Request Demo
Last update 11 Aug 2025

Cornea Research Foundation of America , Inc.
Last update 11 Aug 2025
Overview
Related
8
Clinical Trials associated with Cornea Research Foundation of America , Inc.NCT04787471
Randomized Comparison of Standard vs. Accelerated Corneal Crosslinking for Treatment of Corneal Neovascularization With or Without Concomitant Inflammation and/or Infection
The study objective is to assess safety and efficacy of photo-activation of riboflavin for treatment of corneal neovascularization with or without concomitant inflammation and/or infection.
Start Date03 May 2021 |
Sponsor / Collaborator  Price Vision Group Price Vision Group [+1] |
NCT04018417
A Randomized, Double-masked, Placebo-controlled Study of the Safety of Amphotericin 0.255 μg/mL in Optisol-GS
With the increasing popularity of endothelial keratoplasty, a coincident increase in the rate of fungal infections post-keratoplasty has been seen in the United States. In this study, the eye bank will harvest pairs of donor corneas and randomize one cornea from each pair to be stored in Optisol-GS per Eye Bank Association of America guidelines. The eye bank will add amphotericin B 0.255 μg/mL (antifungal) to the storage solution for the mate cornea. The study donor corneas will be assigned to participants who are scheduled to undergo Descemet membrane endothelial keratoplasty. The surgeons, participants, and evaluators will remain masked regarding the donor cornea storage solution assignment. The participants will be followed for 6 months.
Start Date03 Jul 2019 |
Sponsor / Collaborator |
NCT03248037
Randomized, Double-masked, Placebo-controlled Evaluation of Netarsudil for Prevention of Corticosteroid-induced Intraocular Pressure Elevation
Cornea transplant recipients who are using topical corticosteroids long-term to prevent transplant rejection will be randomized to use netarsudil or placebo.
Start Date05 Sep 2017 |
Sponsor / Collaborator |
100 Clinical Results associated with Cornea Research Foundation of America , Inc.
Login to view more data
0 Patents (Medical) associated with Cornea Research Foundation of America , Inc.
Login to view more data
93
Literatures (Medical) associated with Cornea Research Foundation of America , Inc.01 Nov 2024·Cornea
Descemet Membrane Endothelial Keratoplasty: 10-Year Cell Loss and Failure Rate Compared With Descemet Stripping Endothelial Keratoplasty and Penetrating Keratoplasty
Article
Author: Kanapka, Lauren ; Price, Marianne O. ; Lass, Jonathan H. ; Kollman, Craig ; Price, Francis W.
Purpose::
The aim of this study was to assess long-term endothelial cell loss (ECL) and graft failure with Descemet membrane endothelial keratoplasty (DMEK) and Descemet stripping endothelial keratoplasty (DSEK) versus penetrating keratoplasty (PK) performed for the same indications (primarily Fuchs dystrophy and pseudophakic corneal edema) in the Cornea Donor Study.
Methods::
This retrospective study included consecutive primary DMEK (529 recipients, 739 eyes) and DSEK cases (585 recipients, 748 eyes) with 1 or more endothelial cell density (ECD) measurements at 6 months to 16 years. Main outcomes were ECD, longitudinal ECL, and graft failure.
Results::
Between 6 months and 8 years the ECD declined linearly by approximately 118 cells/mm2/yr after DMEK and 112 cells/mm2/yr after DSEK. Beyond 8 years postoperatively the rate of decline slowed substantially. Selective dropout from graft failure did not significantly affect the ECD trend. At 10 years, median ECL (interquartile range) was 63% (45, 73) with DMEK, 68% (48, 78) with DSEK, and 76% (70, 82) with PK (P = 0.01 DMEK vs. DSEK, P <0.001 DMEK vs. PK, and P < 0.001 DSEK vs. PK). The proportion of surviving grafts with 10-year ECD <500 cells/mm2 was 1.4% with DMEK, 7.3% with DSEK, and 23.9% with PK. The cumulative risk of graft failure between 6 months and 10 years was 5% with DMEK, 11% with DSEK, and 19% with PK (P < 0.001).
Conclusions::
Compared with PK and DSEK, DMEK had significantly lower ECL and significantly lower risk of secondary graft failure through 10 years.
01 Sep 2024·CORNEA
Reply
Letter
Author: Price, Marianne O ; Price, Marianne O. ; Price, Francis W. ; Wileman, Justin M ; Price, Francis W ; Wileman, Justin M.
01 Aug 2024·Cornea
Prospective Assessment of Loteprednol Etabonate 0.25% for Prevention of Immunologic Rejection After Descemet Membrane Endothelial Keratoplasty in Eyes With Fuchs Dystrophy
Article
Author: Feng, Matthew T. ; Price, Marianne O. ; Gang, Anjulie ; Price, Francis W.
Purpose::
The purpose of this study was to assess off-label use of loteprednol etabonate 0.25% ophthalmic suspension for prevention of immunologic rejection after Descemet membrane endothelial keratoplasty (DMEK).
Methods::
This prospective, open-label study enrolled 70 eyes of 70 participants without preexisting glaucoma 1 month after DMEK. Participants used topical loteprednol 0.25% 4 times daily for 2 months, tapered by 1 drop/month to once daily use, and continued use through 1 year after DMEK. Main outcomes were rate of intraocular pressure (IOP) elevation (defined as a relative increase of ≥10 mm Hg over the pretransplant IOP) and rate of initial allograft rejection episodes. The results were compared with historical data using the log-rank test.
Results::
All participants had Fuchs dystrophy, and 40 of 70 (57%) were female. None (0%) experienced an immunologic graft rejection episode, matching the previously reported efficacy of prednisolone acetate 1% suspension and loteprednol 0.5% gel (both 0% incidence). One study eye developed IOP elevation 3 months after DMEK (cumulative risk 1.5%). Compared with historical data, this was similar to the risk with loteprednol 0.5% gel (4%, P = 0.36) and significantly lower than the risk with prednisolone 1% suspension (18%, P = 0.0025). Two participants (3%) complained of instillation site discomfort, consistent with the 5% rate reported on package labeling.
Conclusions::
Loteprednol 0.25% suspension, approved for short-term treatment of dry eyes, effectively prevented immunologic rejection episodes with minimal risk of IOP elevation when used from 1 month until 12 months after DMEK in patients without preexisting glaucoma.
1
News (Medical) associated with Cornea Research Foundation of America , Inc.26 Jan 2021
According to the WHO, as of October 2020, globally at least 1 billion people are suffering from near or far vision impairment. The commercialization scale of corneal implants market is likely to rise along a progressive path in the coming years. There is a growing need for minimally invasive eye surgical solutions as the conventional treatment procedures have proven to be extremely risky due to the complexity involved in it.
Effective interventions, like eye examinations and artificial cornea implant procedures, that prevent and treat eye-infections that impact the vision along with the rise in corneal disease incidences have positively influenced the demand for corneal implants. Efforts undertaken by the governments and respective authorities to impart knowledge among the people regarding the need to maintain eye-health has supported the need for upgraded, safe, and reliable treatments.
For instance, the Healthy People 2020 Vision initiated by the U.S. government aims at enhancing visual health by reducing visual impairment and blindness across the nation through timely treatment, early detection, and rehabilitation. As per reports, corneal implants market share is likely to cross USD 500 million in terms of total annual remuneration through 2025. Mentioned below are some of the integral factors likely to impact the corneal implants market size in the coming years.
High geriatric population
An increase in the elderly population especially in emerging countries such as India, China, Japan, Brazil, and Mexico is one of the leading factors behind the need for corneal implants. Most of these people suffer from chronic eye disorders. As per the National Eye Institute, nearly 2.1 million elderly people across the U.S. have age-related macular degeneration.
In the U.S. and Germany, the aged population suffering from diabetes has a high prevalence of diabetic retinopathy. This provides considerable opportunities for corneal implants providers since the products considerably bolsters access to effective treatment.
Growing establishment of eye clinics
An increase in the establishment of specialized eye clinics in both developed, as well as developing nations, has ensured the easy availability of corneal implant solutions. These clinics provide a specialized eye-disease diagnosis as they are well equipped with the latest and necessary medical equipment.
However, certain eye clinics are not self-sufficient to carry out surgeries as well as non-invasive transplant processes owing to financial constraints. Physicians as well as eye-specialists that are working in these clinics refer patients to hospitals that have well-equipped technologies and have the ability to carry out surgical procedures.
Adoption of artificial corneal implants
The introduction of artificial corneal implants has gained considerable recognition over the years as they are highly preferred by patients that cannot tolerate human donor cornea. As per the Cornea Research Foundation of America, nearly 10 million people go through corneal blindness globally of which only 100,000 corneal implant procedures gain access to human donor tissue. The existing crisis of human donor tissue has amplified the demand for artificial corneal implants.
To access sample pages of this report titled, “Corneal Implants Market Size By Tissue Type (Human Donor, Artificial Cornea), By Transplant Type (Anterior Lamellar Keratoplasty, Endothelial Lamellar Keratoplasty, Penetrating Keratoplasty), By Condition (Fungal Keratitis, Fuchs Dystrophy, Keratoconus), By End-use (Hospitals, Eye Clinics, Ambulatory Surgical Centers), Industry Analysis Report, Regional Outlook, Condition Potential, Competitive Market Share & Forecast, 2019 – 2025” in detail along with the table of contents, please click on the link below
North America is a strong market
Regionally speaking, North America has emerged as a prominent consumer of corneal implants and accounted for nearly 60% of the global revenue share during the year 2018. Developments in the regional corneal implants market may be attributed to the escalating geriatric population that suffers from severe eye infections and require corneal implants in the process of treatment. People suffering from keratoconus and Fuchs’ Dystrophy have showcased an immense need for minimally invasive corneal implant solutions.
As per the European Blind Union, there are nearly 30 million partially- sighted and blind people across Europe. Apparently, nearly one in every 30 European experiences sight loss. This showcases a a high need for corneal transplant, paving the way for an increased number of procedures that are being performed annually. The rise in the elderly population and the constantly growing need for advanced medical procedures have magnified the adoption of corneal implants.
Key players in corneal implants market are San Diego Eye Bank, CorNeat Vision, DIPOTEX, Florida Lions Eye Bank, and Presbia.
About Global Market Insights, Inc.
Global Market Insights, Inc., headquartered in Delaware, U.S., is a global market research and consulting service provider, offering syndicated and custom research reports along with growth consulting services. Our business intelligence and industry research reports offer clients with penetrative insights and actionable market data specially designed and presented to aid strategic decision making. These exhaustive reports are designed via a proprietary research methodology and are available for key industries such as chemicals, advanced materials, technology, renewable energy, and biotechnology.
Contact Us:
Arun Hegde
Corporate Sales, USA
Global Market Insights, Inc.
Phone: 1-302-846-7766
Toll Free: 1-888-689-0688
Email: sales@gminsights.com
Website:
100 Deals associated with Cornea Research Foundation of America , Inc.
Login to view more data
100 Translational Medicine associated with Cornea Research Foundation of America , Inc.
Login to view more data
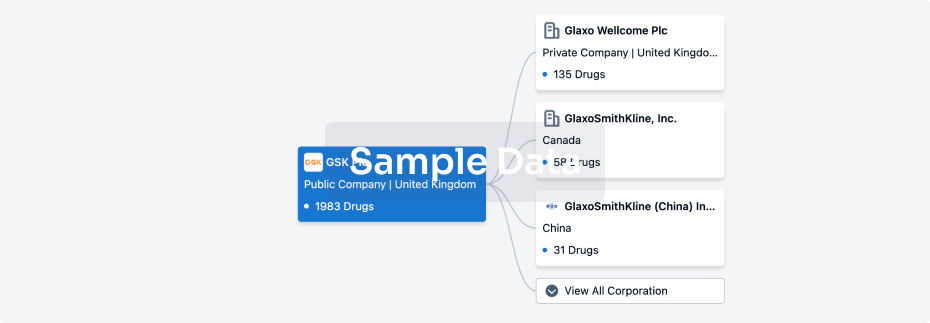
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 07 Dec 2025
No data posted
Login to keep update
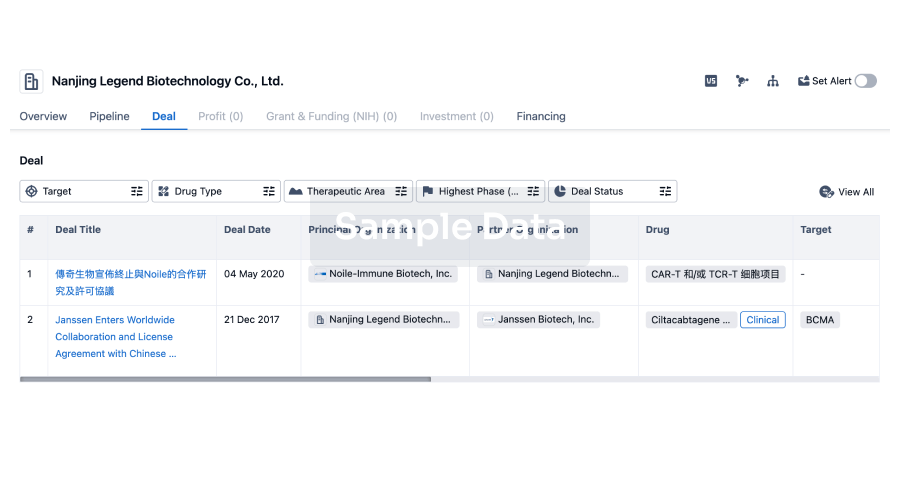
Deal
Boost your decision using our deal data.
login
or
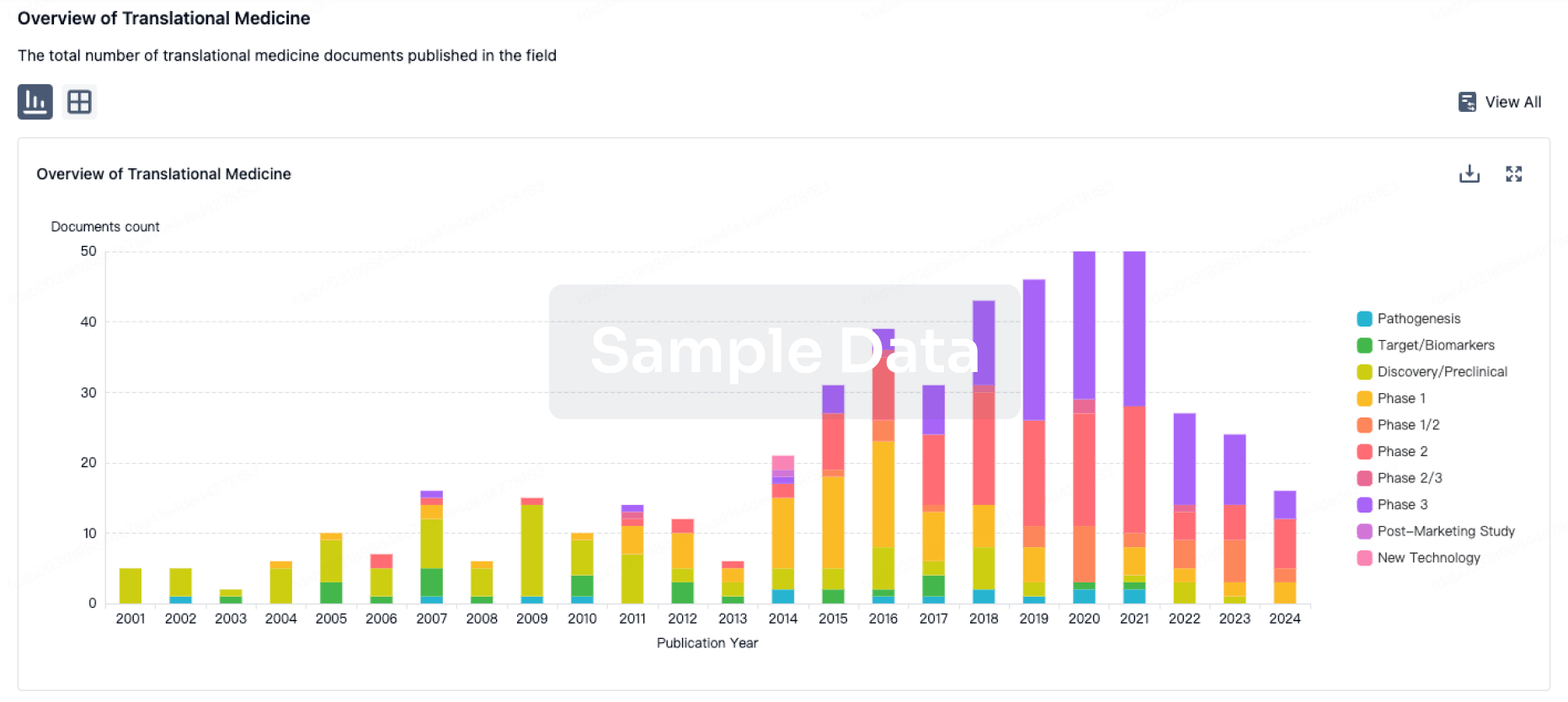
Translational Medicine
Boost your research with our translational medicine data.
login
or
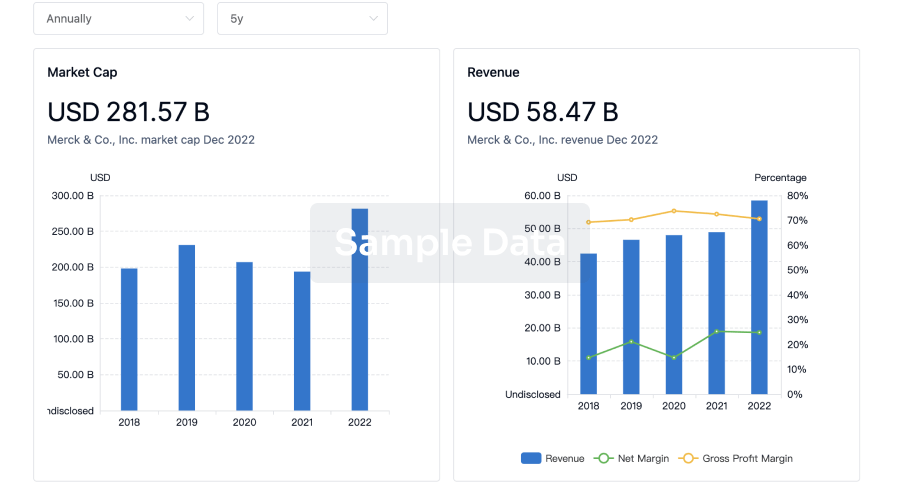
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
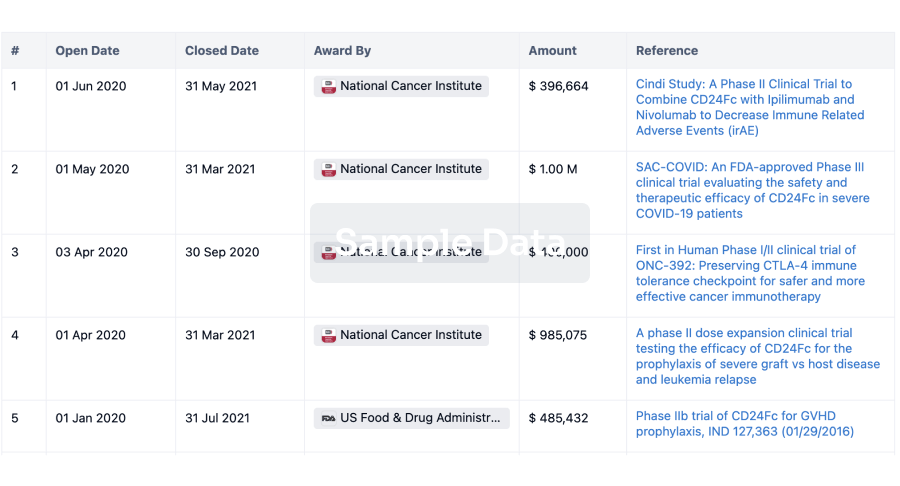
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
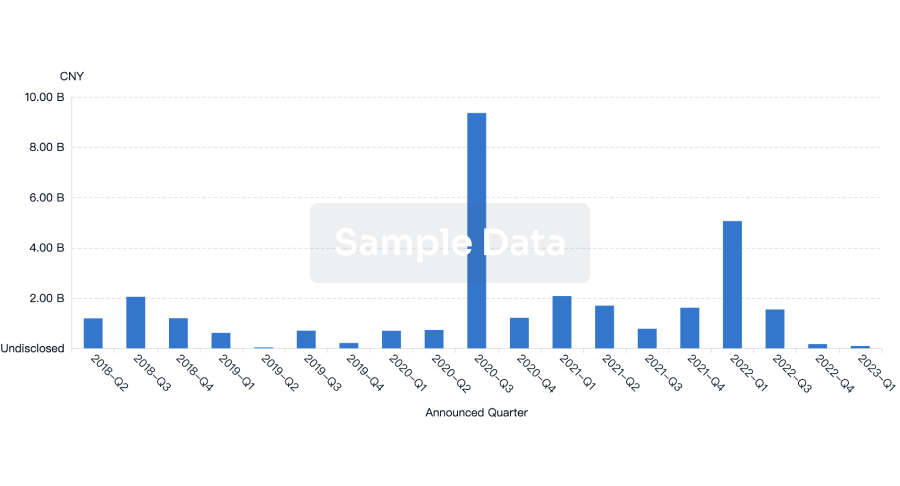
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
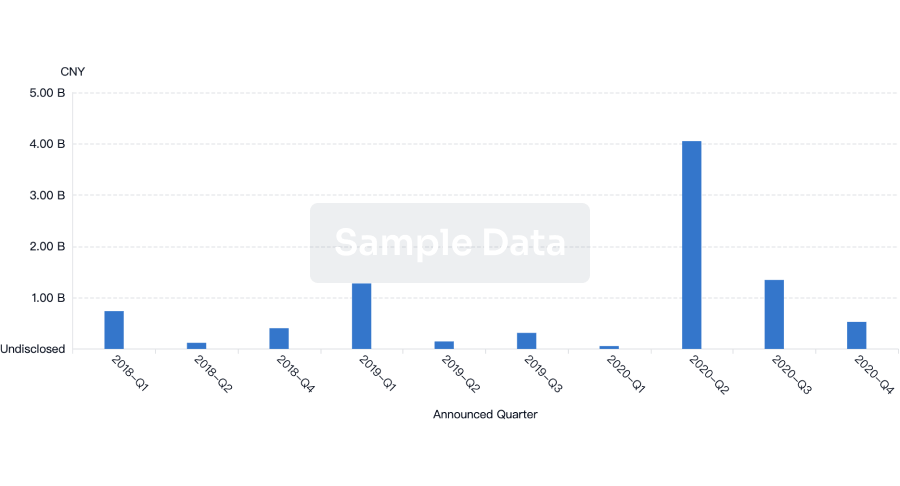
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free