Request Demo
Last update 08 May 2025
Arla Foods Ingredients Group P/S
Last update 08 May 2025
Overview
Related
3
Clinical Trials associated with Arla Foods Ingredients Group P/SNL-OMON53888
Bovine Osteopontin for Elderly Immune Support - BOFEI Study
Start Date13 Feb 2023 |
Sponsor / Collaborator |
NCT04037722
Echocardiographic Changes After Oral Intake of 3-hydroxy Butyrate+Whey in a Human Endotoxemia Model
This study evaluates the cardiovascular effects of adding the ketone body 3-hydroxy butyrate (3-OHB) to whey protein during human endotoxemia. Further, this study compares cardiovascular changes during healthy and catabolic conditions.
Participants will receive isocaloric, isonitrogenous beverages of either whey or 3-OHB+whey in a randomized crossover design during either healthy (overnight fast) or catabolic conditions (inflammation/endotoxemia + 36 h fast and bed rest).
Participants will receive isocaloric, isonitrogenous beverages of either whey or 3-OHB+whey in a randomized crossover design during either healthy (overnight fast) or catabolic conditions (inflammation/endotoxemia + 36 h fast and bed rest).
Start Date17 Jun 2019 |
Sponsor / Collaborator  University of Aarhus University of Aarhus [+2] |
NL-OMON37279
A randomized, placebo-controlled, double blind volunteer study into the effect of milk ingredients on gastroenteritis caused by an attenuated E. coli. - MIRAGE
Start Date02 Oct 2012 |
Sponsor / Collaborator |
100 Clinical Results associated with Arla Foods Ingredients Group P/S
Login to view more data
0 Patents (Medical) associated with Arla Foods Ingredients Group P/S
Login to view more data
73
Literatures (Medical) associated with Arla Foods Ingredients Group P/S22 Apr 2025·Diabetes care
Premeal Whey Protein Lowers Postprandial Blood Glucose in Women With Gestational Diabetes Mellitus: A Randomized, Crossover Clinical Trial.
Article
Author: Kampmann, Ulla ; Knudsen, Janni H ; Ovesen, Per G ; Rittig, Nikolaj ; Wegener, Gregers ; Suder, Louise B ; Brunsgaard, Lise H ; Smedegaard, Stine
01 Apr 2025·The American Journal of Clinical Nutrition
Impact of formula protein quantity and source on infant metabolism: serum, urine, and fecal metabolomes of a randomized controlled study
Article
Author: Hartvigsen, Merete L ; Slupsky, Carolyn M ; He, Xuan ; Hernell, Olle ; Tinghäll Nilsson, Ulrika ; Jacobsen, Lotte N ; Karlsland Åkeson, Pia ; Mishchuk, Darya O ; Lönnerdal, Bo ; Kvistgaard, Anne S
05 Mar 2025·Journal of Agricultural and Food Chemistry
Protein Digestibility and Anti-inflammatory Activity of Processed Whey Protein Ingredients for Infant Formula
Article
Author: Fang, Yajing ; Bering, Stine B. ; Chatterton, Dereck E.W. ; Ye, Yuhui ; Nguyen, Duc Ninh ; Sangild, Per T. ; Bechshøft, Mie Rostved ; Lund, Marianne N. ; Engholm-Keller, Kasper
1
News (Medical) associated with Arla Foods Ingredients Group P/S09 Feb 2021
(Copenhagen, February 9, 2021). Arla Foods Ingredients Group P/S (Arla), a subsidiary of Arla Foods amba, and drug formulation company Zerion ApS (ZERION) have entered into an agreement covering the supply of Arla’s novel and very pure ingredient Lacprodan®BLG that is produced through a patented new technology. ZERION utilises this highly purified protein as a critical component in its patented Dispersome®technology that enables poorly soluble drugs to reach their true therapeutic potential. The agreement marks an important milestone in a year long collaboration between the two companies.
- “Since 2018, we have evaluated a range of protein excipients with our Dispersome®technology and among those, Arla’s Lacprodan® BLG has consistently demonstrated an impressive solubility enhancement of many small molecule drug compounds”, explains ZERION’s Chief Scientific Officer, Dr. Korbinian Löbmann. “As an integral part of the drug evaluation and approval for the Dispersome®formulations, the protein will undergo regulatory assessment by FDA and EMA as a novel pharmaceutical excipient. It is therefore of utmost importance for us to source a protein of the highest quality and purity. Here, we have been very fortunate to work with Arla and to identify Lacprodan® BLG for our applications.”
The agreement between Arla and ZERION sets forth the intention of the parties to complete a full license and supply agreement. Under the final long-term supply agreement, Arla will supply Lacprodan® BLG for use as a pharmaceutical excipient to ZERION.
- “The agreement with Arla confirms our excellent collaboration and represents an important step forward for ZERION to secure the long-term supply of Lacprodan® BLG as an enabling excipient for our Dispersome® technology, says Ole Wiborg, CEO of ZERION. “We are grateful for the support and willingness to explore novel pharmaceutical applications from Arla. We are confident that Lacprodan® BLG can play a pivotal role as a novel excipient in our Dispersome®technology to enable novel drugs and enhance the quality and the safety of medicines for patients.”
Poor drug solubility is a major problem for the pharma industry
ZERION is a pharmaceutical development company specialised in improving the bioavailability of oral drug products by increasing their solubility. The company has pioneered the patented
Dispersome®formulation technologythat enables poorly soluble drugs to reach their true therapeutic potential. Poor drug solubility is one of the biggest challenges hampering the commercial development of novel small molecule drugs. Approximately 90% of all oral drugs in pharmaceutical pipelines do not sufficiently dissolve in the gastrointestinal tract and therefore cannot be absorbed into the circulation and exert their therapeutic effect. Many otherwise promising drug candidates are thus discontinued during early-stage development due to poor bioavailability.
The Dispersome® platform technology
TheDispersome® technology uses Lacprodan® BLG,a patented high quality whey protein, and environmentally friendly by-product from cheese production, to disrupt the drug crystal structure. A unique amorphous composition is formed from the mixture of Lacprodan® BLGand drug molecules resulting in improved drug solubility and bioavailability. The technology enables lowering of the drug dose, resulting in fewer and smaller tablets enhancing patient compliance as well as minimising any side effects. Dispersome®formulations can be produced using standard pharmaceutical equipment.
In addition to its internal product portfolio, ZERION is collaborating with established pharmaceutical companies to assist them in optimising the therapeutic performance of their drug compounds.
Arla Foods Ingredients (AFI)
Arla Foods Ingredients is a global leader in value-added whey solutions that discover and deliver ingredients derived from whey, supporting primarily the food industry with the development and efficient processing of more natural, functional and nutritious foods. Arla Foods Ingredients serves global markets within early life nutrition, medical nutrition, sport nutrition, health foods and other foods and beverage products.
For more information, please visit or contact
Ole Wiborg, CEO
MOB +45 40 96 80 18
For available illustrations/photo materials, please contact Adam Bohr ab@zerion.eu to request materials.
CollaborateSmall molecular drug
100 Deals associated with Arla Foods Ingredients Group P/S
Login to view more data
100 Translational Medicine associated with Arla Foods Ingredients Group P/S
Login to view more data
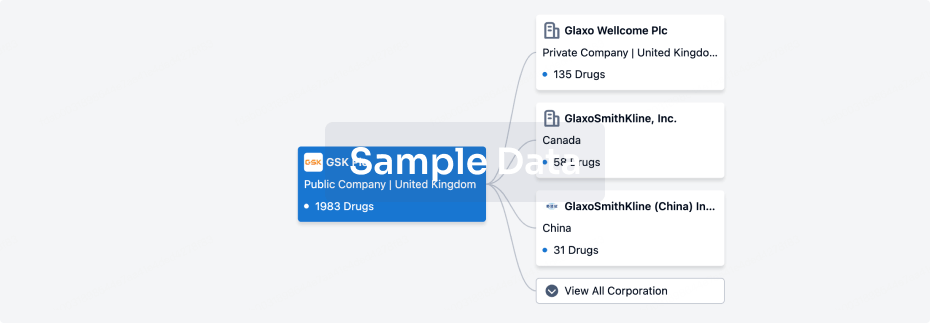
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 11 Sep 2025
No data posted
Login to keep update
Deal
Boost your decision using our deal data.
login
or

Translational Medicine
Boost your research with our translational medicine data.
login
or

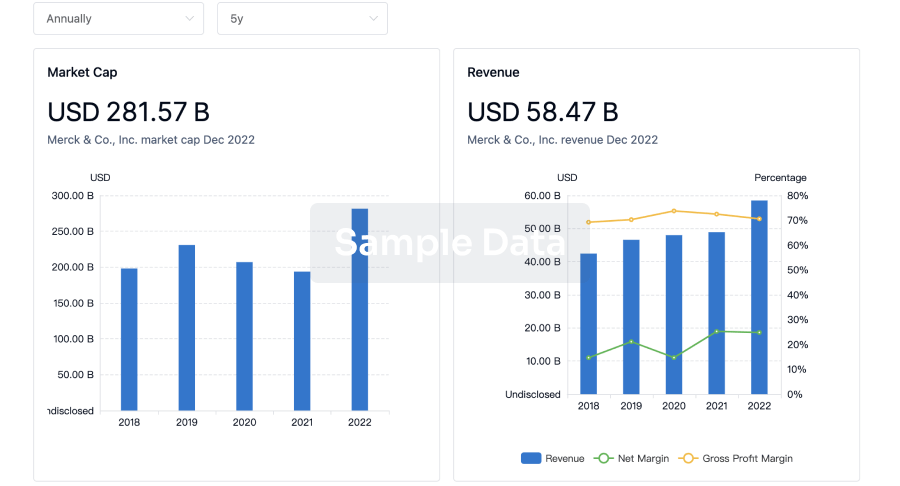
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
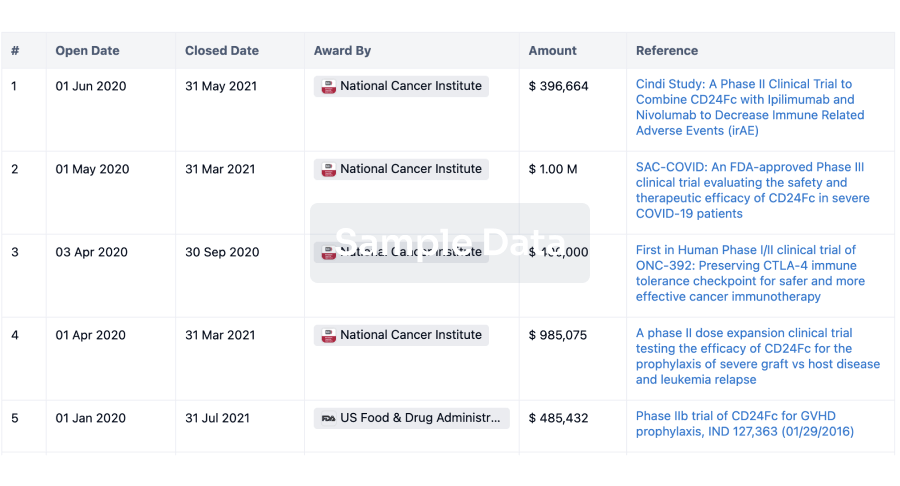
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
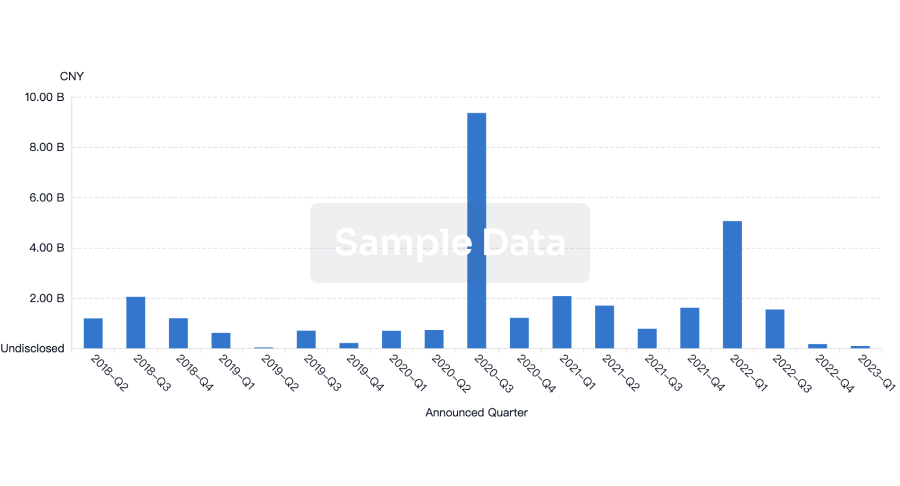
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free