6
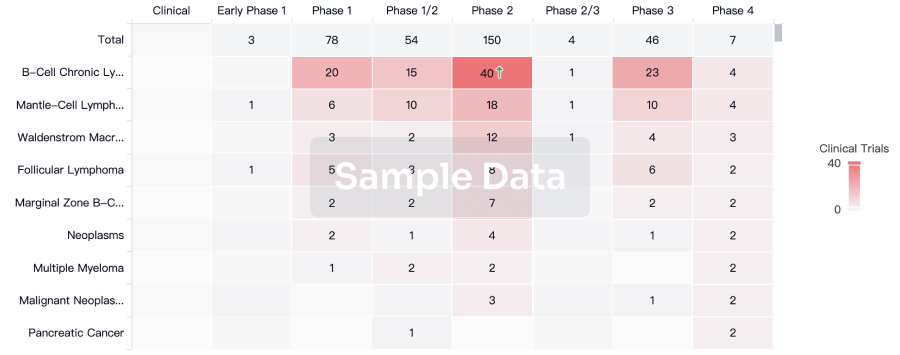
Clinical Trials associated with NY-ESO-1 peptide-pulsed autologous dendritic cell vaccine(National Cancer Institute)NY-ESO-1 TCR Engineered Adoptive Cell Transfer Therapy With Nivolumab PD-1 Blockade
This phase I trial studies the side effects and the best dose of nivolumab when given together with gene-modified T cells and vaccine therapy in treating patients with solid tumors that express the cancer-testes antigen NY-ESO-1 gene AND have spread from where it started to nearby tissue or lymph nodes (locally advanced) or distant organs (stage IV). T cells are a special type of white blood cells (immune cell) that have the ability to kill cancer cells. Nivolumab may block PD-1 which is found on T cells and help the immune system kill cancer cells. Placing a modified gene for the NY-ESO-1 T cell receptor (TCR) into the patients' T cells in the laboratory and then giving them back to the patient may help the body build an immune response to kill tumor cells that express NY-ESO-1. Dendritic cells are another type of blood cell that can teach other cells in the body to look for cancer cells and attack them. Giving a dendritic cell vaccine with the NY-ESO-1 protein may help dendritic cells teach the immune system to target cancer cells expressing that protein, and further help the T cells attack cancer. Giving nivolumab together with gene-modified T-cells and dendritic cell vaccine may teach the immune system to recognize and kill cancer cells that express NY-ESO-1.
Phase II Study of Metastatic Cancer That Expresses NY-ESO-1 Using Lymphodepleting Conditioning Followed by Infusion of Anti-NY ESO-1 TCR-Gene Engineered Lymphocytes
Background:
-This study uses an experimental cancer treatment that uses the patient s own lymphocytes (type of white blood cell), which are specially selected and genetically modified to target and destroy their tumor.
Objectives:
-To test the safety of the treatment and determine if it can cause the patient s tumor to shrink.
Eligibility:
* Patients greater than 18 years and less than or equal to 66 years of age whose cancer has spread beyond the original site and does not respond to standard treatment.
* Patients have tissue type human leukocyte antigen (HLA)-A*0201.
* Patients cancer cells have the ESO-1 gene.
Design:
* Workup: Patients have scans, x-rays, laboratory tests, and other tests as needed.
* Patients have leukapheresis to collect cells for laboratory treatment and later reinfusion. For this procedure, whole blood is collected thorough a tube in a vein, the desired cells are extracted from the blood, and the rest of the blood is returned to the patient.
* Chemotherapy: Patients have low-dose chemotherapy for 1 week to prepare the immune system to receive the treated lymphocytes.
* Cell infusion and aldesleukin (IL-2) treatment: Patients receive the lymphocytes by a 30-minute infusion through a vein. Starting within 24 hours of the infusion, they receive high-dose aldesleukin infusions every 8 hours for up to 5 days (maximum15 doses).
* Recovery: Patients rest for 1 to 2 weeks to recover from the effects of chemotherapy and aldesleukin.
* Tumor biopsy: Patients may be asked to undergo a biopsy (surgical removal of a small piece of tumor) after treatment to look at the effects of treatment on the immune cells in the tumor.
* Follow-up: After treatment is completed, patients return to the clinic once a month for several months for physical examinations, a review of side effects, laboratory tests and scans. They may undergo leukapheresis at some visits to look at the effect of treatment on the immune system and check the viability of the infused cells. Patients then return to the National Institute of Health (NIH) clinic once a year for 5 years and then complete a follow-up questionnaire for another 10 years.
* Retreatment: Patients whose tumor shrinks or disappears following treatment and then recurs may receive one additional treatment, using the same regimen of chemotherapy, lymphocyte infusion and IL-2 treatment.
Treatment Of Patients With Metastatic Melanoma Using Nonmyeloablative But Lymphocyte Depleting Regimen Followed By The Administration Of In Vitro Sensitized Lymphocytes Reactive With ESO-1 Antigen
RATIONALE: Drugs used in chemotherapy, such as cyclophosphamide and fludarabine, work in different ways to stop tumor cells from dividing so they stop growing or die. Treating a person's lymphocytes in the laboratory and reinfusing them may replace immune cells destroyed by chemotherapy. Vaccines made from peptides may make the body build an immune response to kill tumor cells. Giving a vaccine with Montanide ISA-51 may cause a stronger immune response and kill more tumor cells. Interleukin-2 may stimulate a person's lymphocytes to kill tumor cells.
PURPOSE: This phase II trial is studying how well lymphocyte-depleting nonmyeloablative (not damaging to bone marrow) chemotherapy followed by autologous lymphocyte infusion, peptide vaccine plus Montanide ISA-51, and interleukin-2 works in treating patients with metastatic melanoma.
100 Clinical Results associated with NY-ESO-1 peptide-pulsed autologous dendritic cell vaccine(National Cancer Institute)
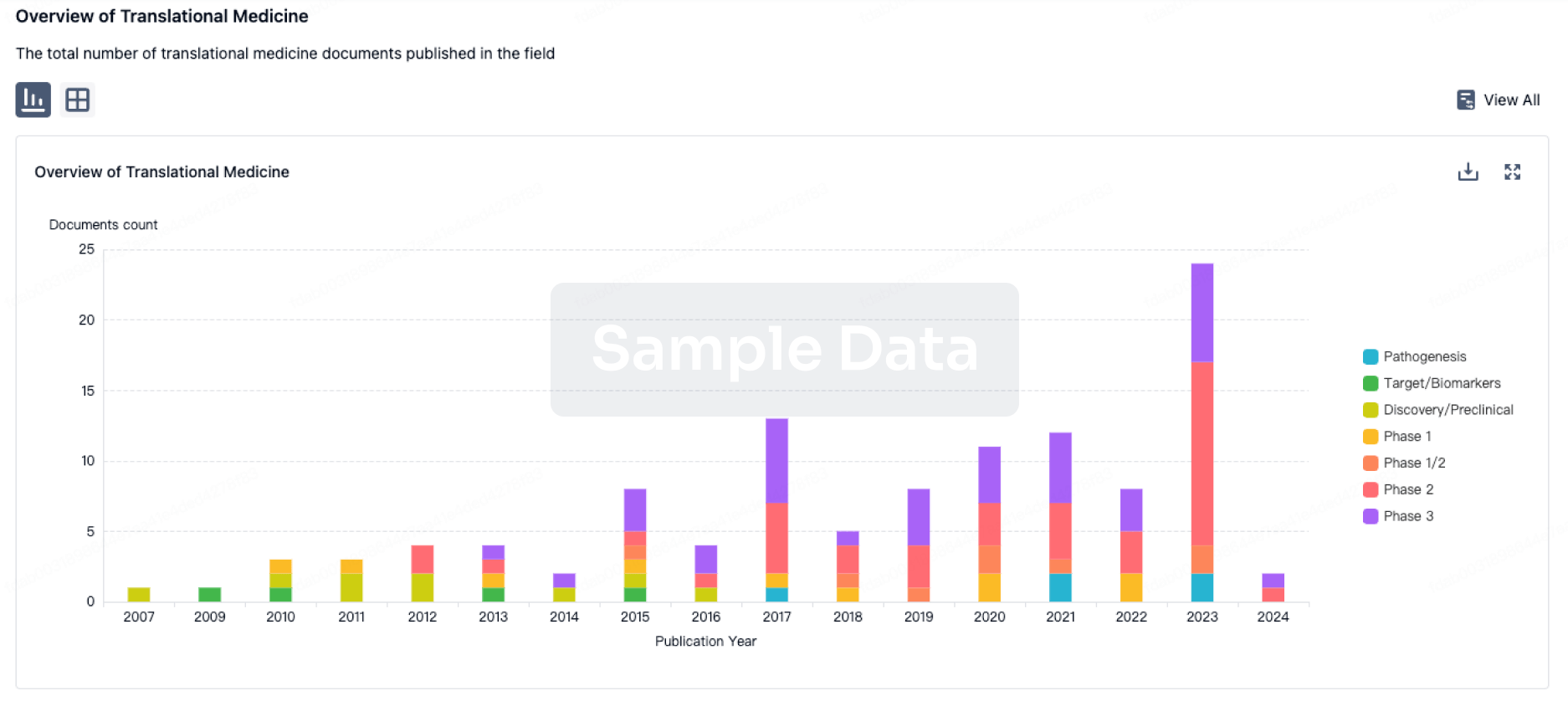
100 Translational Medicine associated with NY-ESO-1 peptide-pulsed autologous dendritic cell vaccine(National Cancer Institute)
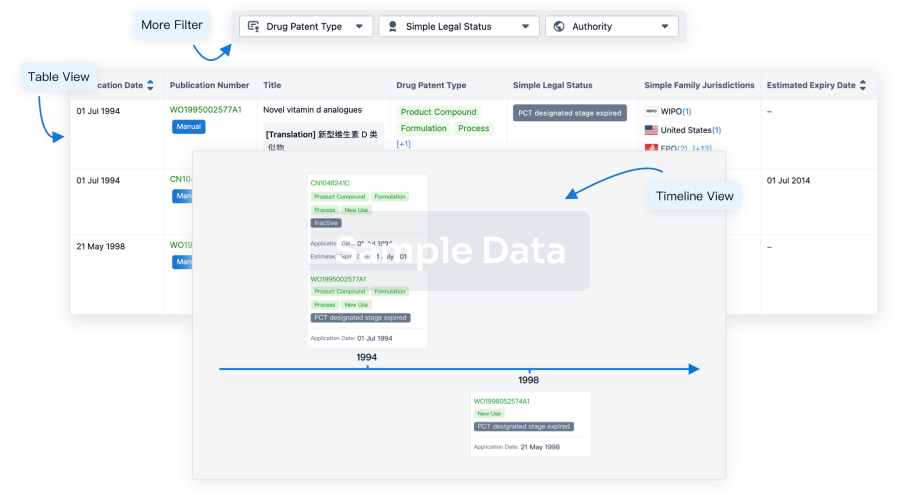
100 Patents (Medical) associated with NY-ESO-1 peptide-pulsed autologous dendritic cell vaccine(National Cancer Institute)
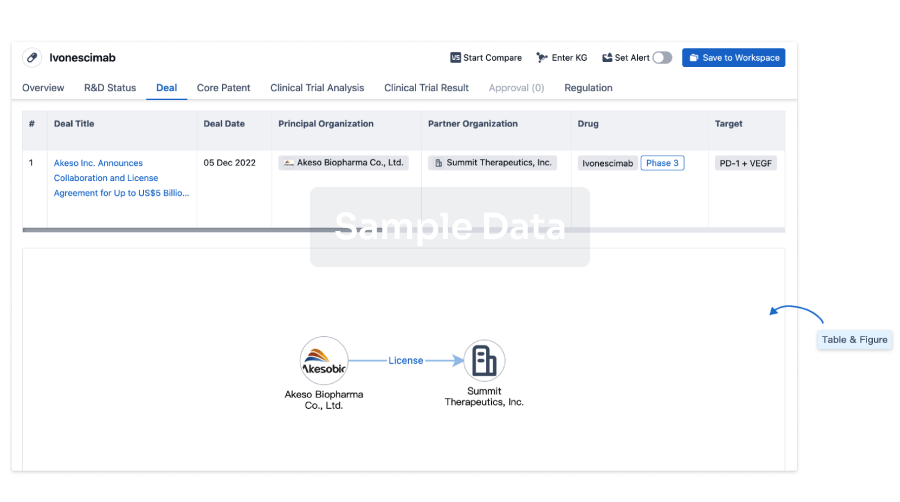
100 Deals associated with NY-ESO-1 peptide-pulsed autologous dendritic cell vaccine(National Cancer Institute)