Request Demo
Last update 08 May 2025

JLK, Inc.
Last update 08 May 2025
Overview
Related
2
Clinical Trials associated with JLK, Inc.KCT0009457
Artificial Intelligence-based Large Vessel Occlusion Diagnosis Algorithm Verification: A retrospective, multicenter, confirmatory study to evaluate the safety and effectiveness of JBS-LVO, a brain image detection and diagnostic aid software that evaluates the presence of large vessel occlusion using brain CTA images
Start Date01 Oct 2023 |
Sponsor / Collaborator |
NL-OMON25644
Efficacy of natural eggshell membrane in the alleviation of joint pain associated with osteoarthritis
Start Date08 Sep 2018 |
Sponsor / Collaborator |
100 Clinical Results associated with JLK, Inc.
Login to view more data
0 Patents (Medical) associated with JLK, Inc.
Login to view more data
9
Literatures (Medical) associated with JLK, Inc.01 Feb 2025·Stroke
Abstract WP321: Development of scoring system for predicting recurrent ischemic stroke in patients with atrial fibrillation
Author: Ryu, Wi-sun ; Oh, Mi-Sun ; Bae, Hee-Joon ; Han, Moon-Ku ; Choi, Kangho ; Kang, Chul-Hoo ; Hong, Keun-Sik ; Lee, Jun ; Hong, Jeong-Ho ; Kim, Do Yeon ; Kim, Jae ; LEE, JUNEYOUNG ; LEE, JEONGYOON ; Shin, Dong Ick ; Kim, Wook-joo ; Kim, Joon-Tae ; Kwon, Jee-hyun ; Park, Jong-moo ; Sohn, Sung-il ; Han, Seokgil ; Kang, Kyusik ; Park, Hong-kyun ; Park, Tai ; Lee, Byung-Chul ; Jeong, Han-gil ; Yu, Kyung-Ho ; Lee, Kyungbok ; Park, Hyungjong ; Kwon, Doo Hyuk ; Kim, Dong-Eog ; Guk, Hyung Seok ; Lee, Minwoo ; Choi, Jay Chol ; Cha, Jae-kwan ; Yum, Kyu Sun ; Kim, Dae Hyun ; Lee, Keon-Joo ; Kim, Joonggoo ; Kim, Beom Joon ; Lee, Soo Joo ; Cho, Yong-jin
01 Feb 2025·Stroke
Abstract WP197: Detection and segmentation of hyperdense middle cerebral artery sign on non-contrast CT using artificial intelligence
Author: Ryu, Wi-sun ; Kim, Chi Kyung ; Oh, Kyungmi
01 Feb 2025·Stroke
Abstract TMP59: Artificial Intelligence Improves Detection Sensitivity for Challenging Acute Ischemic Stroke Lesions on Diffusion-weighted Imaging
Author: HA, Sue Young ; Sunwoo, Leonard ; Ryu, Wi-sun ; Kim, Beom Joon ; Jeong, Younbeom
5
News (Medical) associated with JLK, Inc.28 Mar 2025
Dozee bags $8M for global expansion
Dozee is seeking to enter new international markets following its latest fundraising.
The Indian medical device maker raised INR 71.5 crore ($8.3 million) from Temasek Trust's C3H and other investors.
"Beyond the [United States], we are exploring new international markets while broadening our product portfolio to cover the entire continuum of care — from hospitals to transition care and home settings," a company spokesperson said in a statement shared with Mobihealth News.
The company, which offers an AI-powered contactless vital signs monitoring and alert system, raised $6 million in a second Series A funding round in 2023 to kickstart its expansion.
JLK scores 4th Japan PMDA clearance
South Korean medical AI company JLK has announced new regulatory clearance for one of its stroke AI software products.
It received its fourth approval from Japan's Pharmaceuticals and Medical Devices Agency (PMDA) for its MRI FLAIR-based (Fluid-Attenuated Inversion Recovery) software.
The solution analyses, visualises, and measures high-intensity areas in MRI-FLAIR sequence images, which helps in evaluating treatment options for patients with acute ischemic stroke and predicting cognitive decline and dementia risk.
The company received its last PMDA approval for its non-contrast CT stroke AI software in February.
Coreline Soft secures new US FDA, Korea MFDS approvals
Another medical AI company, Coreline Soft, has also obtained new regulatory approvals in South Korea and the United States.
It received its 11th 510(k) certification from the United States Food and Drug Administration for its upgraded flagship medical image analysis software. The software, now dubbed AVIEW 2.0features an optimised user interface and enhanced accessibility, security, stability, and communication function.
The company was also awarded Class 3 approval from South Korea's Ministry of Food and Drug Safety for AVIEW LCS, its AI-based software for predicting the malignancy of pulmonary nodules.
Health genAI platform bags $500,000
Singaporean startup FlocCare has recently raised $500,000 in investment from DTVP, SDTA Ventures and other angel investors.
Founded in 2023, the company develops large language models for generating personalised medical information for hospitals, healthcare professionals, and patients. It claims its models are "50 times faster, fact-checked, scalable and regulatory-compliant."
In a press statement, FlocCare said it would use its fresh funds to expand its genAI models to more disease categories, including cardiovascular diseases, chronic kidney disease, women's health, and oncology.
It also plans to introduce its AI models in the United Arab Emirates, as well as onboard new team members.
Drug Approval
07 Mar 2025
Chulalongkorn University engineer develops hybrid wheelchair, wearable robot
A wheelchair that also serves as a wearable exoskeleton for people with mobility issues has been developed in Thailand.
The hybrid robot prototype allows its user to leave the wheelchair to stand and walk using an exoskeleton.
"The lower leg can change mode between sitting and walking using a motor to help with the movement of the hip and knee joints. The ankle joint is a free joint with no drive. The left and right wheels can be retracted to the lower leg area to transform into a walking posture or get over obstacles," explained Dr Ronnapee Chaichawarat, an associate professor of the International School of Engineering at Chulalongkorn University.
Dr Chaichawarat, who developed the hybrid robot with funding from the National Research Council of Thailand, is now building a second prototype with improved stability in sitting, standing, and walking. He is also preparing for its clinical trial.
Heuron expands to Japan
Heuron from South Korea has started supplying its medical imaging AI to Japan.
The company recently signed an exclusive deal with remote diagnostic imaging provider, Doctor Net, to distribute and sell its non-contrast CT-based acute stroke triage AI software across healthcare settings in Japan.
They will also collaborate to obtain local regulatory approval for the AI solution, which they target by yearend.
Respiree receives expanded HSA clearance
Singaporean startup Respiree has obtained clearance from Singapore's Health Sciences Authority for the expanded use of its wearable device to children.
Its device measures the respiration of patients with cardio-pulmonary diseases such as COPD and congestive heart failure.
The clearance is also for the extension of its software, which now features automated alerts and symptom questionnaire generation and integrates with EMR systems. It also has API plugins that enable EMR interoperability.
Respiree, which has been approved in Australia, Europe, and the United States, is looking to secure more regulatory clearances for its wearable device and AI-powered software-as-a-medical-device across Asia-Pacific.
JLK secures more FDA approvals
Korean medical imaging AI company JLK has received its sixth and seventh United States Food and Drug Administration approvals.
It obtained 510(k) clearances for its integrated medical image management and analysis platform and AI software for detecting subdural haemorrhage in CT scans.
Most recently in January, JLK secured the US FDA's nod for its AI software supporting intracerebral hemorrhage diagnosis.
License out/in
18 Oct 2024
Biofourmis founder launches health LMM startup
Over a year after leaving biotechnology unicorn Biofourmis, ex-CEO and founder Kuldeep Singh Rajput recently announced that he set up a new health tech company focused on generative AI.
In a LinkedIn post, he shared that his newly founded startup, OutcomesAI, has partnered with SingHealth to deploy its large multi-modal model (LMM) called Glia, which allows organisations to build clinician companion AI.
National Heart Centre Singapore and National Cancer Centre Singapore were identified as the first sites of the LMM integration.
JLK bags 510(k) for CT perfusion AI
South Korean medical AI company JLK has obtained another regulatory approval in the United States for one of its stroke AI offerings.
The company received its third 510(k) clearance from the US Food and Drug Administration for JLK-CTP, which uses AI to automatically identify the centre of cerebral infarction and the area of cerebral hypoperfusion in brain CT perfusion images.
JLK received its first 510(k) in June for its MRI-based prostate analysis AI software, then a second one for another stroke AI solution that specifically detects large vessel occlusion in brain CT scans.
Korea OKs Heuron's Parkinson's disease AI
Fellow Korean medical imaging AI company, Heuron, also recently received regulatory approval from the South Korean Ministry of Food and Drug Safety.
According to a press statement, its AI-powered software HeuronNM identifies and quantifies neuromelanin – a key biomarker of Parkinson's disease – in brain 3D MRI images.
Meanwhile, Heuron is currently working to secure FDA approvals in Thailand for its range of AI solutions following its expansion there in August.
Wadhwani AI backs AIIMS
Indian non-profit Wadhwani Institute for Artificial Intelligence (Wadhwani AI) has been tapped to support the All India Institute of Medical Sciences in New Delhi in its healthcare AI integration projects.
AIIMS was recently designated as one of India's "AI centres of excellence" under the government's Make AI in India, Make AI Work for India initiative, in which healthcare is one of the priority areas.
As a partner, Wadhwani AI will be deploying its AI solutions that support the diagnosis of chest conditions and diabetic retinopathy.
The Indian government has pledged to invest over $110 million in supporting the AI COEs over the next four years.
NUS Medicine establishes digital health accelerator
The Yong Loo Lin School of Medicine of the National University of Singapore (NUS Medicine) has recently launched an accelerator programme for digital health startups, including those developing AI solutions in mental health and hospital administration.
A collaboration with 22Health Ventures, the Digital Accelerator Programme of the NUS Medicine Digital Advanced Technology Accelerator aims to support startups from conception through global expansion.
The cohort includes 2Strands, which develops blood-based cancer recurrence monitoring tests; Health BETA, which offers genetic tests and digital therapeutics for personalised health monitoring; HealthBridge AI, which is currently testing its clinical product for streamlining administrative tasks; Marymount Lab, which provides patient engagement software for preventive health; and TenangAI, which offers an AI-driven solution to support youth mental health.
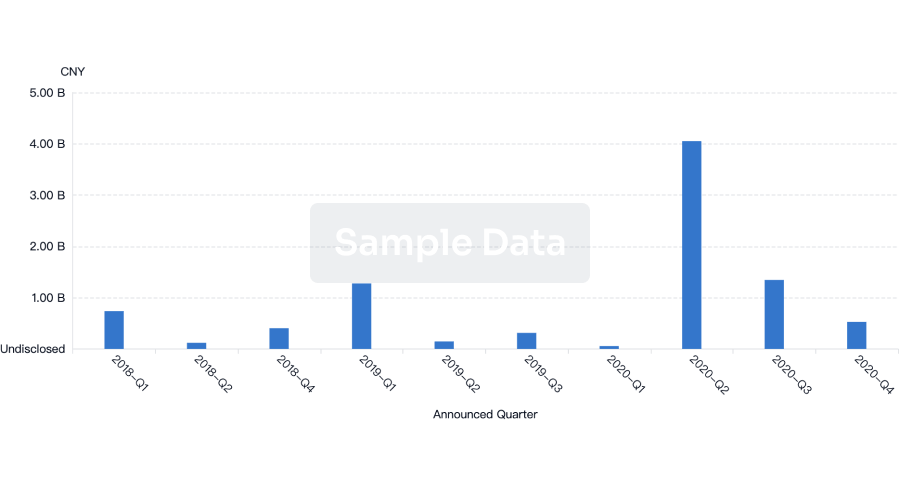
100 Deals associated with JLK, Inc.
Login to view more data
100 Translational Medicine associated with JLK, Inc.
Login to view more data
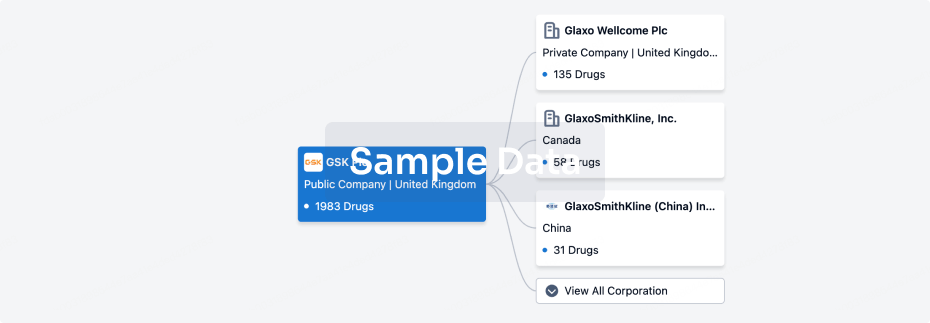
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 28 Aug 2025
No data posted
Login to keep update
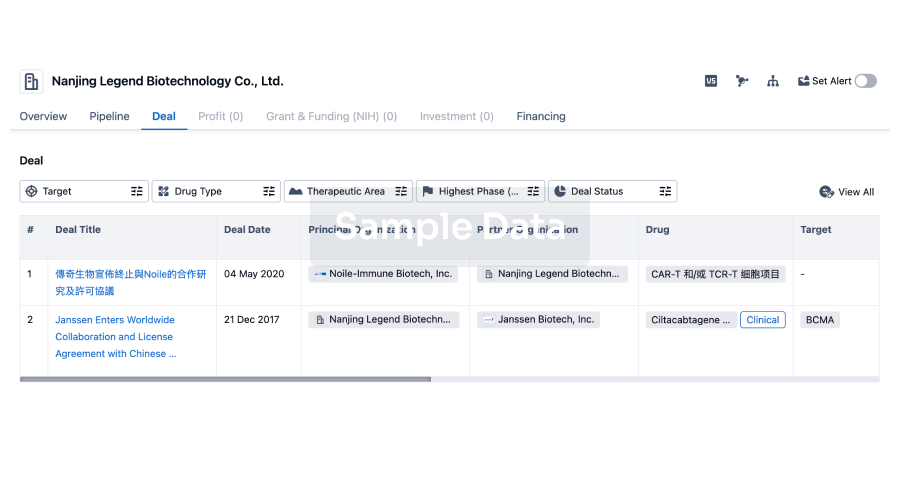
Deal
Boost your decision using our deal data.
login
or
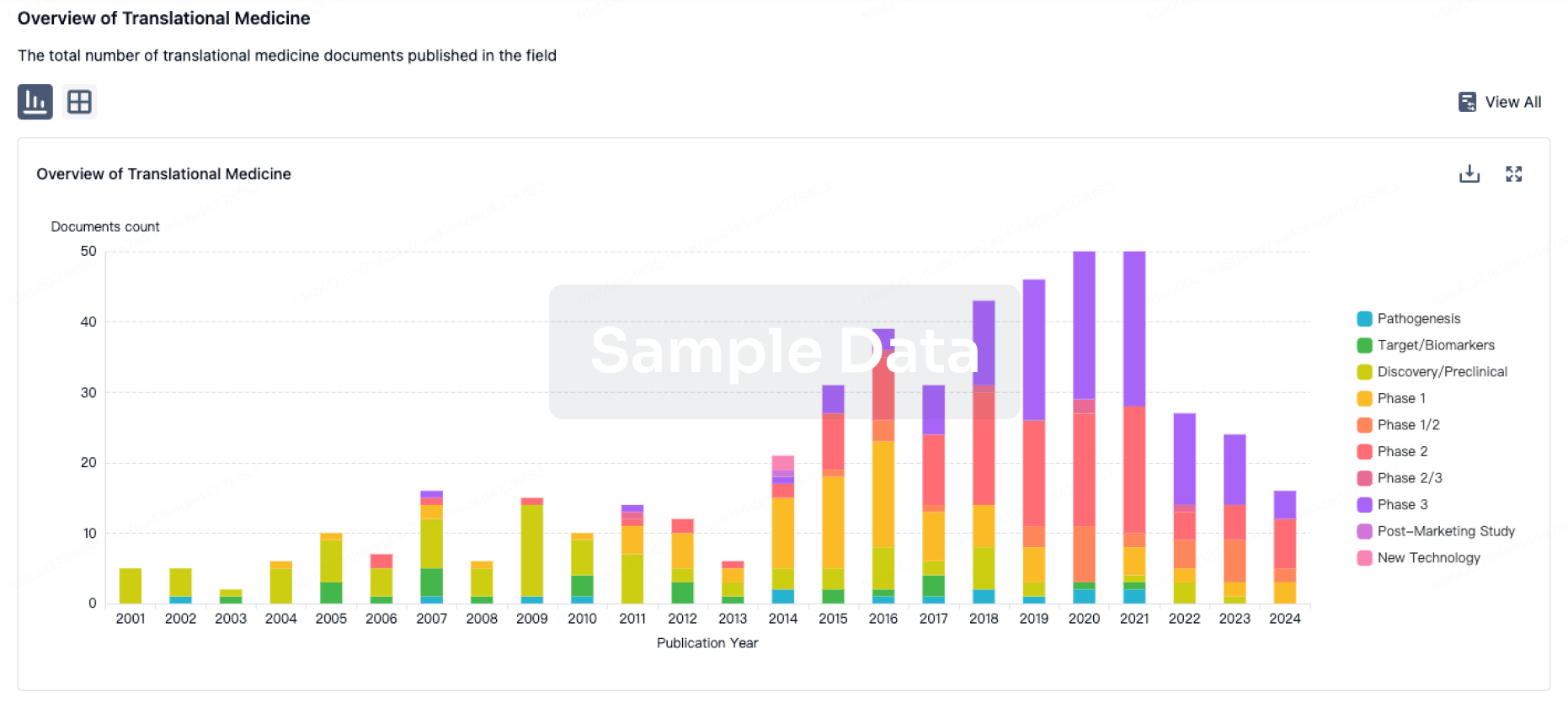
Translational Medicine
Boost your research with our translational medicine data.
login
or
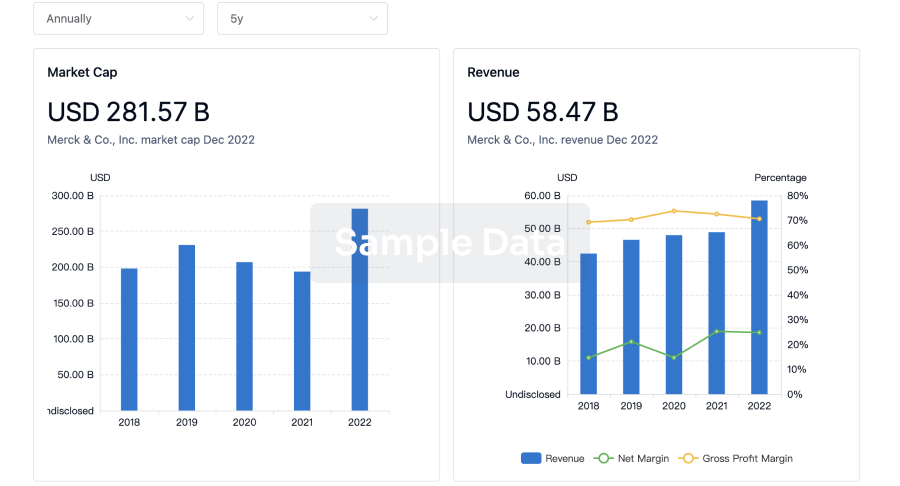
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
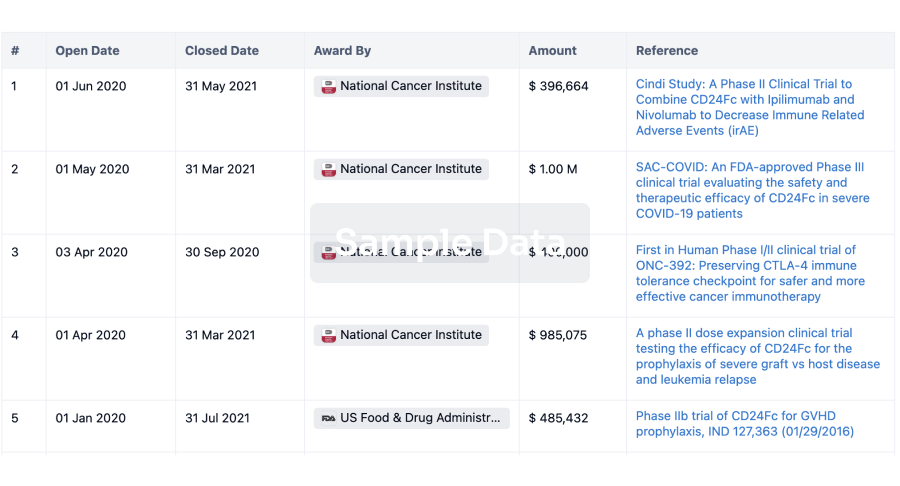
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
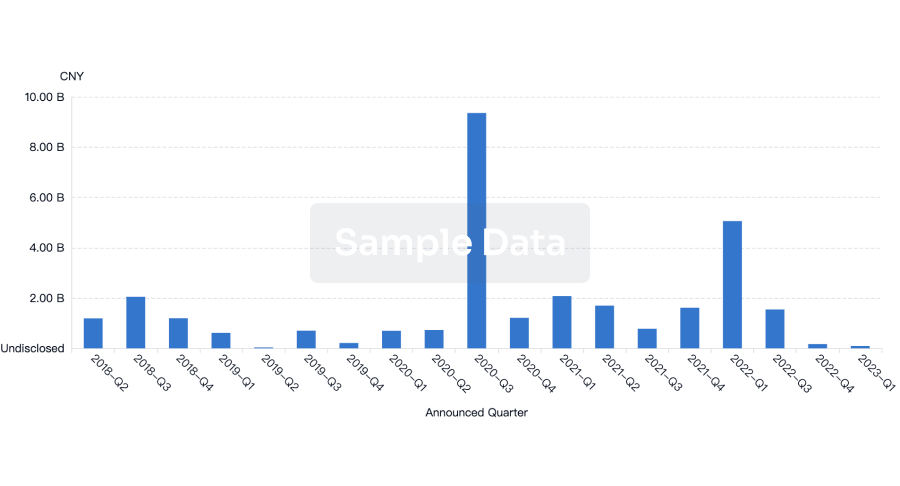
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free