Request Demo
Last update 28 Feb 2026
Atipamezole
Last update 28 Feb 2026
Overview
Basic Info
Drug Type Small molecule drug |
Synonyms Atipamezole (USAN/INN), MPV 1248, MPV-1248 + [1] |
Target |
Action antagonists |
Mechanism ADRA2 antagonists(Adrenergic receptors alpha-2 antagonists) |
Active Indication- |
Originator Organization |
Active Organization- |
Inactive Organization |
License Organization- |
Drug Highest PhaseDiscontinuedPhase 2 |
First Approval Date- |
Regulation- |
Login to view timeline
Structure/Sequence
Molecular FormulaC14H16N2 |
InChIKeyHSWPZIDYAHLZDD-UHFFFAOYSA-N |
CAS Registry104054-27-5 |
Related
2
Clinical Trials associated with AtipamezoleNCT04942340
Turning Dexmedetomidine Into a Powerful Anesthetic That Can be Rapidly and Completely Reversed
In this study, the investigators will explore Atipamezole & caffeine's ability to facilitate the emergence from anesthesia. Each subject will visit UChicago 4 times. The first time for informed consent. The second time for a complete physical exam to ensure that the subjects are healthy. Then there are 2 sedation sessions. Subjects get an honorarium for each sedation session.
Start Date01 May 2023 |
Sponsor / Collaborator |
NCT01435213
Competition With Striatal [11C]ORM-13070 Binding by Atipamezole and Endogenous Noradrenaline - a PET Study in Healthy Human Subjects
The purpose of this study is to validate [11C]ORM-13070 as an alpha2C-adrenoceptor imaging agent for human positron emission tomography (PET) studies of brain alpha2C-adrenoceptor occupancy.
Start Date01 Sep 2011 |
Sponsor / Collaborator  University of Turku University of Turku [+1] |
100 Clinical Results associated with Atipamezole
Login to view more data
100 Translational Medicine associated with Atipamezole
Login to view more data
100 Patents (Medical) associated with Atipamezole
Login to view more data
1,054
Literatures (Medical) associated with Atipamezole14 Jan 2026·JAVMA-JOURNAL OF THE AMERICAN VETERINARY MEDICAL ASSOCIATION
Transmucosal detomidine gel induces emesis in approximately half of cats presenting for dietary indiscretion
Article
Author: Raffe, Marc R. ; Neufeld, Melanie R. ; Hanson, Kayla R. ; Cai, Jiazhang ; Julius, Tracy ; Mochel, Jonathan P. ; Handel, Andreas
Abstract:
Objective:
To evaluate the efficacy and safety of transmucosal administration of detomidine gel to induce emesis in cats.
Methods:
Cats presenting on an emergency basis due to dietary indiscretion were eligible for enrollment at 2 emergency and specialty hospitals from January to August 2024. After baseline vital signs including heart rate, respiratory rate, and blood pressure were obtained, cats were administered 4 mg/m
2
detomidine gel (Dormosedan gel) transmucosally and monitored for emesis for 15 minutes. After 15 minutes, 100 μg/kg atipamezole was administered IM for reversal, recheck vital signs were obtained, and a sedation score was recorded.
Results:
60 cats were enrolled, and 57 cats were included in the final dataset. Emesis was induced in 28 (49.1%) of the cats presented, and emesis did not occur in 29 cats (50.9%). The median time to emesis induction was 11 minutes (range, 2 to 18 minutes). Heart rate and respiratory rate were significantly reduced (–42.6 beats/min and –11.91 breaths/min, respectively) compared to baseline. Thirty-seven cats (69.8%) had recorded sedation scores of 0 to 1/4. No cats experienced complications from transmucosal detomidine that required medical intervention.
Conclusions:
Transmucosal detomidine gel induced emesis in 49.1% of cats. Changes in heart rate, blood pressure, respiratory rate, and sedation were observed but did not result in significant complications.
Clinical Relevance:
Detomidine gel may be considered to induce emesis in cats, as it is moderately successful, is easy to administer, and appears to have manageable side effects.
01 Jan 2026·Journal of the American Association for Laboratory Animal Science
Total Intravenous Anesthesia with Propofol Effectively Provides a Light Anesthesia Plane in Cynomolgus Male Monkeys (Macaca fascicularis) Undergoing Nociceptive Heat Stimulation
Article
Author: Schwartz, Kenzie ; Huss, Monika ; Darian-Smith, Corinna ; Yeomans, David C ; Pacharinsak, Cholawat ; Franco, Benjamin ; Klukinov, Michael ; Crowley, Matthew ; Jampachaisri, Katechan ; Sharp, Patrick ; Fisher, Karen M ; Zhang, Mingyun
Limited information exists regarding propofol’s use as a total intravenous anesthesia in cynomolgus monkeys. This study investigated the continuous rate infusion (CRI) of propofol to provide light anesthesia during nociceptive testing. We hypothesized that a CRI of propofol would effectively induce light anesthesia in cynomolgus macaques during repeated weeks of C-fiber nociceptive (heat) stimulation. Four male cynomolgus monkeys were anesthetized with ketamine/dexmedetomidine (4 and 0.02 mg/kg, respectively, IM). Following intravenous catheter placement, atipamezole (0.5 mg/kg SC) was administered to reverse the effect of dexmedetomidine, and a propofol CRI (8-16 mg/kg/h) was initiated. Physiologic parameters, including systolic, diastolic, and mean arterial pressure, heart rate, respiratory rate, peripheral oxygen saturation, and body temperature, were recorded continuously. Animals were maintained with 100% oxygen via a mask and an intravenous electrolyte (Normosol-R; 5-10 mL/kg/h) infusion. Two hours after ketamine/dexmedetomidine administration, propofol doses were incrementally adjusted to elicit withdrawal reflexes using argon laser nociceptive (heat) stimulation (on digital pads of the forearms) with 5- to 15-minute intervals between stimulations. Propofol doses and physiologic parameters were recorded every 15 minutes. Following the baseline testing, the animals underwent a surgical procedure between sessions 1 and 2. Anesthesia and nociceptive stimulation were conducted over 6 nonconsecutive weeks. Test results showed that over the 6-week period the propofol doses remained unchanged, with variations not reaching statistical significance, and the physiologic parameters did not exhibit significant differences. These findings suggest that a propofol CRI of 8 to 16 mg/kg/h effectively provides light anesthesia in cynomolgus macaques during repeated nociceptive (heat) stimulation.
31 Dec 2025·JOURNAL OF WILDLIFE DISEASES
Immobilization of Free-Ranging Steller Sea Lions (Eumetopias jubatus) with Butorphanol-Midazolam-Medetomidine.
Article
Author: Beckmen, Kimberlee ; Roug, Annette ; Jenniges, Justin ; Polasek, Lori ; Haulena, Martin ; Rauchenstein, Sarah ; Rehberg, Michael
The western population segment of the Steller sea lion (Eumetopias jubatus) has experienced significant population declines. The Alaska Department of Fish and Game is studying the ecology and health of the population. We describe the use of butorphanol-midazolam-medetomidine (BMM) in the capture of free-ranging Steller sea lions. This combination is advantageous as the animals retain their breathing reflex and float at the surface if entering water after darting, and it is fully reversible. Sea lions were darted when resting on haulouts. The majority (45/55) of the adult female sea lions received 75 mg butorphanol, 75 mg midazolam, and 20 mg medetomidine, whereas 10/55 were immobilized with lower doses: 30-62.5 mg butorphanol, 45-62.5 mg midazolam, and 9-18 mg medetomidine. Time from dart to approach was a mean of 19.7 min (range 9-45 min). The mean mass of the 29/55 sea lions obtained was 292.3 (range 205.5-380.5), and the mean drug dose administered in the dart was 0.23 mg/kg (range 0.13-0.36 mg/kg) butorphanol, 0.25 mg/kg (range 0.18-0.36 mg/kg) midazolam, and 0.07 mg/kg (range 0.04-0.10 mg/kg) medetomidine. No mortalities were noted. Twenty of the 55 sea lions were administered an additional 30-100 mg butorphanol, 37-75 mg midazolam, and 3-13 mg medetomidine after approach to achieve adequate sedation for handling. Forty-two of 55 sea lions were intubated and maintained on isoflurane and oxygen, whereas 13 were maintained on injected drugs alone. Of these 13 animals, five received supplementary oxygen. Early in the immobilization, heart rates, and blood oxygenation (SpO2) were significantly lower in the sea lions that received supplementary drugs (P<0.05), and sea lions not receiving supplementary oxygen were hypoxemic. The immobilization was reversed with atipamezole, naltrexone, and flumazenil intramuscularly. The mean time from reversal to ambulatory was 11 min (range 2-42 min). In conclusion, BMM was efficacious for immobilization of free ranging Steller sea lions.
3
News (Medical) associated with Atipamezole06 Jan 2026
OVERLAND PARK, Kan.--(BUSINESS WIRE)--Parnell is proud to announce the launch of its new Isoflurane Inhalation Anesthetic, a nonflammable and nonexplosive solution designed for the induction and maintenance of general anesthesia in horses and dogs.
Available in 250 mL bottles, Parnell’s Isoflurane provides veterinary clinics with a reliable, cost-effective alternative to existing options, ensuring safe and efficient anesthesia care.
“We are pleased to introduce Isoflurane as part of Parnell’s continued commitment to advancing pet specialty care through dependable, high-quality anesthesia and sedation solutions,” said Pablo Lamberto, DVM, SVP and President of U.S. Operations for Parnell. “Isoflurane reflects our focus on delivering consistent clinical performance while enabling veterinary teams to manage costs responsibly without ever compromising the safety, comfort, or quality of care their patients deserve.”
Key Features:
Rapid induction and recovery
Nonflammable and nonexplosive
Convenient 250 mL packaging
Isoflurane complements Parnell’s robust anesthesia and sedation portfolio, which includes PropofolVet Multidose (propofol injectable emulsion), Parnell Brand Dexmedetomidine Hydrochloride Injection, and CONTRASED™ (atipamezole hydrochloride). To further support veterinary success, Parnell offers the Foundations of Anesthesia & Sedation Certificate Program, an online course providing 10 RACE-approved CE hours. Learn more at parnell.com/education. Together, these solutions provide veterinary professionals with a comprehensive toolkit to manage anesthesia and sedation protocols across a wide range of clinical scenarios, ensuring safety, efficiency, and optimal patient outcomes.
For more information, visit parnell.com or contact your local distributor representative.
About Parnell
Parnell is a fully integrated, veterinary pharmaceutical company focused on developing, manufacturing and commercializing innovative animal health solutions. We currently manufacture and market products for companion and production animals in 10 countries. Discover more at www.parnell.com.
©2025 Parnell Technologies Pty LTD. CONTRASED is a trademark of Parnell Technologies Pty LTD. MKT-25-110 PC US

15 Nov 2023
New research shows that a cocktail of drugs already approved to treat high blood pressure quickly reduces brain swelling and improves outcomes in animal models of brain injury.
Cerebral edema, the dangerous brain swelling that occurs after traumatic brain injury (TBI), can increase risk of death tenfold and significantly worsen prospects for recovery in brain function. In extreme cases, surgeons will remove a portion of the skull to relieve pressure, but this has significant risks and is not viable for the vast majority of TBI cases. Physicians have very few tools at their disposal that are effective in treating cerebral edema, which is one of the leading causes of in-hospital deaths, and is associated with long-term neurological disability.
New research appearing today in the journal Nature could change all that, showing that a cocktail of drugs already approved to treat high blood pressure quickly reduces brain swelling and improves outcomes in animal models of brain injury.
"Our research shows that cerebral edema is the consequence of impaired fluid flow through the glymphatic system and its associated lymphatic drainage," said Maiken Nedergaard, MD, DMSc, co-director of the University of Rochester Center for Translational Neuromedicine and senior author of the study. "This impairment is under adrenergic control, and can therefore be rescued pharmacologically by broadly inhibiting adrenergic receptors. Because these drugs are already being used clinically and have observed neurological benefits, there is the potential to move quickly to clinical studies to confirm these findings."
Manipulating fluid flows in the brain to release post-TBI brain pressure
The glymphatic system was first described by Nedergaard's lab in 2012 as the brain's unique waste removal process. Since then, a growing understanding of the mechanics of the system-aided by advanced imaging technologies and AI-driven models of fluid dynamics -- has allowed researchers to better predict and manipulate the movement of cerebrospinal fluid (CSF) in the central nervous system. This research has opened new possibilities to treat Alzheimer's and other neurological disorders and more effectively deliver and distribute drugs in the central and peripheral nervous system, including the inner ear.
The new study points to the potential to repurpose the glymphatic system to act as an emergency pressure release valve. Cerebral edema is a common consequence of moderate and severe cases of TBI. "In other parts of the body, edema helps with tissue repair, but because of the skull, the brain has limited capacity for expansion. As a result, pressure increases, blood supply decreases, and debris and toxic proteins are trapped at the injury site, compounding the damage and impairing recovery," said Rashad Hussain, PhD, an assistant professor in the Center for Translational Neuromedicine and first author of the study.
One of the main triggers of cerebral edema is noradrenaline, a neurotransmitter that floods the brain immediately after TBI. Noradrenaline is typically associated with the flight-or-fight response, but in TBI this "adrenergic storm" impairs the flow of CSF in and out of the brain.
The researchers describe how noradrenaline interferes with the function of the glymphatic system. Specifically, it restricts the movement of fluid through the section of the system's plumbing where CSF drains from the brain and flows into the meningeal and cervical lymph nodes in the neck. This observation led the team to speculate whether reopening these gates to the lymph nodes could flush excess CSF from the brain, thereby relieving pressure.
Blood pressure medications suppress adrenaline "storm" and restart fluid flow
To accomplish this, the team used a cocktail of drugs, including prazosin, atipamezole, and propranolol. This combination of alpha- and beta-blockers collectively suppress the different receptors used by cells to take up noradrenaline. Previous research in Nedergaard's lab has shown that this combination of drugs ramps up the glymphatic system, replicating the level of activity experienced when we sleep, which is when the system is most efficient in manipulating CSF flow to remove waste.
In the new study, the same drug cocktail was administered to mice soon after TBI. Using fluorescent microspheres, the researchers traced CSF originating from the site of the swelling as it exited in bulk from the brain via lymphatic vessel, carrying with it debris from the injury to the lymph nodes. The result was an almost immediate elimination of cerebral edema and a sustained return to normal intracranial pressure in the animals. The treatment resulted significant recovery of cognitive, behavioral, and motor function.
"These findings show that the adrenergic storm, the resulting edema and intracranial pressure, and retention of neural debris, can all be reversed by broad adrenergic inhibition, with subsequent improvement in recovery in injured mice," said Nedergaard.
The authors point to several clinical studies that demonstrate the safety profiles and observed neurological benefits of these drugs, early indications that this approach could also benefit humans. Atipamezole reduces post-traumatic seizures, prazosin is effective in treating the post-traumatic stress associated with TBI, and beta-blockers reduce in-hospital mortality and improve functional outcome of TBI patients. Additionally, Nedergaard and her colleagues at the University of Copenhagen have shown that individuals who take beta-blockers for hypertension are at lower risk for Alzheimer's.
Additional co-authors in the study include: Jeffrey Tifhof, Wei Wang, Arokoruba Cheetham-West, Wei Song, Weiguo Peng, Qian Sun, Sisi Peng, and Doug Kelley with the University of Rochester; Bjorn Sigurdsson and Pia Weikop with the University of Copenhagen; Virginia Pla, Hajime Hirase and Steve Goldman with both with the Universities of Rochester and Copenhagen; Daeyun Kim with the University of Minnesota; Jorge Castorena-Gonzalez with the Tulane University; and Michael Davis with the University of Missouri. The research was supported with funding from the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the National Institute of Neurological Disorders and Stroke, the Burroughs Wellcome Fund, the Joint Programme -- Neurodegenerative Disease Research, the Novo Nordisk Foundation, the Lundbeck Foundation, and the US Army Research Office.
12 Oct 2022
Rising demand in safe and reliable reversal of sedative effects of dexmedetomidine and medetomidine propelling revenue size in atipamezole market; preference as injectable for dogs hinges on good tolerability
Rising need for effective and safe anti-sedative solutions in pets underpins vast potential; pharmaceutical companies expanding online distribution networks to tap into thriving demand in North America
WILMINGTON, Del. , Oct. 12, 2022 /PRNewswire/ -- Rising adoption of anti-sedative agents for safe and quick reversal of sedative effects induced by dexmedetomidine and medetomidine in pets is a key pivot for expansion of profitable avenue for companies in atipamezole market. A TMR study on the growth dynamics found that intramuscular route of administration is expected to be largest revenue generator in atipamezole market. The atipamezole market size is projected to reach US$ 70 million by the end of 2030.
Growing regulatory approval of atipamezole solutions for injections in pets will spur future market demand for atipamezole market manufacturing. Veterinary hospitals are estimated to tap into the vast demand for atipamezole solutions in dogs and cats and other companion animals. On the other hand, the study authors observed that rise in investments by various pharmaceutical companies on expanding online pharmacies will also propel revenue streams.
Get Exclusive PDF Sample Copy of
Atipamezole Market
–
The TMR study found that leading players in atipamezole market are leaning on R&D for unveiling anti-sedation agents with high tolerability and effectiveness in recovery from anesthesia. Furthermore, drug manufacturers are taking initiatives in raising awareness of correct dosage of atipamezole and special precautions that pet owners and veterinarians need to exercise while administering the injections.
Key Findings of Atipamezole Market Study
Use as Anti-sedative Agents in Dogs and Cats Underpins Abundant Opportunities: Growing adoption of atipamezole in anti-sedative agents in dogs and cats is generating substantial growth opportunities for companies in the market. Especially in case of health dogs, the injections have demonstrated good tolerability, hence stoking the popularity of products. Educating clinicians of the contraindications will boost the outlook of the atipamezole market, opined the study.
R&D on Enhancing Tolerability and Safety of Atipamezole Solutions for Reversal of Medetomidine-Induced Sedation: Ongoing clinical studies and R&D by pharmaceutical companies will pave the way for increasing the tolerability and safety of anesthetic reversal agents. Stridently, the efforts will lead to new revenue streams for firms in the atipamezole market.
Massive Research Potential in Sleep Disorder Medications in Adults: Growing demand for medications for insomnia and sleep disorders is creating an incredible revenue potential in atipamezole market. Prevalence of sleep disorders in adults is catalyzing research on ant-sedative agents.
Ask for References –
Atipamezole Market: Key Drivers
Growing spending on pet care in conjunction with growing ownership of pets in developing and developed regions is a key driver of atipamezole market. Of note, ongoing clinical trials pertaining to medications that address complications of prolonged anesthesia in wide variety of species in veterinary medicine is likely to create tremendous lucrative opportunity for pharmaceutical companies.
R&D in sleep-inducing drugs for humans holds a massive potential, pivoting on the need for reducing prevalence of insomnia, will open up several new growth frontiers in atipamezole market.
Atipamezole Market: Regional Growth Dynamics
North America held a major share of the global atipamezole market in 2019. Rise in pet ownership over the past few years coupled with improving infrastructure of veterinary hospitals for companion animals has created massive revenue potential. In addition, rising spending on pet care in the U.S. has generated substantial lucrative demand for ant-sedative products in the region, thereby stirring the commercialization of atipamezole ingredients. Rise in demand for quality animal healthcare services is bolstering the prospects of the atipamezole market in North America.
Atipamezole Market: Competition Landscape
Multinational pharmaceutical companies in atipamezole market are reaping substantial revenue gains on the back of product approvals by regulatory agencies in various geographies. Key players are keenly expanding their product portfolio.
Some of them are Troy Laboratories Pty Ltd, Forte Healthcare Ltd., Chanelle Pharma Group, Vetoquinol UK Ltd, Jurox Pty Limited, Orion Corporation, Modern Veterinary Therapeutics, and Merck & Co., Inc.
Make an Enquiry Before Buying –
Atipamezole Market Segmentation
Application
Anti-sedative
Antitoxic (Off-label Use)
Route of Administration
Intramuscular
Intravenous
Others
Animal Type
Dogs
Cats
Others
Distribution Channel
Veterinary Hospitals
Retail Pharmacies
Online Pharmacies
Region
North America
Europe
Asia Pacific
Latin America
Middle East & Africa
Modernization of healthcare in terms of both infrastructure and services have pushed the healthcare industry to new heights, Stay Updated with Latest Healthcare Research Reports by Transparency Market Research:
Anticoagulant Reversal Drugs Market: The global anticoagulant reversal drugs market is anticipated to reach more than US$ 2.3 Bn by the end of 2031 at a CAGR of 11.3% from 2022 to 2031.
Macular Degeneration Treatment Market: The global macular degeneration treatment market is anticipated to reach more than US$ 21.1 Bn by the end of 2031 at a CAGR of 8.8% from 2022 to 2031.
PET Radiotracer Market: The global PET radiotracer market is anticipated to reach more than US$ 3.2 Bn by the end of 2031 at a CAGR of 8.5% from 2022 to 2031.
Gemcitabine HCL Market: The global gemcitabine HCl market is anticipated to reach more than US$ 1.3 Bn by 2031 at a CAGR of 7.8% from 2022 to 2031.
Homeopathic Products Market: The global homeopathic products market is anticipated to reach more than US$ 32.4 Bn by the end of 2031 at a CAGR of 11.6% from 2022 to 2031.
Pain Management Therapeutics Market: The global pain management therapeutics market is anticipated to reach more than US$ 98.0 Bn by the end of 2031 at a CAGR of 2.9% from 2022 to 2031.
Peptide Therapeutics Market: The global peptide therapeutics market is anticipated to reach more than US$ 91.25 Bn by 2031 at a CAGR of 8.8% from 2022 to 2031.
Collagen Peptide & Gelatin Market: The global collagen peptide and gelatin market is anticipated to reach more than US$ 7.8 Bn by the end of 2031 at a CAGR of 5.0% from 2022 to 2031.
About Transparency Market Research
Transparency Market Research, a global market research company registered at Wilmington, Delaware, United States, provides custom research and consulting services. Our exclusive blend of quantitative forecasting and trends analysis provides forward-looking insights for thousands of decision makers. Our experienced team of Analysts, Researchers, and Consultants use proprietary data sources and various tools & techniques to gather and analyse information.
Our data repository is continuously updated and revised by a team of research experts, so that it always reflects the latest trends and information. With a broad research and analysis capability, Transparency Market Research employs rigorous primary and secondary research techniques in developing distinctive data sets and research material for business reports.
For More Research Insights on Leading Industries, Visit Our YouTube Channel and hit subscribe for Future Update -
Contact
Rohit Bhisey
Transparency Market Research Inc.
CORPORATE HEADQUARTER DOWNTOWN,
1000 N. West Street,
Suite 1200, Wilmington, Delaware 19801 USA
Tel: +1-518-618-1030
USA – Canada Toll Free: 866-552-3453
Website:
Blog:
Email: [email protected]
Logo:
SOURCE Transparency Market Research
100 Deals associated with Atipamezole
Login to view more data
External Link
| KEGG | Wiki | ATC | Drug Bank |
|---|---|---|---|
| D03002 | Atipamezole | - |
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Depressive Disorder, Major | Phase 2 | Finland | - | |
| Reversal of Neuromuscular Blockade | Phase 1 | United States | 01 May 2023 | |
| Parkinson Disease | Preclinical | Finland | - |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or

Deal
Boost your decision using our deal data.
login
or

Core Patent
Boost your research with our Core Patent data.
login
or
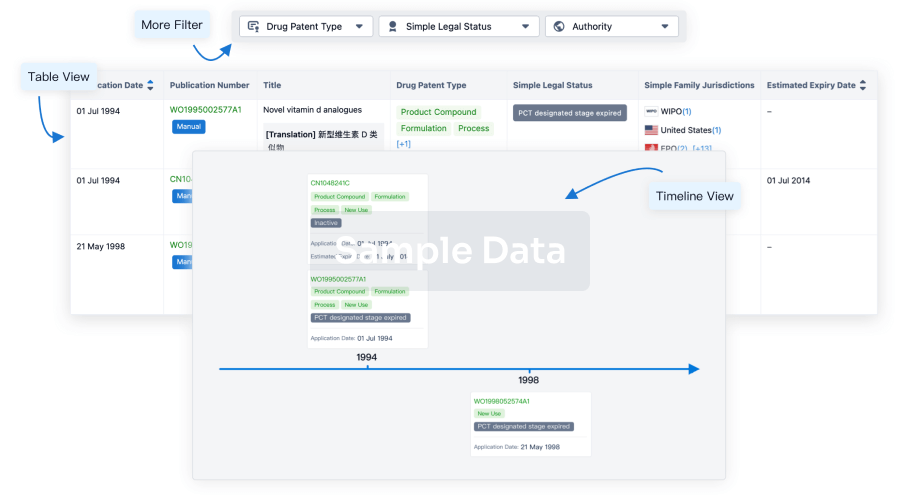
Clinical Trial
Identify the latest clinical trials across global registries.
login
or

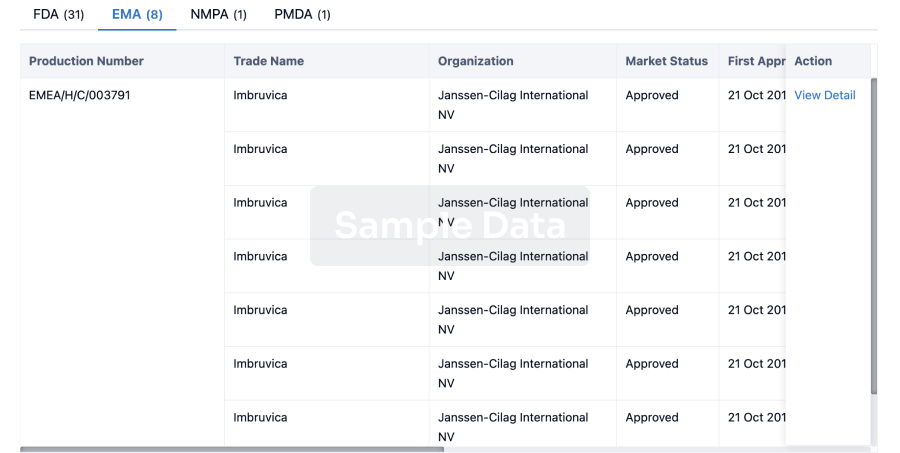
Approval
Accelerate your research with the latest regulatory approval information.
login
or
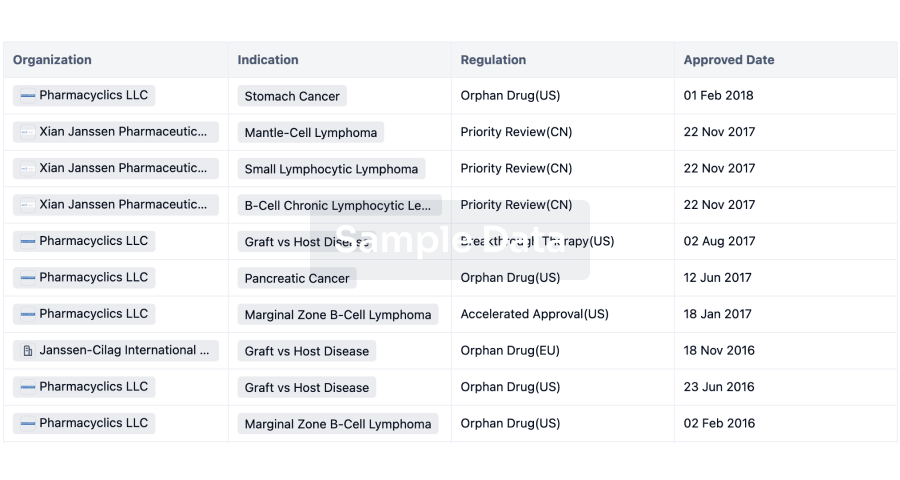
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

