Request Demo
Last update 23 Jan 2025
Military Infectious Diseases Research Program (MIDRP)
Last update 23 Jan 2025
Overview
Related
2
Drugs associated with Military Infectious Diseases Research Program (MIDRP)Target- |
Mechanism Immunostimulants |
Active Org.- |
Originator Org. |
Active Indication- |
Drug Highest PhaseDiscontinued |
First Approval Ctry. / Loc.- |
First Approval Date- |
Target- |
Mechanism Immunostimulants |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhasePending |
First Approval Ctry. / Loc.- |
First Approval Date- |
5
Clinical Trials associated with Military Infectious Diseases Research Program (MIDRP)NCT02174978
Phase 1 Clinical Trial With Controlled Human Malaria Infection (CHMI) Open-label Dose Safety, Reactogenicity, Immunogenicity, and Efficacy of the Vaccine Candidate Plasmodium Falciparum Malaria Protein (FMP012), Administered Intramuscularly With AS01B Adjuvant System in Healthy Malaria-Naïve Adults
The proposed study is a Phase 1 study with controlled human malaria infection (CHMI) designed primarily to evaluate the safety of the FMP012 combined with AS01B adjuvant system. AS01B is a proprietary current good manufacturing practices (cGMP) grade adjuvant manufactured by GlaxoSmithKline (GSK) Biologicals. It is a formulation based on liposomes mixed with the immunostimulants monophosphoryl lipid (MPL) and Quillaja saponaria (QS)-21. The immunogenicity and efficacy of this new candidate vaccine will be evaluated in addition to safety.
Start Date01 Aug 2014 |
Sponsor / Collaborator |
NCT02215707
A Clinical Trial of the PfSPZ Vaccine Administered by Direct Venous Inoculation in Healthy Malaria-Naïve Adults: Heterologous vs. Homologous Controlled Human Malaria Infection and Reduction in Number of Doses
This is an open-label evaluation of the safety, tolerability immunogenicity and efficacy of the PfSPZ Vaccine administered by Direct Venous Inoculation (DVI) in healthy, malaria-naïve subjects. There will be 3 groups and a total of 69 subjects (45 immunized subjects and 24 infectivity controls).
Start Date01 Jun 2014 |
Sponsor / Collaborator  Sanaria, Inc. Sanaria, Inc. [+3] |
NCT00459615
A Phase II, Randomized, Open-Label, Dose-Ranging Study of Intravenous Artesunate Therapy for the Treatment of Acute, Uncomplicated Plasmodium Falciparum Malaria.
The purpose of this study is to compare four regimens using US FDA GMP intravenous artesunate for the treatment of uncomplicated Plasmodium falciparum malaria to identify the most effective treatment regimen as determined by rapidity of parasite clearance by microscopy.
Start Date01 Apr 2007 |
Sponsor / Collaborator |
100 Clinical Results associated with Military Infectious Diseases Research Program (MIDRP)
Login to view more data
0 Patents (Medical) associated with Military Infectious Diseases Research Program (MIDRP)
Login to view more data
3
News (Medical) associated with Military Infectious Diseases Research Program (MIDRP)22 Mar 2023
For mosquito-borne diseases such as dengue fever, the abundance of the insects in places where people gather has long served as the main barometer for infection risk. A new study, however, suggests that the number of 'hidden' infections tied to a place, or cases of infected people who show no symptoms, is the key indicator for dengue risk.
For mosquito-borne diseases such as dengue fever, the abundance of the insects in places where people gather has long served as the main barometer for infection risk. A new study, however, suggests that the number of "hidden" infections tied to a place, or cases of infected people who show no symptoms, is the key indicator for dengue risk.
PNAS Nexus published the research led by scientists at Emory University, which drew from six years of data collected in the Amazonian city of Iquitos, Peru.
The results found that 8% of human activity spaces in the study accounted for more than half of infections during a dengue outbreak. And these "super spreader" spaces were associated with a predominance of asymptomatic cases, or 74% of all infections.
"Our findings show that any public health intervention that focuses on responding to symptomatic cases of dengue is going to fail to control an outbreak," says Gonzalo Vazquez-Prokopec, first author of the study and an Emory associate professor of environmental sciences. "Symptomatic cases represent only the tip of the iceberg."
Co-authors of the research include Uriel Kitron, Emory professor of environmental sciences; Lance Waller, professor of biostatistics and bioinformatics at Emory's Rollins School of Public Health; and scientists from University of California-Davis, Tulane University, San Diego State University, University of Notre Dame, North Carolina State University and the U.S. Naval Medical Research Unit in Lima, Peru.
Dengue fever is caused by a virus transmitted by the bite of a female Aedes aegypti mosquito. When the insect takes a blood meal from a human infected with dengue, the virus begins replicating within the mosquito. The virus may then spread to another person that the mosquito bites days later.
This species of mosquito feeds exclusively on human blood, has a limited flight range of about 100 meters and thrives in sprawling urban areas of the tropics and subtropics. Its preferred habitat is inside homes, where it rests on the backs of furniture and at the bases of walls. Even the little bit of water held by an upturned bottle cap can serve as a nursery for its larvae.
Vazquez-Prokopec is pioneering new mosquito-borne disease interventions, including tapping spatiotemporal data to track, predict and control outbreaks of pathogens transmitted by Aedes aegypti. The mosquito spreads the Zika, chikungunya and yellow fever viruses in addition to dengue.
Around 500,000 cases of dengue occur annually around the world, according to the World Health Organization. The disease is caused by four distinct but closely related serotypes of the dengue virus. Infected people may have some immunity that prevents them from experiencing any noticeable effects while others may be severely debilitated for a week or more by symptoms such as extreme aches and pains, vomiting and rashes. Dengue hemorrhagic fever, the most severe form of the disease, causes an estimated 25,000 deaths annually worldwide.
Iquitos, a city of nearly 500,000 people on the edge of the Amazon rainforest in Peru, is a dengue hotspot. For more than a decade, Vazquez-Prokopec and colleagues have mapped patterns of human mobility and dengue spread in Iquitos.
"For diseases that are directly spread from one person to another, like COVID-19, what matters is who you were near," he says. "But in the case of dengue, what matters most is where you went."
For the current study, the researchers wanted to determine the role of asymptomatic cases. People without symptoms may continue to go about their daily routines, unknowingly infecting any mosquitoes that bite them, which can then later spread the virus to more people.
The study involved 4,600 people in two different neighborhoods. They were surveyed three times a week about their mobility. This data was used to map "activity spaces," such as residences, churches and schools.
The study participants were also regularly surveilled to determine if they experienced any dengue symptoms. Blood analyses confirmed a total of 257 symptomatic cases of dengue during the six-year study period. That led to investigations of other participants whose activity spaces overlapped with the symptomatic cases. More than 2,000 of these location-based contacts were confirmed by blood tests to have dengue infections and more than half of them reported not having any noticeable symptoms.
The results pinpointed the role of asymptomatic "super spreaders" in a dengue outbreak. A small number of the activity spaces, or 8%, were linked to more than half of the infections and most of the cases associated with those places were asymptomatic.
The comprehensive, one-of-a-kind study broke down the virus infections by serotype and measured the amount of mosquitoes in the activity spaces.
"We found that the mosquito numbers in a location alone is not a predictor of the risk of infection," Vazquez-Prokopec says.
Instead, risk prediction for a location requires a cascade of circumstances: a high number of asymptomatic cases frequenting the location combined with high levels of mosquitos and high numbers of people who are not immune to the particular serotype of dengue virus that is circulating.
"That's the complicated nature of this virus," Vazquez-Prokopec says. "We have underestimated the role of asymptomatic cases in spreading dengue."
Generally, about 50 to 70% of dengue cases are asymptomatic, making detection by public health officials impractical, and the current study reveals that asymptomatic cases are tied to a third of transmission.
"The lesson is that we need to focus on prevention of dengue outbreaks," Vazquez-Prokopec says. "The interventions for dengue for decades have been reactive. Simply reacting by closing a net around reported cases of the disease, however, will fail to contain an outbreak because that's missing the super spreaders."
The study was funded by the U.S. National Institute of Allergy and Infectious Diseases, Bill and Melinda Gates Foundation, University of Notre Dame, Defense Threat Reduction Agency, Military Infectious Disease Research Program and the Armed Forces Health Surveillance Branch Global Emerging Infections Systems research program.
Clinical Result
10 Aug 2022
Urinary tract infections are common, yet are increasingly tough to treat because the bacteria that cause them are becoming resistant to many antibiotics. Now researchers report a new molecule that inhibits drug-resistant bacteria in lab experiments, as well as in mice with pneumonia and urinary tract infections. The researchers say that this compound, fabimycin, could one day be used to treat challenging infections in humans.
Urinary tract infections are common, yet are increasingly tough to treat because the bacteria that cause them are becoming resistant to many antibiotics. Now, in ACS Central Science, researchers report a new molecule that inhibits drug-resistant bacteria in lab experiments, as well as in mice with pneumonia and urinary tract infections. The researchers say that this compound, fabimycin, could one day be used to treat challenging infections in humans.
Gram-negative bacteria are a class of microbes that infect millions of people worldwide, according to the U.S. Centers for Disease Control and Prevention, causing conditions such as pneumonia, urinary tract infections and bloodstream infections. These bacteria are especially difficult to treat because they have strong defense systems - tough cell walls that keep most antibiotics out and pumps that efficiently remove those antibiotics that get inside. The microbes can also mutate to evade multiple drugs. Furthermore, treatments that do work aren't very specific, eradicating many kinds of bacteria, including those that are beneficial. So, Paul Hergenrother and colleagues wanted to design a drug that could infiltrate the defenses of gram-negative bacteria and treat infections, while leaving other helpful microbes intact.
The team started with an antibiotic that was active against gram-positive bacteria and made a series of structural modifications that they believed would allow it to act against gram-negative strains. One of the modified compounds, dubbed fabimycin, proved potent against more than 300 drug-resistant clinical isolates, while remaining relatively inactive toward certain gram-positive pathogens and some typically harmless bacteria that live in or on the human body. In addition, the new molecule reduced the amount of drug-resistant bacteria in mice with pneumonia or urinary tract infections to pre-infection levels or below, performing as well as or better than existing antibiotics at similar doses. The researchers say the results show that fabimycin could one day be an effective treatment for stubborn infections.
The authors acknowledge funding from the University of Illinois, the National Institutes of Health, the National Science Foundation, the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator, Anita and Josh Bekenstein, Biomedical Advanced Research and Development Authority, Military Infectious Diseases Research Program and the Roy J. Carver Charitable Trust.
10 Nov 2021
Nov. 10, 2021 12:16 UTC
MADISON, Wis.--(BUSINESS WIRE)-- Imbed Biosciences, Inc. (Imbed) announced today that it has been awarded a contract for $1,999,481 by the U.S. Army Medical Research and Development Command’s (USAMRDC) Military Infectious Diseases Research Program (MIDRP) to accelerate clinical development of an antibiofilm version of its next-generation Microlyte® Matrix wound dressing that can kill bacteria hidden in biofilms. The contract was awarded through Medical Technology Enterprise Consortium (MTEC) for prototype solutions that prevent combat wound infections following blast injuries and burns.
This press release features multimedia. View the full release here:
Imbed Biosciences is at the forefront of the development of advanced wound care and surgical products, including those to support members of America's armed services. (Photo: Business Wire)
Combat wound infections are a major risk to warfighter survivability and can delay their return to active duty, posing a significant burden to the Army Health System. Research has shown that greater than 30% of all combat wounds become infected. That percentage is expected to rise in a prolonged field care environment.
This competitive award was made in response to a solicitation from the U.S. Army seeking prototype solutions that prevent warfighter wound infections close to the point of injury without requiring evacuation to higher roles of care, and that enable speedy return of warfighters to duty. The proposed solution will be part of a system to provide an adequate response to traumatic penetrating combat injuries.
“Combat wounds are contaminated with bacteria that start forming biofilms within hours of injury and can lead to failure of treatment, septic shock, and death”, said Ankit Agarwal, co-founder and CEO of the company. “An advanced version of our FDA-cleared Microlyte® Matrix wound dressing kills bacteria hidden in biofilms. The new matrix is ultrathin, bioresorbable, provides a template for cell growth, and can prevent biofilm infections in wounds for several days. This award will fund a prospective human clinical trial of the novel antibiofilm matrix on donor site wounds in patients in need of autologous skin grafts. We are honored to develop this advanced wound matrix for maximizing the readiness and performance of our warfighters in the field.”
About MIDRP:
USAMRDC's MIDRP is one of the six major core research program areas that lead the planning and programming for Army and Defense Health Program research portfolios. As such, MIDRP oversees for DOD a world class requirements-driven infectious diseases Science and Technology program. More information at .
About MTEC:
MTEC is a non-profit enterprise partnership in collaboration with industry and academia to facilitate biomedical research and development activities in cooperation with USAMRDC for U.S. military personnel’s health. For more information, visit mtec-sc.org.
About Imbed Biosciences, Inc.
Imbed is a growth stage privately held biotech company registered with FDA as a medical device manufacturer with an ISO 13485 certified quality management system. The company has a portfolio of products on the market and in development to combat local pain and infections in complex wounds using its patented Microlyte® Matrix technology platform. The research is funded in part by USAMRDC’s OTA Delivery Order #W81XWH-21-9-0007. For more information, visit .
100 Deals associated with Military Infectious Diseases Research Program (MIDRP)
Login to view more data
100 Translational Medicine associated with Military Infectious Diseases Research Program (MIDRP)
Login to view more data
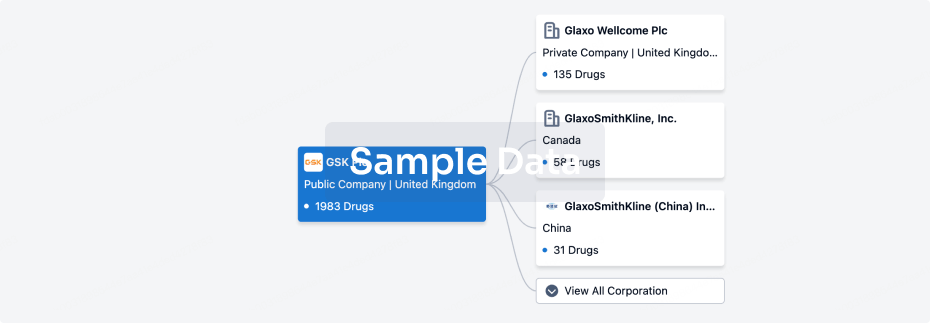
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 22 Apr 2025
The statistics for drugs in the Pipeline is the current organization and its subsidiaries are counted as organizations,Early Phase 1 is incorporated into Phase 1, Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3
Other
2
Login to view more data
Current Projects
| Drug(Targets) | Indications | Global Highest Phase |
|---|---|---|
NMRC-MV-Ad-PfC(U.S. Army Medical Research and Development Command) | Malaria, Falciparum More | Pending |
Malaria vaccine(GenVec, Inc.) | Malaria, Falciparum More | Pending |
Login to view more data
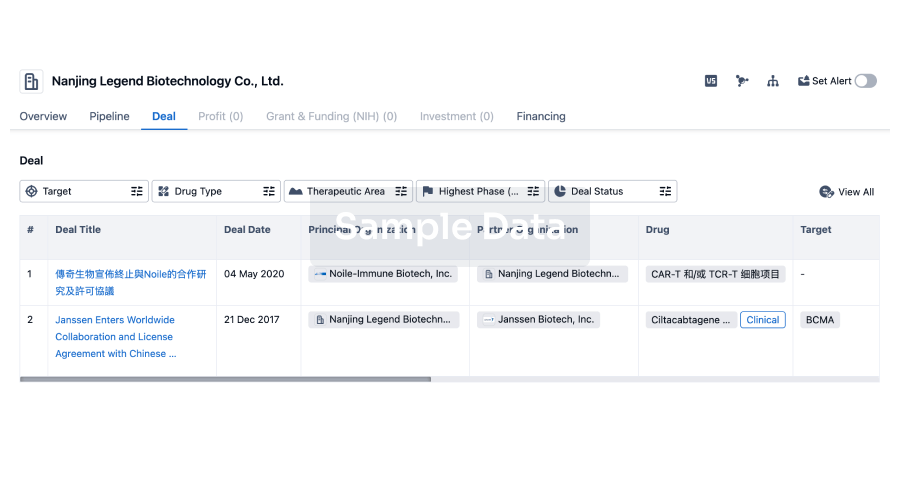
Deal
Boost your decision using our deal data.
login
or
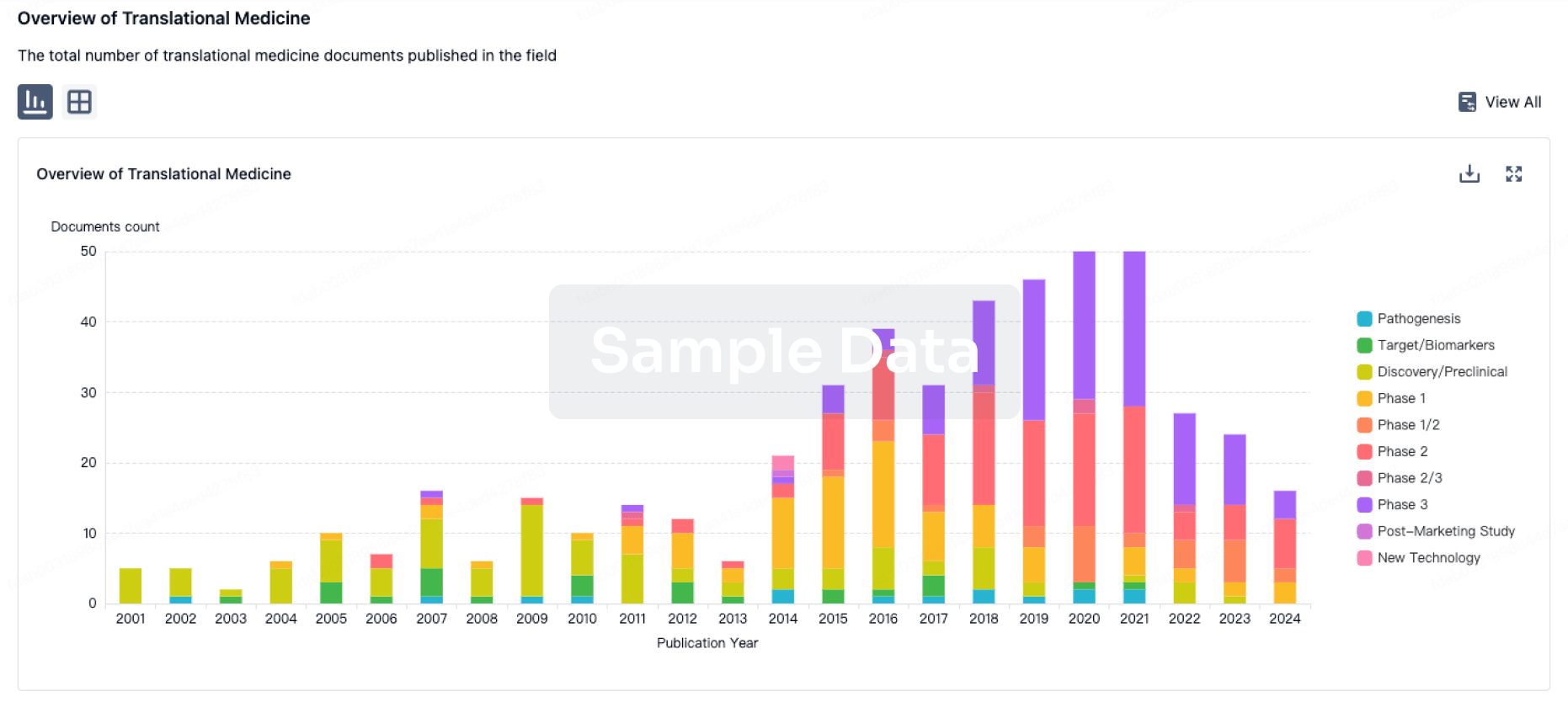
Translational Medicine
Boost your research with our translational medicine data.
login
or
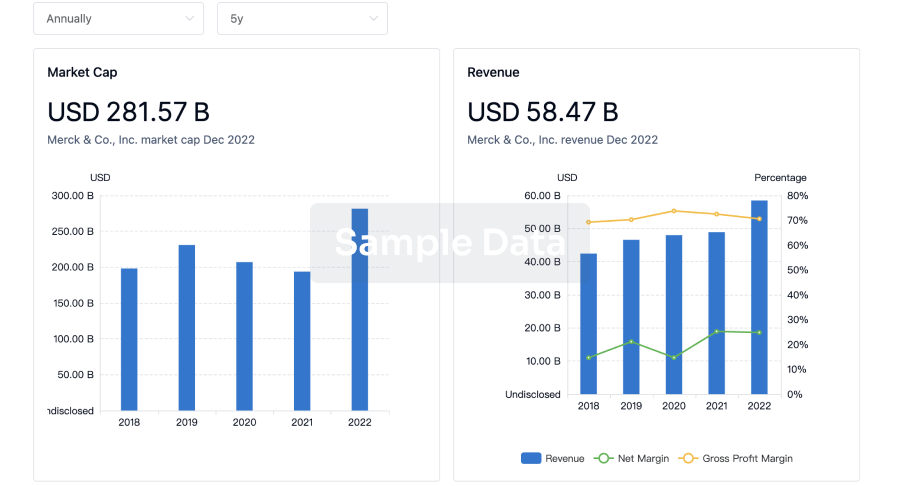
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
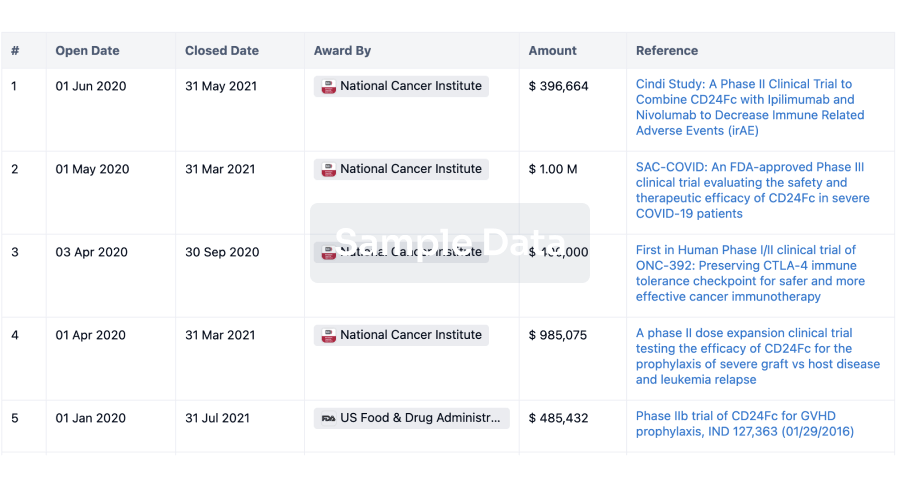
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
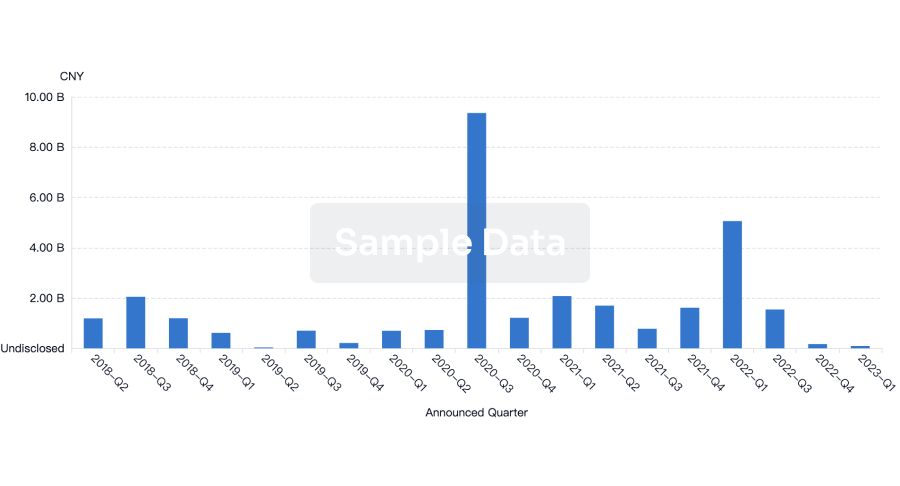
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
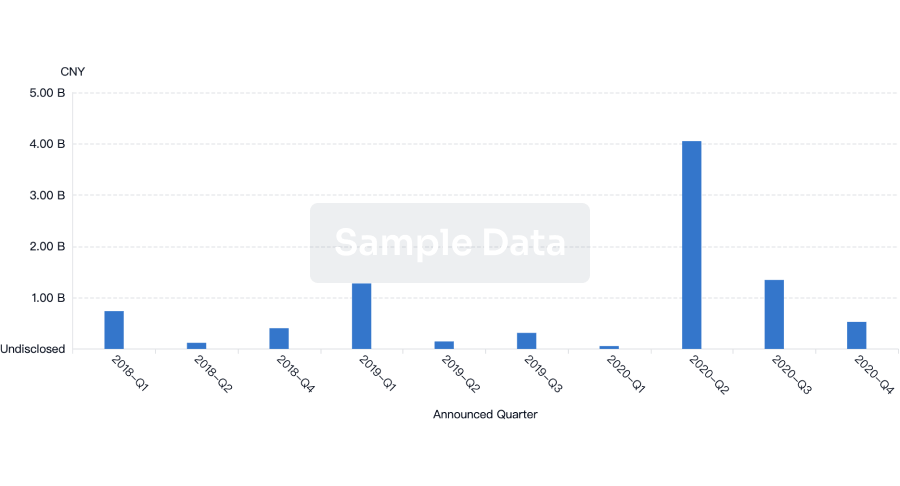
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
Chat with Hiro
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free

