Request Demo
Last update 08 May 2025

Virginia Spine Institute Plc
Last update 08 May 2025
Overview
Related
2
Clinical Trials associated with Virginia Spine Institute PlcNCT01238536
Multicenter Randomized Controlled Trial of Epidural Steroid Injections for Spinal Stenosis in Persons 50 and Older
The broad, long-term objective of this research protocol is to improve the quality of life for patients suffering from lumbar spinal stenosis. This objective will be met by examining the safety and clinical efficacy of epidural steroid injections for treatment of pain associated with lumbar spinal stenosis. This prospective, randomized, double-blind controlled trial (RCT) will test the hypothesis that the effectiveness of epidural steroid injections (ESI) plus local anesthetic (LA) is greater than epidural injections of LA alone in older adults with lumbar spinal stenosis.
Start Date01 Apr 2011 |
Sponsor / Collaborator  University of Washington University of Washington [+11] |
NCT02178605
A Prospective Non-Randomized Investigation Of The Use Of Infuse® (rhBMP-2) In Cervical Arthrodesis
This prospective study will investigate the use of recombinant human bone morphogenetic protein (rhBMP-2) in the current surgical standard of care for cervical spine pathology. Specifically, the outcomes of three forms of cervical fusion will be investigated:
Anterior cervical fusion with rhBMP-2, allograft corticocancellous bone as an interbody device, and anterior cervical plate fixation.
Posterior cervical fusion with rhBMP-2, local bone graft, with or without posterior screw fixation.
A combination of the previous two approaches: a combined anterior-posterior cervical fusion with rhBMP-2.
Anterior cervical fusion with rhBMP-2, allograft corticocancellous bone as an interbody device, and anterior cervical plate fixation.
Posterior cervical fusion with rhBMP-2, local bone graft, with or without posterior screw fixation.
A combination of the previous two approaches: a combined anterior-posterior cervical fusion with rhBMP-2.
Start Date01 Oct 2008 |
Sponsor / Collaborator |
100 Clinical Results associated with Virginia Spine Institute Plc
Login to view more data
0 Patents (Medical) associated with Virginia Spine Institute Plc
Login to view more data
33
Literatures (Medical) associated with Virginia Spine Institute Plc01 Apr 2025·The Spine Journal
Effect of Enhanced Surgical Recovery Program for Thoracolumbar Spine Surgery on Opioid Use, Length of Hospital Stay, and Hospital Readmissions: Evaluation of 51,236 Cases
Article
Author: Bess, Shay ; Orosz, Lindsay D ; Remington, Gina ; Jazini, Ehsan ; Scibelli, Stephen S ; Good, Christopher R ; Luckett, Daniel ; Line, Breton ; Roman, Cecile
01 Mar 2025·The Spine Journal
Performance comparison between Hounsfield units and DXA in predicting lumbar cage subsidence in the degenerative population
Article
Author: Schuler, Thomas C ; Lerebo, Wondwossen T ; Haines, Colin M ; Roy, Rita T ; Good, Christopher R ; Yamout, Tarek ; Allen, Brandon J ; Jazini, Ehsan ; Orosz, Lindsay D ; Schuler, Kirsten A
01 Jun 2024·Journal of Spine Surgery
Anterior cervical hybrid constructs reduce superior adjacent segment burden compared to multilevel anterior cervical discectomy and fusion
Article
Author: Roy, Rita T ; Schuler, Thomas C ; Jazini, Ehsan ; Good, Christopher R ; Schuler, Kirsten A ; Orosz, Lindsay D ; Bhatt, Fenil R ; Grigorian, Julia N ; Haines, Colin M ; Allen, Brandon J
5
News (Medical) associated with Virginia Spine Institute Plc18 Sep 2024
RESTON, Va., Sept. 18, 2024 /PRNewswire/ -- Dr. Ehsan Jazini, renowned spine surgeon at VSI (Virginia Spine Institute), has reached a significant milestone, performing his 100th prodisc® cervical disc replacement surgery at HCA Reston Hospital Center. Dr. Jazini is now the fourth surgeon in the United States to achieve this distinction, further establishing his leadership in advanced spine surgery.
Continue Reading
Dr. Ehsan Jazini celebrates a landmark achievement at VSI (Virginia Spine Institute), receiving the Prodisc Milestone Award for completing 100 successful procedures with the state-of-the-art Cervical Disc Replacement System
Spine Surgeon Dr. Ehsan Jazini successfully completes his 100th prodisc surgery, showcasing the modern surgical techniques that make VSI a leader in motion-preserving spine surgery.
With this milestone, Dr. Jazini has demonstrated his expertise in providing patients suffering from neck conditions with modern surgical options that alleviate pain and preserve natural neck motion. He has successfully performed over 1,000 cervical artificial disc replacement surgeries, utilizing devices from four leading companies. This advanced procedure provides an effective treatment for conditions such as degenerative disc disease, herniated discs, spondylosis, radiculopathy, and myelopathy, offering patients pain relief while preserving natural neck motion.
"Reaching the 100th prodisc surgery milestone is a testament to my commitment to providing the most advanced, motion-preserving solutions in spine care," said Dr. Jazini. "Each procedure is tailored to meet the patient's specific needs, allowing them to regain mobility and live pain-free, active lives. This achievement highlights my dedication to innovation and solidifies my leadership role in modern spine surgery."
Dr. Jazini frequently utilizes the prodisc® C SK and prodisc® C Vivo implants in his surgeries, both offer customized solutions designed to match the patient's unique anatomy. The prodisc system features 84 subtypes and size variations, ensuring optimal fit for the specific level of the treated spine. The implant's ball-and-socket mechanism mirrors the technology used in joint replacements, maintaining the physiological range of motion in the cervical spine.
For more information on Dr. Jazini's expertise and advanced spine care options at VSI, visit or contact +1 703.709.1114.
SOURCE Virginia Spine Institute
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
13 Feb 2024
ADR Spine Welcomes Elite Physicians to Top Doctors in Arthroplasty Program
BEVERLY HILLS, CA / ACCESSWIRE / February 13, 2024 / ADR Spine, a leading authority in spinal care and innovation founded by Dr. Todd H. Lanman, proudly announces the addition of four distinguished physicians to the national Top Doctors in Arthroplasty Program. This program, known for its commitment to excellence in spine surgery and motion preservation, welcomes Dr. K. Brandon Strenge, Dr. Thomas Schuler, Dr. Ehsan Jazini, and Dr. John Peloza to its roster of top doctors.
Dr. K. Brandon Strenge is a fellowship-trained orthopedic spine surgeon specializing in minimally invasive spinal surgery and motion-preserving procedures based in Kentucky. He brings deep experience to spine surgery and is dedicated to patient care. Dr. Strenge is recognized for his advancements in spinal health including disc replacement devices and techniques and has served as a principal investigator for several clinical surgery research trials.
Dr. Thomas Schuler, a leading figure in spine surgery, founded the Virginia Spine Institute in 1992. With dual certification in neurosurgery and orthopedic spine surgery, he's recognized among the top 50 spine surgeons in America and chairs the National Spine Health Foundation's Medical Board. Unique in his experience as both a surgeon and a patient, Dr. Schuler has pioneered advanced techniques, including the first three-level cervical disc replacement in the mid-Atlantic.
Dr. Ehsan Jazini, also dually trained in orthopedic spine surgery and neurosurgery and a surgeon at the Virginia Spine Institute, is at the forefront of innovative spine surgery technologies. Among his notable accomplishments, Dr. Jazini performed the world's first disc replacement spine surgery and first minimally invasive laminectomy with the aid of augmented reality.
Dr. John H. Peloza, of Midwest Orthopedic and Spine Specialists, leads in spine surgery innovation, holding 16 patents and conducting over 24 clinical trials, including cervical and lumbar disc replacements. His focus on minimally invasive surgery, regenerative discogenics, and artificial disc technology ensures safe, top-tier spine care. He ranks among America's Top 50 Spine Surgeons.
The ADR Spine Top Doctors in Arthroplasty Program is designed to identify and highlight the very best providers of motion preservation and motion restoration spine surgery. These four esteemed physicians embody the program's dedication to excellence, innovation, and patient satisfaction.
"We are thrilled to welcome Drs. K. Strenge, Schuler, Jazini, and Peloza to the ADR Spine Top Doctors in Arthroplasty Program," said Dr. Todd H. Lanman, Founder of ADR Spine. "Their expertise and commitment to advancing spinal care align perfectly with our mission to reduce pain and preserve spinal motion in our patients."
New members who meet the rigorous requirements and complete the onboarding process are inducted into the program every quarter. Dr. Jason M. Cuéllar, who worked closely with Dr. Lanman in Los Angeles before establishing a spine surgery practice in Palm Beach, Florida, was the first surgeon accepted into the Top Doctors in Arthroplasty Program last summer.
Contact Information
Brandi Kamenar
PR + Brand Manager
brandi@brandikamenar.com
310-734-6180
SOURCE: ADR Spine
View the original press release on newswire.com.
Executive Change
11 Nov 2022
The prodisc C SK device features a flat endplate design to enable optimised implant positioning for individual patient anatomy, along with a low-pro keel that facilitates immediate fixation and a streamlined keel preparation
The prodisc C SK Cervical TDR device. (Credit: PRNewswire/ Centinel Spine, LLC)
US-based medical device company Centinel Spine has announced the first implantation of its prodisc C SK Cervical Total Disc Replacement (TDR) device.
The prodisc C SK device features a flat endplate design to enable optimised implant positioning for individual patient anatomy.
In addition, it comes with a low-pro keel that facilitates immediate fixation and enables a streamlined keel preparation technique.
The prodisc C SK device incorporates prodisc CORE technology, which is the basis for predictable clinical outcomes after 30 years and over 225,000 implantations worldwide, said the company.
Centinel Spine CEO Steve Murray said: “In spine care, each patient’s circumstances are different, so it is critical to provide surgeons with the ability to address each patient’s unique needs.
“With the release of both the prodisc C Vivo and prodisc C SK devices, we have expanded the options available to surgeons to allow for better matching of the disc to the patient.
“While these two new product releases have been conducted on a limited scale, we have already seen a strong positive response from surgeon partners related to the potential patient benefits.”
Centinel Spine is a medical device company focused on addressing cervical and lumbar spinal disease through anterior surgical access.
The company offers motion-preserving and fusion solutions, including clinically-proven technology platforms for total disc replacement and Integrated Interbody fusion (STALIF).
In July this year, the company secured the US Food and Drug Administration (FDA) approval for the prodisc C Vivo, prodisc C SK, and prodisc C Nova products.
The prodisc C SK system is the second among the three new products to be rolled out, with the company recently announcing the completion of the 100th procedure using its prodisc C Vivo TDR product.
Centinel Spine claimed that it has an extensive offering of cervical TDR solutions to address individual patient anatomy and meet surgeon preference needs.
Virginia Spine Institute orthopaedic spine surgeon Ehsan Jazini said: “I am proud to be the first surgeon to use this innovative technology in the DC metro region.
“As a pioneer working to make disc replacement surgery ultra-customised for each patient, the prodisc C SK and prodisc C Vivo devices provide me the versatility to match the disc to the patient’s anatomy.
“With this advanced proven technology, we can best gain motion preservation and stability as appropriate for each cervical surgery.”
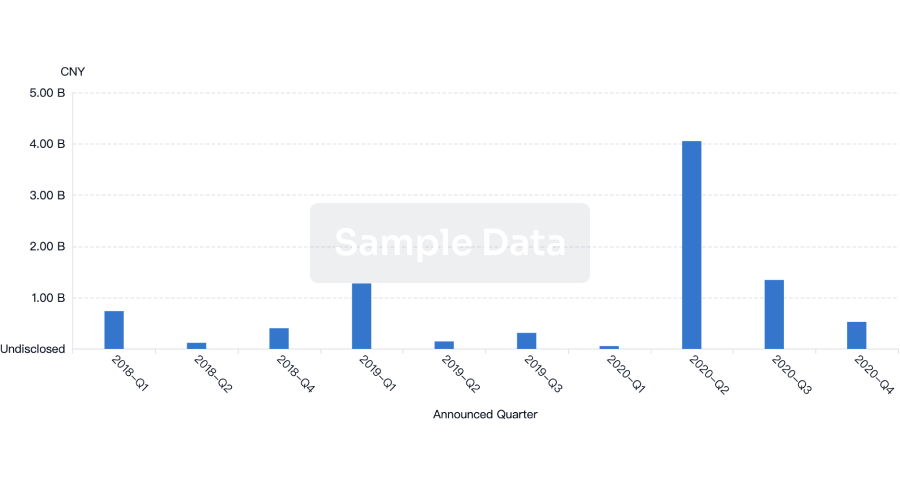
100 Deals associated with Virginia Spine Institute Plc
Login to view more data
100 Translational Medicine associated with Virginia Spine Institute Plc
Login to view more data
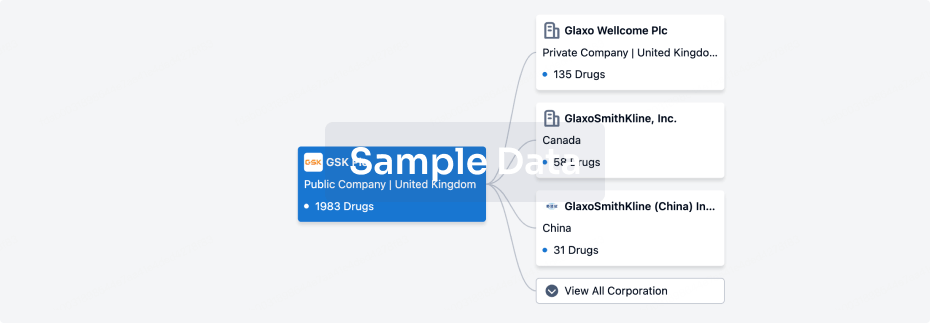
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 18 May 2025
No data posted
Login to keep update
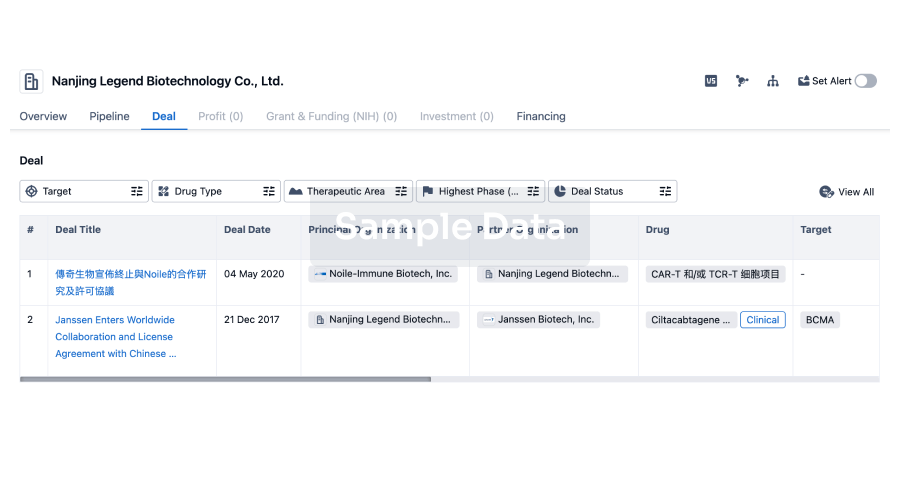
Deal
Boost your decision using our deal data.
login
or
Translational Medicine
Boost your research with our translational medicine data.
login
or

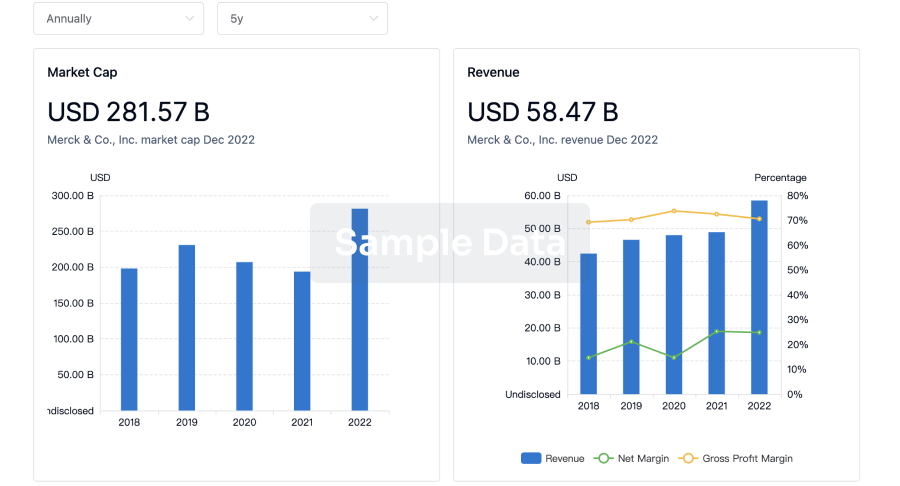
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
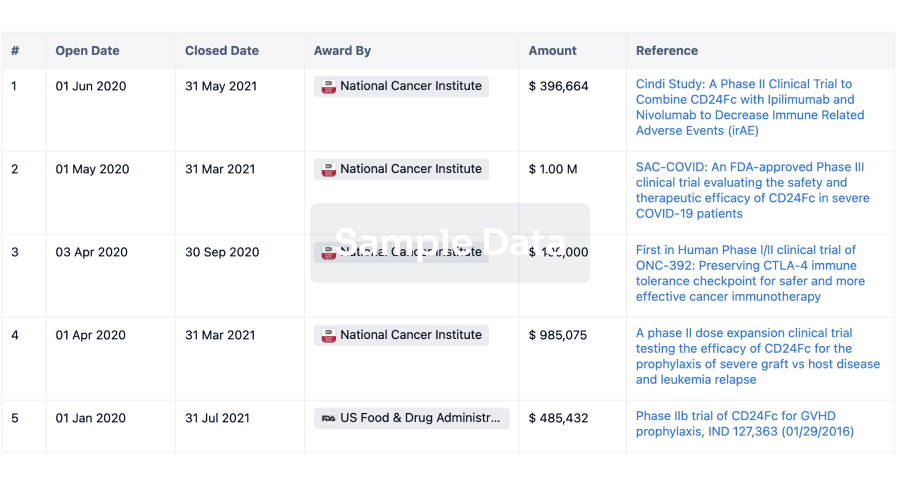
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
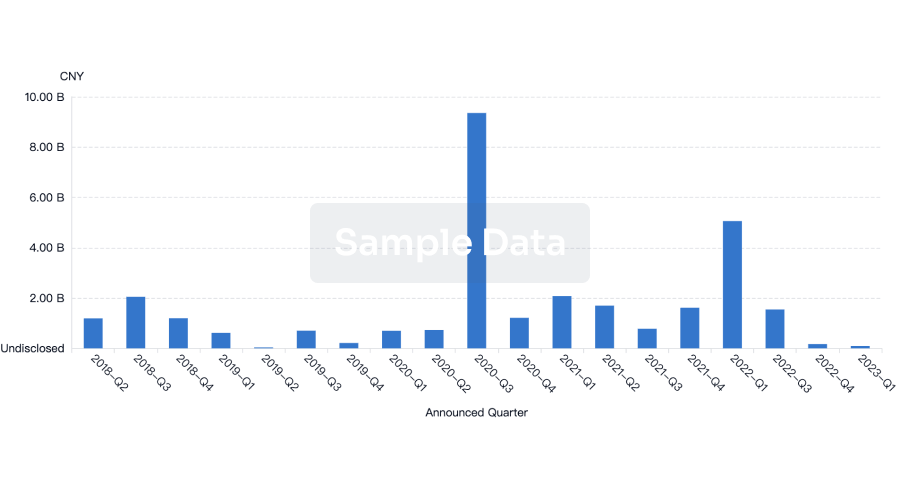
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free