Request Demo
Last update 08 May 2025
Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII
Private Company|Italy
Private Company|Italy
Last update 08 May 2025
Overview
Related
1
Drugs associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIIITarget- |
Mechanism Stem cell replacements |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date- |
6
Clinical Trials associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIIINCT06354829
Creation of a Collection of Medical Images to Facilitate Their Use for Future Not-for-profit Research
This is a not-for-profit project for the collection, archiving and reuse of magnetic resonance imaging, computed tomography and ultrasound images, and related demographic and clinical data, for research purposes only.
Start Date07 Jan 2025 |
Sponsor / Collaborator |
NCT06807255
Lactate Values During Labour and Their Correlation With Maternal and Foetal Outcome: a Prospective Observational Single-centre Study
Postpartum haemorrhage (PPH) represents a significant cause of morbidity in the obstetric population, with a mortality rate of 140,000 women per year, and the predominant cause of PPH (70%) is uterine atony.
Consequently, elevated lactate levels during labour could influence maternal and foetal well-being. We decided to assess lactate concentrations during labour in women receiving neuraxial anaesthesia and evaluate the association between high lactate levels and adverse maternal and foetal outcomes.
The secondary aims of the study were to assess lactate levels at different stages of labour and investigate whether increased lactate concentrations could influence neonatal cord pH upon delivery.
Consequently, elevated lactate levels during labour could influence maternal and foetal well-being. We decided to assess lactate concentrations during labour in women receiving neuraxial anaesthesia and evaluate the association between high lactate levels and adverse maternal and foetal outcomes.
The secondary aims of the study were to assess lactate levels at different stages of labour and investigate whether increased lactate concentrations could influence neonatal cord pH upon delivery.
Start Date01 May 2023 |
Sponsor / Collaborator |
NCT06884631
Metabolic Exercise Test Data Combined with Cardiac and Kidney Indexes (MECKI) Score Evolution: Study of Cardiovascular Risk in Patients with Heart Failure
Heart failure is a complex condition involving multiple organs beyond the cardiovascular system, all influencing disease progression and prognosis. Accurate risk assessment requires considering multiple variables, as no single parameter alone provides a complete prognostic picture.
This has led to the development of prognostic models combining clinical and laboratory parameters. Some of these models incorporate cardiopulmonary exercise testing (CPET), which provides key prognostic indicators. Since the 1990s, CPET has been recommended in heart failure management guidelines due to its strong prognostic value when combined with clinical data.
However, existing risk models often exclude important predictors such as ventilatory parameters from CPET (VE/VCO₂), renal function, and hemoglobin levels. To address this gap, in 2012 the investigators developed the MECKI (Metabolic Exercise test data combined with Cardiac and Kidney Indexes) score, integrating oxygen consumption, ventilatory efficiency, and easily accessible biochemical and echocardiographic parameters. Unlike previous models requiring extensive data collection, MECKI is based on only six variables, making it practical and effective.
Recent studies suggest the need to update the cutoff values and parameters used for risk stratification, as new therapies and treatment strategies may significantly alter prognostic accuracy in different patient populations.
This study aims to expand and refine the MECKI score by updating the patient dataset, optimizing its performance in specific subgroups, and aligning it with emerging therapeutic approaches.
Additionally, the investigators will evaluate whether the model's risk accuracy varies in advanced-stage patients, those with comorbidities, or under different treatment regimens. This could lead to correction factors that enhance the score's predictive power across diverse clinical scenarios, further improving its applicability and reliability in heart failure management.
This has led to the development of prognostic models combining clinical and laboratory parameters. Some of these models incorporate cardiopulmonary exercise testing (CPET), which provides key prognostic indicators. Since the 1990s, CPET has been recommended in heart failure management guidelines due to its strong prognostic value when combined with clinical data.
However, existing risk models often exclude important predictors such as ventilatory parameters from CPET (VE/VCO₂), renal function, and hemoglobin levels. To address this gap, in 2012 the investigators developed the MECKI (Metabolic Exercise test data combined with Cardiac and Kidney Indexes) score, integrating oxygen consumption, ventilatory efficiency, and easily accessible biochemical and echocardiographic parameters. Unlike previous models requiring extensive data collection, MECKI is based on only six variables, making it practical and effective.
Recent studies suggest the need to update the cutoff values and parameters used for risk stratification, as new therapies and treatment strategies may significantly alter prognostic accuracy in different patient populations.
This study aims to expand and refine the MECKI score by updating the patient dataset, optimizing its performance in specific subgroups, and aligning it with emerging therapeutic approaches.
Additionally, the investigators will evaluate whether the model's risk accuracy varies in advanced-stage patients, those with comorbidities, or under different treatment regimens. This could lead to correction factors that enhance the score's predictive power across diverse clinical scenarios, further improving its applicability and reliability in heart failure management.
Start Date10 Feb 2021 |
Sponsor / Collaborator |
100 Clinical Results associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII
Login to view more data
0 Patents (Medical) associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII
Login to view more data
250
Literatures (Medical) associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII08 Apr 2025·Clinical Kidney Journal
Renal functional reserve in living kidney donors
Article
Author: Rivero Viera, Yaiza ; Martín Izquierdo, Edduin ; Luis-Lima, Sergio ; Hernández Marrero, Domingo ; González Cabrera, Faina ; Stefany Rincón, Marian ; Alonso Bethencourt, Alejandro ; Díaz Martín, Laura ; Fariña Hernández, Arminda ; González, Selene ; Acosta Sorensen, Cristian ; González Rinne, Ana ; Escamilla, Beatriz ; Cruz, Coriolano ; Cabello Moya, Elisa ; Gaspari, Flavio ; Reseghetti, Elia ; Porrini, Esteban ; Morales, Adelaida ; González Rinne, Federico ; Pérez Tamajón, Lourdes
01 Apr 2025·Transplantation and Cellular Therapy
Prospective Validation of CAR-HEMATOTOX and a Simplified Version Predict Survival in Patients with Large B-Cell Lymphoma Treated with Anti-CD19 CAR T-Cells: Data from CART-SIE Study
Article
Author: Barone, Angelica ; Martino, Massimo ; Chiusolo, Patrizia ; Musso, Maurizio ; Olivieri, Jacopo ; Stella, Federico ; Brunello, Lucia ; Russo, Domenico ; Krampera, Mauro ; Farina, Lucia ; Cutini, Ilaria ; Sorà, Federica ; Santoro, Armando ; Pennisi, Martina ; Angelillo, Piera ; Grillo, Giovanni ; Novo, Mattia ; Zinzani, Pierluigi ; Chiappella, Annalisa ; Barbui, Anna Maria ; Tisi, Maria Chiara ; Casadei, Beatrice ; Cavallo, Federica ; Ljevar, Silva ; Corradini, Paolo ; Arcaini, Luca ; Rocco, Alice Di ; Massaia, Massimo ; Bonifazi, Francesca ; Miceli, Rosalba ; Bramanti, Stefania
04 Mar 2025·Clinical Kidney Journal
Mechanisms and treatment of obesity-related hypertension—Part 2: Treatments
Review
Author: Abbate, Manuela ; Ruggenenti, Piero ; Parvanova, Aneliya ; Reseghetti, Elia
1
News (Medical) associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII06 Sep 2022
Positive Agenzia Italiana del Farmaco (AIFA) decision provides reimbursed access to the first medicine available for the treatment of all types of PFIC, a rare and devastating disorder that affects young children and causes progressive, life-threatening liver diseaseBylvay receives “Full Therapeutic Innovation” special designation status by AIFA for select products with high unmet need, added clinical benefit, robustness of the scientific evidence BOSTON, Sept. 06, 2022 (GLOBE NEWSWIRE) -- Albireo Pharma, Inc. (Nasdaq: ALBO), a rare liver disease company developing novel bile acid modulators to treat pediatric and adult liver diseases, today announced that the Italian Medicines Agency, also known as Agenzia Italiana del Farmaco (AIFA), has enabled reimbursed access to Bylvay (odevixibat) for the treatment of all types of progressive familial intrahepatic cholestasis (PFIC) patients in Italy. A potent, oral, once-daily, non-systemic ileal bile acid transport inhibitor, Bylvay has minimal systemic exposure and acts locally in the small intestine as a treatment for PFIC, a rare and devastating disorder that causes progressive, liver disease. "It’s extremely important to see the positive decision by AIFA to enable access to Bylvay to treat patients in need. As the first approved medicine for PFIC, I’m relieved to now be able to offer a non-surgical treatment option that provides meaningful clinical benefits that can improve the lives of patients and families,” said Dr. Lorenzo D’Antiga, Director, Unit of Hepatology, Gastroenterology and Pediatric Transplantation, Papa Giovanni XXIII Hospital. Patients with PFIC have impaired bile flow, or cholestasis, and the resulting bile build-up in liver cells causes life-threatening liver disease and symptoms, such as intense itching, poor sleep, delayed growth, and diminished quality of life. The harmful impacts of the disease extend beyond the individuals with PFIC to those caring for them as shown by the 2022 multinational PICTURE study, which revealed PFIC negatively affects caregivers’ quality of life, relationships, and career prospects. “The burden of the disease is devastating for children and families living with PFIC. Severe itching can cause a tremendous impact on patients and disrupt basic daily activities resulting in loss of sleep, poor attention, and lower school performance. Intractable pruritus can, by itself, justify liver transplantation in these patients. We are thrilled to have Bylvay as an innovative therapeutic non-surgical option that could significantly improve disease management and, potentially, modify the natural history of the disease,” said Prof. Giuseppe Maggiore, Director of the Division of Hepatology, Gastroenterology, Digestive Endoscopy, and Nutrition, Pediatric Hospital Bambino Gesù. Bylvay was granted “Full Therapeutic Innovation” status by AIFA, a special designation applied to select drug applications that address a high unmet need, added clinical benefit, and robustness of the scientific evidence. This status provides access to dedicated national funding. For Healthcare Provider General Inquires, please email: Italy@albireopharma.com “Bylvay has the potential to transform the lives of those impacted by PFIC, and availability in Italy marks an important milestone for our PFIC community,” explained Francesca Lombardozzi, Head of PFIC Italia Network and the mother of a 3-year-old child living with PFIC. “I know firsthand the extreme burden and challenges PFIC patients and caregivers are facing. This is a great first step for the whole community, and we hope others will follow. I’m grateful for the Albireo team’s continued efforts to provide access to this critical medication that will make a huge impact on our lives.” “We are grateful to AIFA for this positive decision, recognizing the clinical and economic value of Bylvay,” said Thomas Topini, General Manager, Italy at Albireo. “It is because of AIFA’s engagement that we were able to accelerate reimbursed access to Bylvay and help PFIC patients and families in Italy living with the devastating effects of this disease.” Bylvay was approved in Europe for the treatment of all types of PFIC in patients aged 6 months or older, based on the PEDFIC 1 study and PEDFIC 2 open-label extension (OLE) study. This availability marks the fourth reimbursement approval for Bylvay in Europe, following launches in Germany, England, Wales & Northern Ireland, and Scotland. Bylvay is currently being evaluated in the ASSERT Phase 3 study for Alagille syndrome (ALGS) and in the BOLD Phase 3 study for patients with biliary atresia. The ASSERT and BOLD studies remain on track to report topline data in the fall of 2022 and 2024, respectively. PEDFIC 1 & PEDFIC 2 Studies The decision by the Italian Medicines Agency is based on data from PEDFIC 1 and PEDFIC 2, the largest, global, Phase 3 trials ever conducted in PFIC. In PEDFIC 1, a randomized, double-blind, placebo-controlled study, Bylvay met both its pruritus (p=0.004) and serum bile acid (p=0.003) primary endpoints and was well tolerated with low incidence of drug-related diarrhea/frequent bowel movements (9.5% of treated patients vs. 5.0% of placebo patients). PEDFIC 2, a long-term, open-label Phase 3 extension study, affirmed Bylvay delivered sustained reductions in serum bile acid, as well as improvements in pruritus assessments, growth and sleep and markers of liver function in patients treated up to 48 weeks in an interim analysis. Across both studies, Bylvay was well tolerated. The most common adverse reactions for Bylvay were diarrhea, liver test abnormalities, vomiting, abdominal pain, and fat-soluble vitamin deficiency. There were no serious treatment-related adverse events reported in any clinical study with Bylvay. About Bylvay (odevixibat) Bylvay is the first drug approved in the U.S. for the treatment of pruritus in patients 3 months of age and older in all types of progressive familial intrahepatic cholestasis (PFIC). Limitation of Use: Bylvay may not be effective in PFIC type 2 patients with ABCB11 variants resulting in non-functional or complete absence of bile salt export pump protein (BSEP-3). The European Commission (EC) and UK Medicines and Healthcare Products Regulatory Agency (MHRA) have also granted marketing authorization of Bylvay for the treatment of PFIC in patients aged 6 months or older. Bylvay is available in Italy, Germany and the UK and will be available for sale in other European countries following pricing and reimbursement approval. A potent, once-daily, non-systemic ileal bile acid transport inhibitor, Bylvay acts locally in the small intestine. Bylvay can be taken as a capsule for patients that are able to swallow capsules, or opened and sprinkled onto food, which is a factor of key importance for adherence in a pediatric patient population. The most common adverse reactions for Bylvay are diarrhea, liver test abnormalities, vomiting, abdominal pain, and fat-soluble vitamin deficiency. The medicine can only be obtained with a prescription. For more information about using Bylvay, see the package leaflet or contact your doctor or pharmacist. For full prescribing information, visit www.bylvay.com. In the U.S. and Europe, Bylvay has orphan exclusivity for its approved PFIC indications, and orphan designations for the treatment of ALGS, biliary atresia and primary biliary cholangitis. Bylvay is being evaluated in the ongoing PEDFIC 2 open-label trial in patients with PFIC, in the BOLD Phase 3 study for patients with biliary atresia and the ASSERT Phase 3 study for ALGS. Important Safety Information The most common adverse reactions for Bylvay are diarrhea, liver test abnormalities, vomiting, abdominal pain, and fat-soluble vitamin deficiency.Liver Test Abnormalities: Patients should obtain baseline liver tests and monitor during treatment. Dose reduction or treatment interruption may be required if abnormalities occur. For persistent or recurrent liver test abnormalities, consider treatment discontinuation.Diarrhea: Treat dehydration. Treatment interruption or discontinuation may be required for persistent diarrhea.Fat-Soluble Vitamin (FSV) Deficiency: Patient should obtain baseline vitamin levels and monitor during treatment. Supplement if deficiency is observed. If FSV deficiency persists or worsens despite FSV supplementation, discontinue treatment. About Albireo Albireo Pharma is a rare disease company focused on the development of novel bile acid modulators to treat pediatric and adult liver diseases. Albireo’s lead product, Bylvay, was approved by the U.S. FDA as the first drug for the treatment of pruritus in all types of progressive familial intrahepatic cholestasis (PFIC), and it is also being developed to treat other rare pediatric cholestatic liver diseases with Phase 3 trials in Alagille syndrome (ALGS) and biliary atresia, as well as Open-label Extension (OLE) studies for PFIC and ALGS. In Europe, Bylvay is reimbursed for the treatment of PFIC in Germany, England, Wales & Northern Ireland, Scotland, and Italy. The Company has also completed a Phase 1 clinical trial for A3907 to advance development in adult cholestatic liver disease, with IND-enabling studies progressing with A2342 for viral and cholestatic liver disease. Albireo was spun out from AstraZeneca in 2008 and is headquartered in Boston, Massachusetts, with its key operating subsidiary in Gothenburg, Sweden. For more information on Albireo, please visit www.albireopharma.com. Forward-Looking Statements This press release includes “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995. Forward-looking statements include statements, other than statements of historical fact, regarding, among other things: Albireo’s commercialization plans; the plans for, or progress, scope, cost, initiation, duration, enrollment, results or timing for availability of results of, development of Bylvay, A3907, A2342 or any other Albireo product candidate or program; the PEDFIC 2 open-label trial in patients with PFIC; the pivotal trial for Bylvay in biliary atresia (BOLD); the pivotal trial for Bylvay in Alagille syndrome (ASSERT); the Phase 2 study for A3907 the IND-enabling or clinical studies for A2342; the target indication(s) for development or approval; the timing for initiation or completion of or availability or reporting of results from any clinical trial, including the long-term open-label extension study for Bylvay in PFIC, the BOLD and ASSERT trials, the Phase 2 study for A3907, and the IND-enabling and clinical studies for A2342; potential regulatory approval and plans for potential commercialization of Bylvay in additional countries; the potential benefits or competitive position of Bylvay or any other Albireo product candidate or program or the commercial opportunity in any target indication;; or Albireo’s plans, expectations or future operations, financial position, revenues, costs or expenses. Albireo often uses words such as “anticipates,” “believes,” “plans,” “expects,” “projects,” “future,” “intends,” “may,” “will,” “should,” “could,” “estimates,” “predicts,” “potential,” “planned,” “continue,” “guidance,” or the negative of these terms or other similar expressions to identify forward-looking statements. Actual results, performance or experience may differ materially from those expressed or implied by any forward-looking statement as a result of various risks, uncertainties and other factors, including, but not limited to: results achieved in Bylvay in the treatment of patients with PFIC may be different than observed in clinical trials, and may vary among patients; potential negative impacts of the COVID-19 pandemic, including on manufacturing, supply, conduct or initiation of clinical trials, or other aspects of our business; whether favorable findings from clinical trials of Bylvay to date, including findings in indications other than PFIC, will be predictive of results from other clinical trials of Bylvay; the timing for initiation or completion of, or for availability of data from, clinical trials of Bylvay, including BOLD and ASSERT and the Phase 2 clinical trial of A3907, and the outcomes of such trials; Albireo’s ability to obtain coverage, pricing or reimbursement for approved products in the United States or Europe; delays or other challenges in the recruitment of patients for, or the conduct of, the Company’s clinical trials; and the Company’s critical accounting policies. These and other risks and uncertainties that Albireo faces are described in greater detail under the heading “Risk Factors” in Albireo’s most recent Annual Report on Form 10-K or in subsequent filings that it makes with the Securities and Exchange Commission. As a result of risks and uncertainties that Albireo faces, the results or events indicated by any forward-looking statement may not occur. Albireo cautions you not to place undue reliance on any forward-looking statement. In addition, any forward-looking statement in this press release represents Albireo’s views only as of the date of this press release and should not be relied upon as representing its views as of any subsequent date. Albireo disclaims any obligation to update any forward-looking statement except as required by applicable law. Media Contacts: Colleen Alabiso, 857-356-3905, colleen.alabiso@albireopharma.com Lance Buckley, 917-439-2241, lbuckley@lippetaylor.com Investor Contact:Hans Vitzthum, LifeSci Advisors, LLC., 617-430-7578
Collaborate
100 Deals associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII
Login to view more data
100 Translational Medicine associated with Azienda Socio Sanitaria Territoriale Papa Giovanni XXIII
Login to view more data
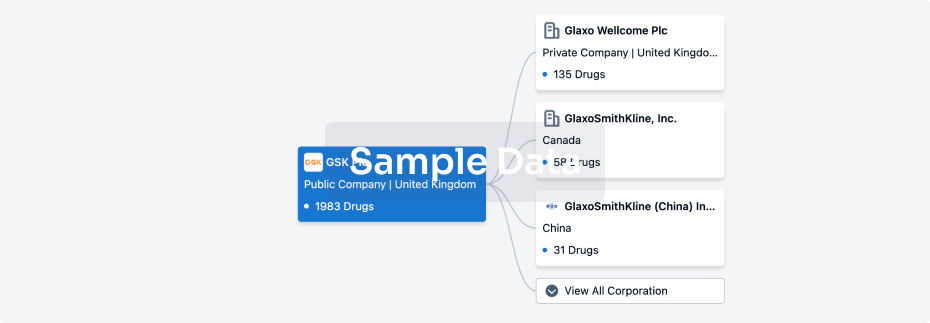
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 18 Dec 2025
The statistics for drugs in the Pipeline is the current organization and its subsidiaries are counted as organizations,Early Phase 1 is incorporated into Phase 1, Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3
Other
1
Login to view more data
Current Projects
| Drug(Targets) | Indications | Global Highest Phase |
|---|---|---|
Autologous Adipose-derived Stem Cells(ASST Papa Giovanni XXIII) | Perianal fistula due to Crohn's disease More | Pending |
Login to view more data
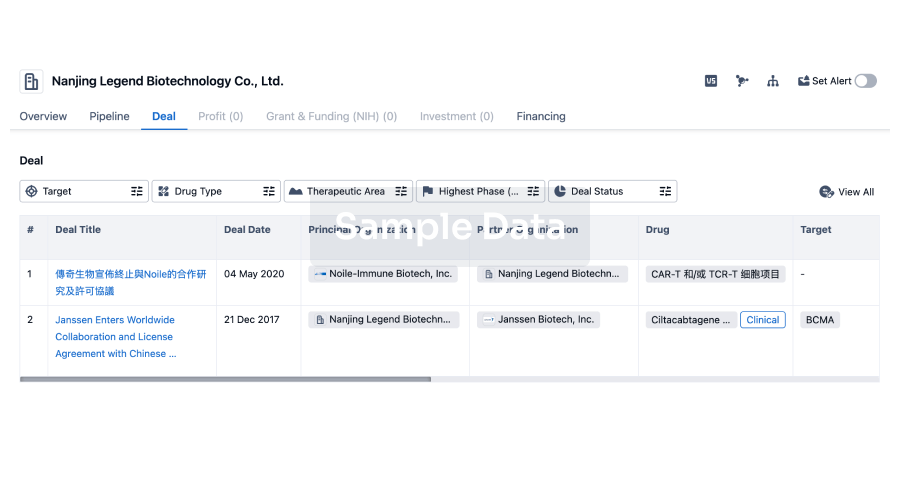
Deal
Boost your decision using our deal data.
login
or
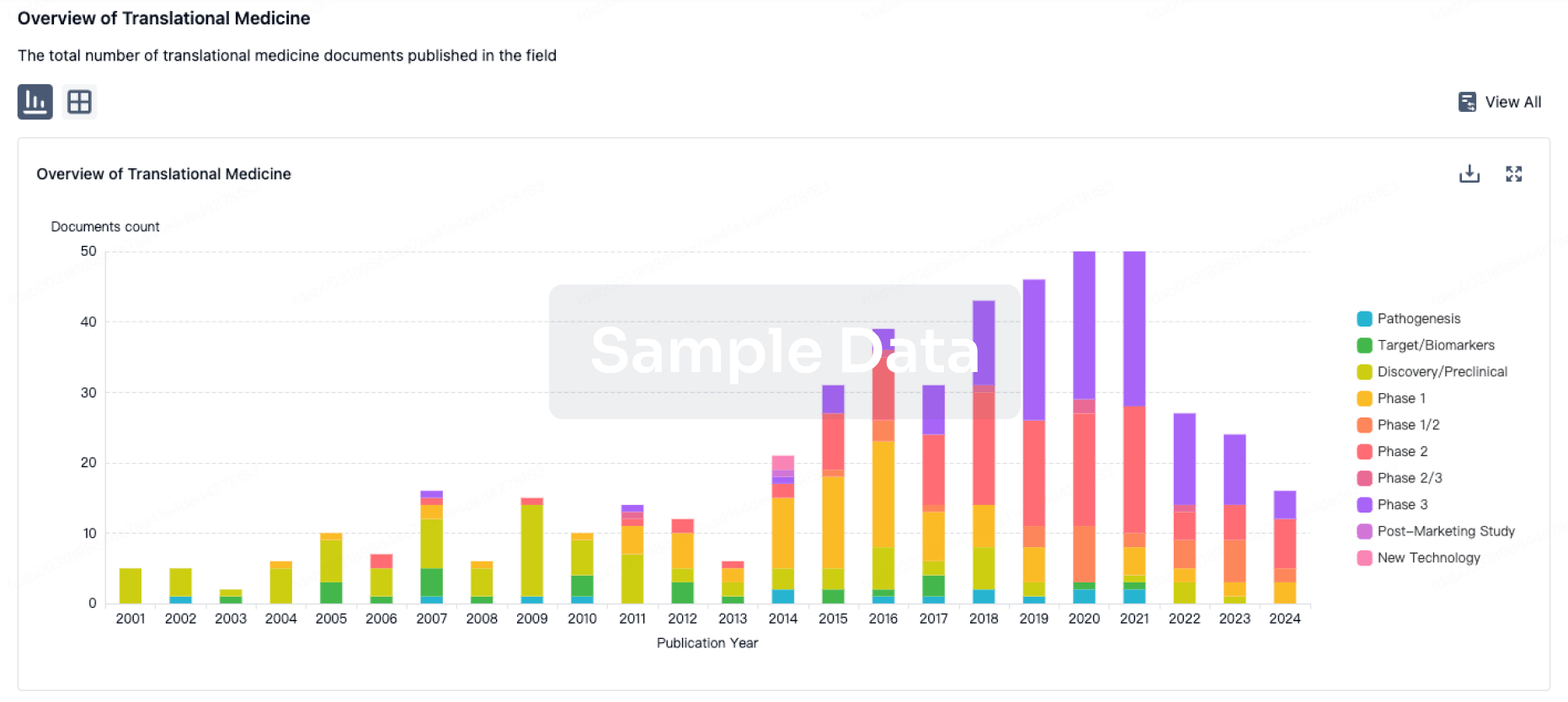
Translational Medicine
Boost your research with our translational medicine data.
login
or
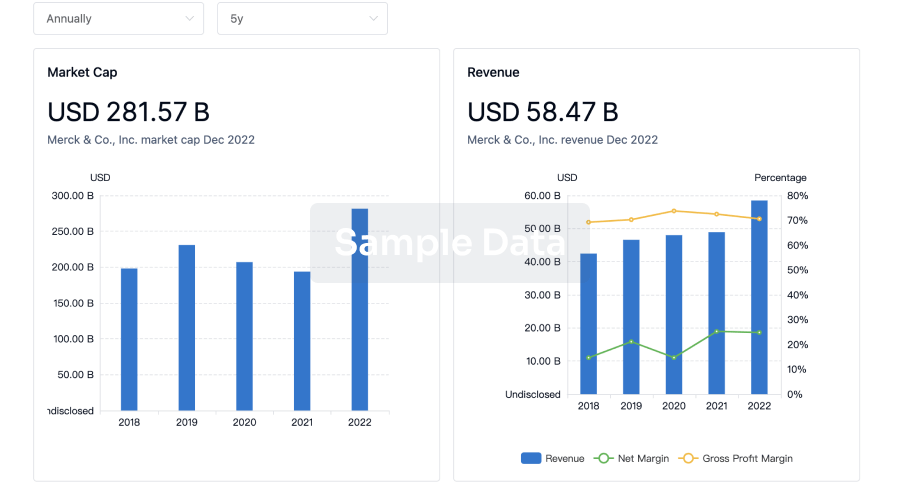
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
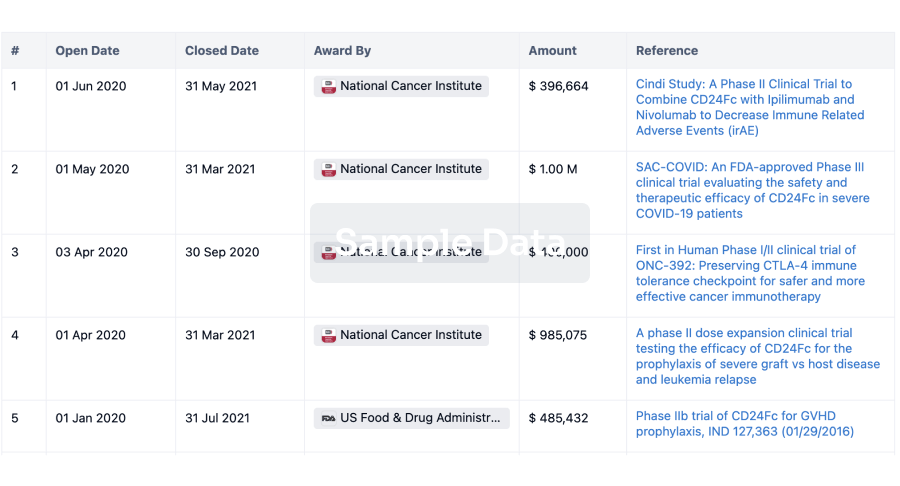
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
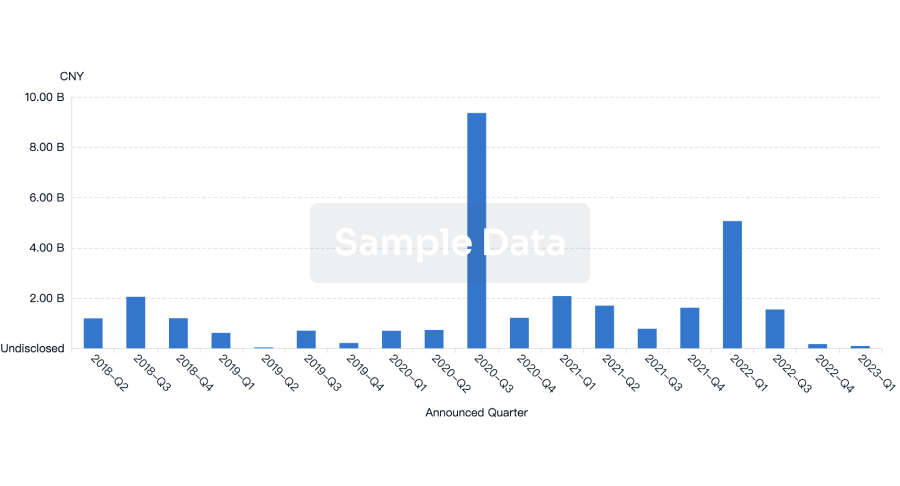
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
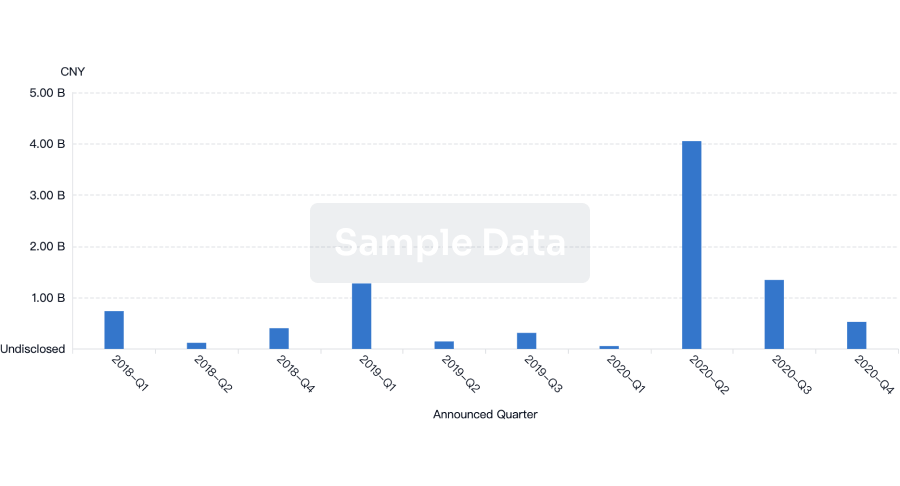
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

