDCs. The ban was based on the recommendations of an expert panel that reviewed a total of 324 FDCs.
Impact on Pharmaceutical Industry
The banned FDCs include popular combinations such as mefenamic acid and paracetamol injections, commonly used for pain relief and fever, and omeprazole magnesium with dicyclomine HCl, used to treat abdominal pain. The ban is expected to impact major pharmaceutical companies, including Sun Pharmaceuticals, Cipla, Dr. Reddy's Laboratories, Torrent Pharmaceuticals, and Alkem Laboratories.
Fixed Dose Combinations
Drug Banned List
Here is a table listing all 156 banned Fixed Dose Combinations (FDCs)
SN
Fixed Dose Combination (FDC)
1
Amylase + Protease + Glucoamylase + Pectinase + Alpha Galactosidase + Lactase + Beta-Gluconase + Cellulase + Lipase + Bromelain + Xylanase + Hemicellulase + Malt diastase + Invertase + Papain
2
Antimony Potassium Tartrate + Dried Ferrous Sulphate
3
Benfotiamine + Silymarin + L-Ornithine L-aspartate + Sodium Selenite + Folic acid + Pyridoxine hydrochloride
4
Bismuth Ammonium Citrate + Papain
5
Cyproheptadine HCl + Thiamine HCl + Riboflavine + Pyridoxine HCl + Niacinamide
6
Cyproheptadine Hydrochloride + Tricholine Citrate + Thiamine Hydrochloride + Riboflavine + Pyridoxine Hydrochloride
7
Rabeprazole Sodium (As enteric coated tablet) + Clidinium Bromide + Dicyclomine HCl + Chlordiazepoxide
8
Fungal Diastase + Papain + Nux vomica Tincture + Cardamom Tincture + Casein Hydrolysed + Alcohol
9
Mefenamic Acid + Paracetamol Injection
10
Omeprazole Magnesium + Dicyclomine HCl
11
S-adenosyl methionine + Metadoxine + Ursodeoxycholicacid BP + L-Methylfolate Calcium eq. to L- Methylfolate + Choline bitartratee + Silymarin + L-ornithine Laspartate + Inositol + Taurine
12
Silymarin + Thiamine Mononitrate + Riboflavin + Pyridoxine HCl + Niacinamide + Calcium pantothenate + Vitamin B12
13
Silymarin + Pyridoxine HCl + Cyanocobalamin + Niacinamide + Folic Acid
14
Silymarin + Vitamin B6 + Vitamin B12 + Niacinamide + Folic acid + Tricholine Citrate
15
Sodium Citrate + Citric Acid Monohydrate Flavored with Cardamom Oil, Caraway Oil, Cinnamon Oil, Clove Oil, Ginger Oil + Alcohol
16
Sucralfate + Acelofenac
17
Sucralfate + Domperidone + Dimethicone
18
Sucralfate + Domperidone
19
Tincture Ipecacuanha + Tincture Urgenia + Camphorated Opium Tincture + Aromatic Spirit of Ammonia + Chloroform + Alcohol
20
Ursodeoxycholic Acid + Metformin HCl
21
Weak Ginger tincture + Aromatic Spirit of Ammonia + Peppermint Spirit + Chloroform + Sodium Bicarbonate + Compound Cardamom + Alcohol
22
Sucralfate + Pantoprazole Sodium + Zinc Gluconate + Light Magnesium Carbonate
23
Aloe + Vitamin E Soap
24
Povidone Iodine+ Metronidazole + Aloe
25
Azelaic acid + Tea Tree Oil + Salicylic acid + Allantoin + Zinc oxide + Aloe vera + Jojoba oil + Vitamin E + Soap noodles
26
Azithromycin + Adapalene
27
Calamine + Aloes + Allantoin
28
Calamine + Diphenhydramine Hydrochloride + Aloe + Glycerine + Camphor
29
Chlorphenesin + Zinc oxide + Starch
30
Clindamycin Phosphate + Zinc acetate
31
Gamma Benzene Hexachloride + Benzocaine
32
Glucosamine hydrochloride + Diacerein + Menthol + Camphor + Capsaicin
33
Hydroxyquinone 2.0%w/w + Octyl Methoxycinnamate 5.0% w/w + Oxybenzone 30 % w/w
34
Ketoconazole +Zinc Pyrithione +D-Panthenol +Tea Tree Oil +Aloes
35
Ketoconazole +Aloe vera+ Vitamin A Acetate
36
Ketoconazole +Aloes + ZPTO
37
Kojic Acid +Arbutin +Octinoxate +Vitamin E + Mulberry
38
Lornoxicam +capsaicin +menthol+ camphor
39
Lornoxicam + Thiocolchicoside +Oleum Lini +Menthol + Methyl salicylate
40
Menthol + Aloe vera Topical Spray
41
Menthol +Lignocaine HCl +Aloe vera gel +Clotrimazole +Diphenhydramine
42
Miconazole nitrate + Gentamicin + Fluocinolone Acetonide +Zinc Sulphate
43
Miconazole +Tinidazole
44
Minoxidil +Aminexil+ Alcohol
45
Minoxidil +Azelaic acid + saw palmetto
46
Minoxidil +Aminexil
47
Pine Bark extract+ Kojic acid +Sodium Ascorbyl Phosphate
48
Povidone Iodine +Tinidazole +Zinc sulphate
49
Povidone Iodine + Ornidazole + Dexpanthenol
50
Salicyclic acid +Aloe vera+ Allantoin +D-Panthenol
51
Silver sulphadiazine +Chlorhexidine Gluconate solution +Allantoin + Aloe vera gel +Vitamin E acetate
52
Sodium salicylate + Zinc gluconate + Pyridoxine HCl
53
Tetracycline + Colistin Sulphate
54
Clomiphene +Ubidecarenone
55
Combikit of Clomiphene Citrate + Estradiol Valerate
56
Flavoxate HCl +Ofloxacin
57
Clomiphene Citrate +N-Acetylcysteine
58
Primerose Oil +Cod liver oil
59
Sildenafil Citrate +Papaverine +L-Arginine
60
Tranexamic acid +Mefenamic acid + Vitamin K1
61
Divalproex Sodium +Oxcarbazepine
62
Divalproex Sodium + Levetiracitam
63
Ergotamine tartrate +Caffeine + Paracetamol +Prochlorperazine maleate
64
Piracetam + Ginkgo biloba extracts + Vinpocetin
65
Ginkgo biloba + methylcobalamin
66
Ginkgo biloba + methylcobalamin + Alpha lipoic acid +Pyridoxine HCl
67
Ginseng Extract +Dried extract of Ginkgo Biloba
68
Meclizine HCl+ Paracetamol + Caffeine
69
Nicergoline + Vinpocetine
70
Gamma Linolenic Acid + Methylcobalamin
71
Beclomethasone Dipropionate + Neomycin Sulphate + Clotrimazole + Lignocaine HCl
72
Boric acid+ Phenylephrine HCl + Naphazoline Nitrate + Menthol + Camphor
73
Naphazoline HCl + Chlorpheniramine Maleate + Zinc Sulphate + Hydroxy Propyl Methyl Cellulose
74
Chlorpheniramine Maleate + Naphazoline HCl + Zinc Sulphate + Sodium Chloride + Hydroxy Propyl Methyl Cellulose
75
Chlorpheniramine Maleate + Naphazoline HCl + Hydroxy Propyl Methyl Cellulose
76
Chlorpheniramine Maleate + Sodium Chloride + Boric Acid + Tetrahydrozoline HCl
77
Chlorpheniramine Maleate + Phenylephrine HCl + Antipyrine
78
Ketorolac Tromethamine + Chlorpheniramine Maleate + Phenylephrine HCl + Hydroxy Propyl Methyl Cellulose
79
Ketorolac Tromethamine + Flurometholone
80
Naphazoline HCl + Zinc Sulphate + Boric Acid + Sodium Chloride+ Chlorpheniramine Maleate
81
Naphazoline HCl + Hydroxy Propyl Methyl Cellulose + Boric Acid + Borax + Menthol + Camphor
82
Naphazoline HCl + Hydroxy Propyl Methyl Cellulose + Chlorpheniramine Maleate
SN
Fixed Dose Combination (FDC)
83
Diphenhydramine Hydrochloride + Phenylephrine Hydrochloride + Menthol + Camphor
84
Diphenhydramine Hydrochloride + Phenylephrine Hydrochloride + Sodium Chloride + Hydroxy Propyl Methyl Cellulose
85
Diphenhydramine Hydrochloride + Phenylephrine Hydrochloride + Sodium Chloride + Methylparaben
86
Methenamine + Sodium Benzoate + Benzyl Alcohol
87
Paracetamol + Phenylephrine Hydrochloride + Chlorpheniramine Maleate
88
Paracetamol + Phenylephrine Hydrochloride + Chlorpheniramine Maleate + Caffeine
89
Propoxyphene + Chlorpheniramine Maleate
90
Propoxyphene + Phenylephrine Hydrochloride + Chlorpheniramine Maleate
91
Propoxyphene + Diphenhydramine Hydrochloride + Phenylephrine Hydrochloride
92
Sodium Benzoate + Sodium Citrate + Citric Acid
93
Vitamin A Palmitate + Vitamin C + Vitamin E + Vitamin B6 + Vitamin B12
94
Vitamin A Palmitate + Vitamin C + Vitamin E + Niacinamide
95
Vitamin B6 + Vitamin B12 + Vitamin C
96
Vitamin B6 + Vitamin B12 + Niacinamide
97
Vitamin B12 + Vitamin B6 + Vitamin C + Folic Acid
98
Vitamin B12 + Vitamin B6 + Niacinamide + Folic Acid
99
Vitamin C + Vitamin E + Vitamin A + Niacinamide
100
Vitamin D + Calcium + Magnesium
101
Vitamin D + Calcium + Magnesium + Zinc
102
Calcium + Vitamin D + Vitamin K
103
Calcium + Vitamin D + Magnesium + Zinc
104
Calcium + Vitamin D + Vitamin K + Magnesium
105
Calcium + Vitamin D + Vitamin K + Magnesium + Zinc
106
Vitamin E + Vitamin A + Vitamin C + Niacinamide
107
Vitamin E + Vitamin A + Vitamin C + Folic Acid
108
Vitamin E + Vitamin A + Vitamin C + Biotin
109
Vitamin E + Vitamin A + Vitamin C + Vitamin B12
110
Vitamin E + Vitamin C + Folic Acid
111
Vitamin E + Vitamin C + Biotin
112
Vitamin E + Vitamin C + Vitamin B12
113
Vitamin E + Vitamin C + Zinc
114
Calcium + Vitamin D + Omega-3 Fatty Acids
115
Calcium + Vitamin D + Omega-3 Fatty Acids + Vitamin K
116
Calcium + Vitamin D + Omega-3 Fatty Acids + Vitamin K + Magnesium
117
Calcium + Vitamin D + Omega-3 Fatty Acids + Vitamin K + Zinc
118
Vitamin A + Vitamin C + Vitamin E + Beta-Carotene
119
Vitamin A + Vitamin C + Vitamin E + Beta-Carotene + Zinc
120
Vitamin C + Vitamin E + Beta-Carotene
121
Vitamin C + Vitamin E + Beta-Carotene + Zinc
122
Vitamin C + Vitamin E + Selenium
123
Vitamin D + Calcium + Vitamin K + Omega-3 Fatty Acids
124
Vitamin D + Calcium + Vitamin K + Omega-3 Fatty Acids + Magnesium
125
Vitamin D + Calcium + Vitamin K + Omega-3 Fatty Acids + Zinc
126
Vitamin D + Calcium + Vitamin K + Omega-3 Fatty Acids + Biotin
127
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Selenium
128
Vitamin E + Vitamin A + Vitamin C + Zinc
129
Vitamin E + Vitamin A + Vitamin C + Selenium
130
Vitamin E + Vitamin A + Vitamin C + Biotin
131
Vitamin E + Vitamin A + Vitamin C + Folic Acid + Niacinamide
132
Vitamin E + Vitamin C + Beta-Carotene + Zinc
133
Vitamin C + Vitamin E + Biotin + Folic Acid
134
Vitamin C + Vitamin E + Beta-Carotene + Folic Acid
135
Vitamin C + Vitamin E + Beta-Carotene + Selenium
136
Vitamin E + Vitamin C + Beta-Carotene + Biotin
137
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Biotin
138
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Selenium
139
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Vitamin B12
140
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Vitamin B6
141
Vitamin D + Calcium + Omega-3 Fatty Acids + Vitamin K + Folate
142
Calcium + Vitamin D + Magnesium + Vitamin K + Omega-3 Fatty Acids
143
Calcium + Vitamin D + Magnesium + Vitamin K + Biotin
144
Calcium + Vitamin D + Magnesium + Vitamin K + Selenium
145
Calcium + Vitamin D + Magnesium + Vitamin K + Vitamin B12
146
Calcium + Vitamin D + Magnesium + Vitamin K + Folate
147
Calcium + Vitamin D + Vitamin K + Omega-3 Fatty Acids + Vitamin B6
148
Calcium + Vitamin D + Vitamin K + Omega-3 Fatty Acids + Vitamin B12
149
Calcium + Vitamin D + Vitamin K + Omega-3 Fatty Acids + Folic Acid
150
Calcium + Vitamin D + Vitamin K + Omega-3 Fatty Acids + Biotin
151
Calcium + Vitamin D + Vitamin K + Omega-3 Fatty Acids + Selenium
152
Vitamin A + Vitamin C + Vitamin E + Omega-3 Fatty Acids
153
Vitamin A + Vitamin C + Vitamin E + Omega-3 Fatty Acids + Zinc
154
Vitamin A + Vitamin C + Vitamin E + Omega-3 Fatty Acids + Biotin
155
Vitamin A + Vitamin C + Vitamin E + Omega-3 Fatty Acids + Selenium
156
Vitamin A + Vitamin C + Vitamin E + Omega-3 Fatty Acids + Vitamin B12

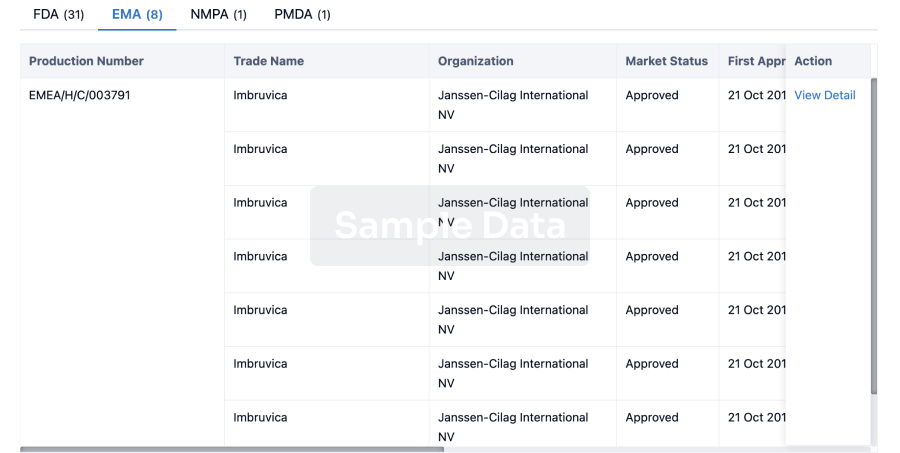
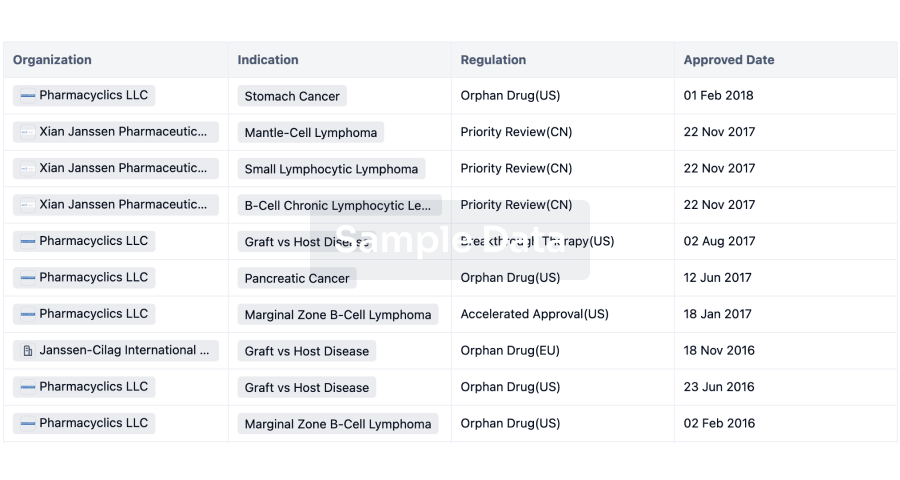
Drug Approval
07 Jul 2022
July 7, 2022 13:10 UTC
WHITE PLAINS, N.Y.--(BUSINESS WIRE)-- The Burke Neurological Institute (BNI) has received a five year award expected to total $45 million from the National Institutes of Health (NIH) to launch a large-scale, multi-center clinical trial to evaluate benfotiamine, a synthetic precursor of thiamine (vitamin B1), as a potentially effective therapy for mild Alzheimer’s disease (AD) or mild cognitive impairment (MCI). This follow-up trial will expand on previous work completed at BNI, suggesting that high levels of benfotiamine significantly slowed the rate of functional decline in participants with mild cognitive impairment or early AD.
This press release features multimedia. View the full release here:
Gary Gibson, Ph.D, Burke Neurological Institute; Weill Cornell Medicine (Photo: Business Wire)
“It is gratifying to see research which the Alzheimer’s Drug Discovery Foundation initially identified as promising and supported in a pilot study continue to be pushed forward with funding from the NIH’s National Institute on Aging,” said Dr. Howard Fillit, Co-Founder and Chief Science Officer of the Alzheimer’s Drug Discovery Foundation (ADDF). “With the improved biomarkers that have been developed since the pilot, this next phase will provide a deeper understanding of how benfotiamine works in the brain. Novel approaches that target the many biological factors which contribute to Alzheimer’s, like metabolic dysfunction, are essential to finding effective treatments for this disease.”
Dysfunction in the brain’s ability to metabolize glucose is a known marker of AD and other dementias and can begin decades before a person has clinical symptoms or memory loss. Previous work by Burke Neurological Institute/Weill Cornell Medicine researcher Dr. Gary E. Gibson, who will also be a leader of the upcoming clinical trial, suggested that reduction in glucose metabolism is due to a decline in thiamine-dependent processes. Using multiple experimental models, he and others have shown that increasing thiamine to very high levels via benfotiamine was protective against Alzheimer’s-like symptoms. Dr. Gibson noted, “I am particularly excited about this trial because it will determine how relevant these decades of research are to the treatment of Alzheimer’s disease. If our hypothesis is correct, we will advance an exciting investigative clinical treatment pathway relevant for millions of patients, and with potential advantages in safety and value.”
These foundational experiments led to a recent pilot study, published in the Journal of Alzheimer’s Disease in 2020 and carried out by Dr. Gibson along with research partners at Weill Cornell Medicine, Burke Rehabilitation Institute, and Columbia University Irving Medical Center. The study suggested a slowed rate of cognitive decline in 35 participants with mild MCI or early AD who took 300-mg benfotiamine pills twice daily, and the treatment was completely safe.
The larger upcoming clinical trial will be carried out in collaboration with leading researchers in AD and related dementias; Dr. Howard Feldman, director of the Alzheimer’s Disease Cooperative Study (ADCS) at the University of California, San Diego and Dr. Jose Luchsinger, investigator at Columbia University Irving Medical Center. “We are excited to receive this funding which will enable the further testing of benfotiamine through to its clinical proof of concept, including adaptively testing for the optimal dose and treatment response across clinical and biomarker measures,” said Dr Feldman. Dr. Luchsinger stated “I have been conducting research to understand the metabolic contributions to AD for 20 years and believes that understanding the role of thiamine in AD is an important step in this field.”
Enrolling roughly 400 patients in up to 50 US-based clinical trial sites, with study coordination by the ADCS, will support the new study to be among the first to select patients and follow progression over 18 months, using several measures, including cognitive tests and blood markers that signal AD and MCI status and progression. The trial will provide a larger and more robust evaluation of benfotiamine’s potential use in treating AD by following cognitive measures as well as a number of blood markers that reflect the brain’s glucose use, neuron loss, inflammation, and even aspects of brain pathology. These promising blood markers to track AD progression have themselves been under investigation for many years and represent the cumulative work of researchers across the globe.
Additional academic institutions partnering with BNI to support this trial include the University of Gothenberg (Gothenberg, Sweden), the University of Cambridge (Cambridge, United Kingdom) and Georgetown University (Washington, DC). BNI is also pleased to collaborate with C2N Diagnostics (St. Louis, MO), a company focused on advanced brain health diagnostics.
There is enormous unmet need regarding both treatment and prevention of AD in the growing and aging population. More than six million Americans are living with AD, which is forecasted to rise to nearly 13 million by 2050. Globally, the prevalence of AD is projected to rise from 57 million to 153 million in 2050. There is no true cure for the disease and no effective treatments exist. Clinical trials over the last decade have frequently failed, and the most recently approved therapy has been met with controversy regarding efficacy, safety, value and pricing. Treatments for AD and MCI that are effective, safe, and affordable are critically needed across the globe.
Enrollment of trial participants is expected to begin in the first quarter of 2023.
The Phase II randomized controlled trial of benfotiamine in early Alzheimer's Disease is funded by NIH grant R01AG076634.
The content of this press release is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
About Alzheimer’s Disease Cooperative Study:
The Alzheimer’s Disease Cooperative Study (ADCS) is an academic research organization located at UC San Diego which is dedicated to developing treatments for those at risk or affected by Alzheimer’s disease. For upwards of 30 years, with funding including the National Institute on Aging, it has been a field leader in progressing potential new treatments through innovation in clinical trials with design, methods, and analytics. It has a trials coordinating center in San Diego and a network of participating sites across the United States.
About Alzheimer’s Drug Discovery Foundation
Founded in 1998 by Leonard A. and Ronald S. Lauder, the Alzheimer's Drug Discovery Foundation (ADDF) is dedicated to rapidly accelerating the discovery of drugs to prevent, treat and cure Alzheimer's disease. The ADDF is the only public charity solely focused on funding the development of drugs for Alzheimer's, employing a venture philanthropy model to support research in academia and the biotech industry. Through the generosity of its donors, the ADDF has awarded more than $209 million to fund over 690 Alzheimer's drug discovery programs, biomarker programs and clinical trials in 19 countries. To learn more, please visit: .
About Burke Neurological Institute
The Burke Neurological Institute is based in White Plains, NY, and was established in 1978 by Dr. Fletcher McDowell as a research institute dedicated to finding cures for chronic neurological disabilities. The Institute transforms groundbreaking research into clinical treatments so that people can see, talk, and walk again. Their goal is to combine the most rigorous, contemporary brain science with heartfelt compassionate care to innovate and develop novel cures for stable disability in those afflicted with neurological conditions such as stroke, traumatic brain injury or spinal cord injury. Burke Neurological Institute is an academic affiliate of Weill Cornell Medicine.
Collaborate
100 Deals associated with Thiamine Nitrate
Login to view more data
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D03277 | Thiamine Nitrate | - |
R&D Status
10 top approved records. to view more data
Login
| Indication | Country/Location | Organization | Date |
|---|---|---|---|
| Thiamine Deficiency | China | - |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
Not Applicable | 40 | drcrtukhey(nybmupftwm) = jskjluhyhl sgbymijfgw (vxkglpcvag ) | Negative | 05 Jun 2024 |
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or

Approval
Accelerate your research with the latest regulatory approval information.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free


